Migraine Treatment Guidelines
Learn effective Migraine Treatment Guidelines to relieve debilitating headaches and improve your quality of life.


What is a migraine?
A migraine is a neurological condition characterized by recurrent, moderate to severe headaches, often accompanied by other symptoms such as nausea, vomiting, and sensitivity to light and sound. These headaches typically last from a few hours to several days, significantly impacting daily functioning. One distinct subtype is menstrual migraine, occurring in conjunction with the menstrual cycle in some individuals. Migraines can manifest as unilateral headaches and may be associated with aura—transient neurological symptoms preceding the headache phase.
Preventive treatments are available for individuals experiencing frequent or severe attacks, aiming to reduce the frequency and severity of migraines. Acute medications, such as triptans or combination analgesics, provide relief during migraine episodes. However, uncontrolled hypertension or other medical conditions may necessitate caution or alternative treatment approaches. Clinical practice guidelines, including those developed by the Canadian Headache Society, offer evidence-based recommendations for migraine management, ensuring optimal care for individuals with this debilitating condition.
As research advances, the treatment of migraine is continually emerging, often validated through rigorous randomized controlled trials. Ultimately, understanding the complexity of migraines and optimizing treatment approaches can significantly alleviate migraine-related disability and improve the quality of life for those affected.
Types
Migraines are complex neurological conditions that affect millions worldwide, often causing debilitating symptoms that significantly impact daily life. Understanding the different types of migraines is crucial for proper diagnosis and treatment of migraine. Here are various types of migraines, each with unique characteristics and management approaches:
- Migraine with aura: This type involves sensory disturbances or visual changes known as aura, preceding or during the migraine attack, characterized by seeing flashing lights, blind spots, or tingling sensations.
- Migraine without aura: Migraines without aura occur without the sensory disturbances seen in migraine with aura, characterized by moderate to severe pulsating headaches, often accompanied by nausea, vomiting, and sensitivity to light and sound.
- Migraines in children (abdominal migraine): Children may experience migraines with symptoms like abdominal pain, nausea, and vomiting instead of headache.
- Chronic migraine (acute migraine): Chronic migraines involve experiencing headaches on 15 or more days per month for at least three months, with at least eight of those days meeting criteria for migraine.
- Hemiplegic migraine: This rare type of migraine causes temporary paralysis or weakness on one side of the body, along with other migraine symptoms.
- Menstrual migraine: Some women experience migraines that are closely linked to their menstrual cycle, occurring before, during, or after menstruation.
- Migraine without headache (silent migraine): Silent migraines present with aura symptoms but without the headache phase.
- Retinal migraine (ocular migraine): Retinal migraines cause temporary visual disturbances or blindness in one eye, often preceding the headache phase.
- Status migrainosus: This is a severe and prolonged migraine attack lasting more than 72 hours, despite treatment.
Each type of migraine requires tailored approaches for acute and preventive treatment to manage symptoms and improve quality of life effectively.
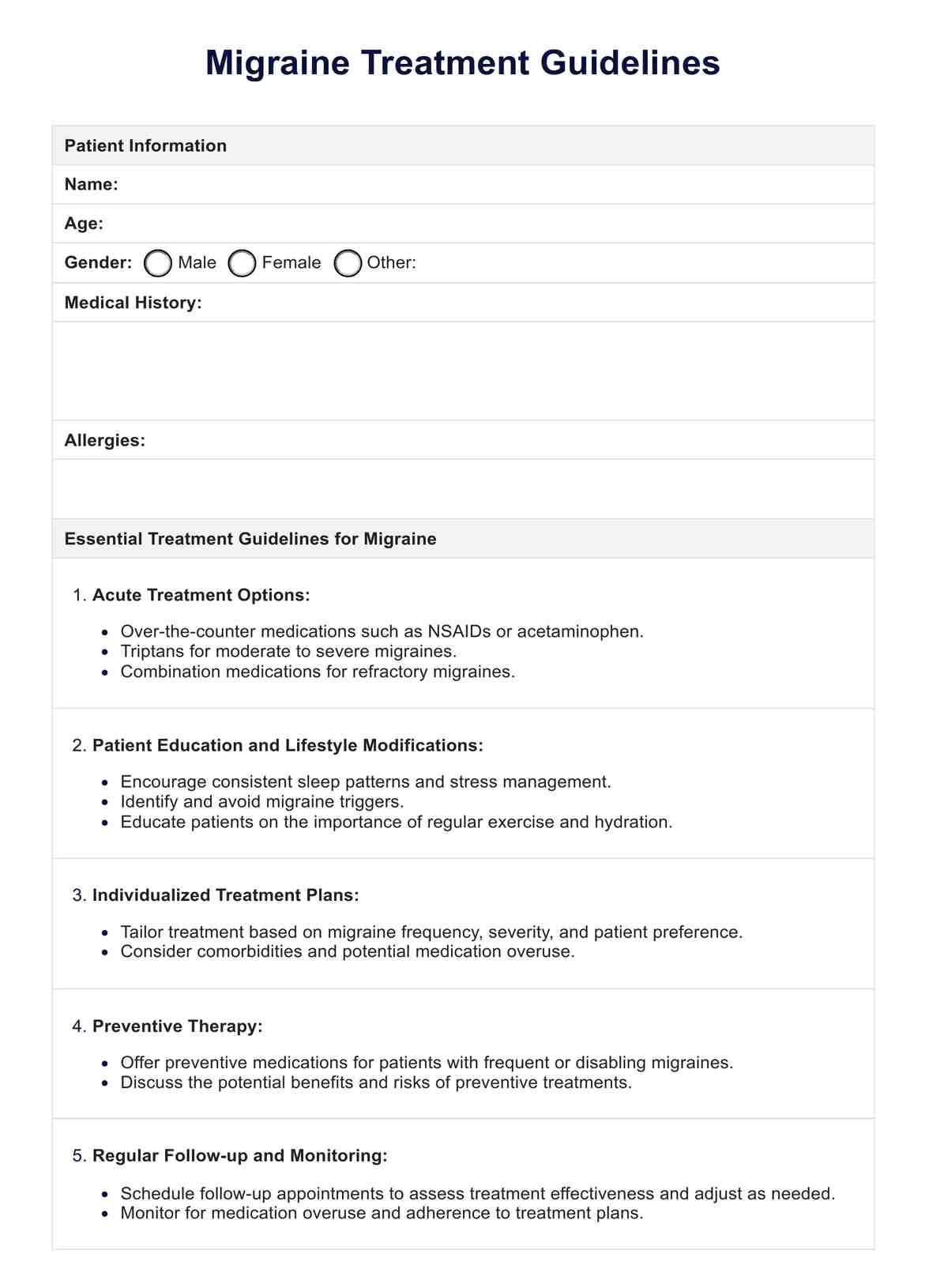
Migraine Treatment Guidelines Template
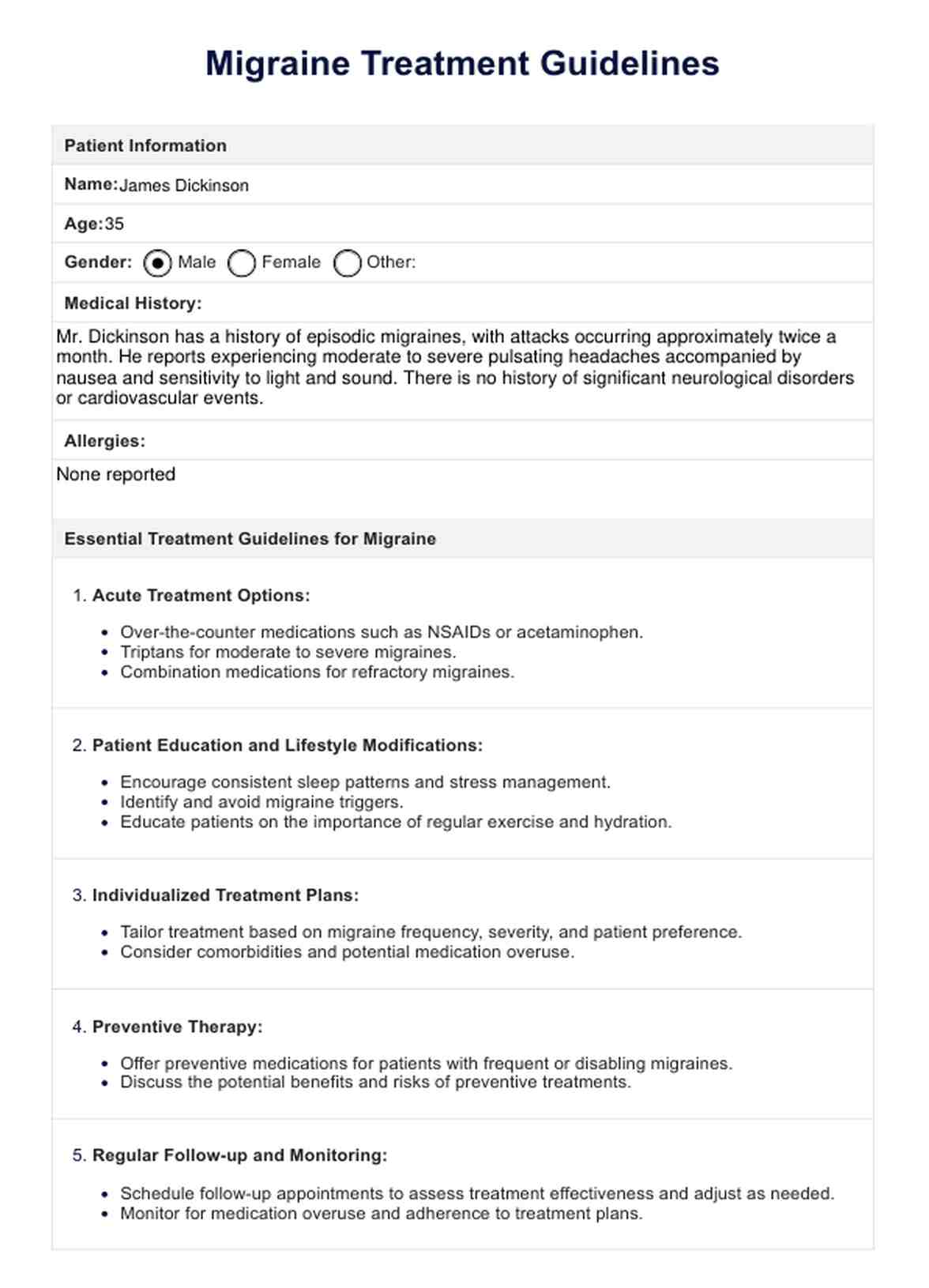
Migraine Treatment Guidelines Example
Diagnosing migraine attacks
According to the American Headache Society (2016), diagnosing migraine attacks involves thorough clinical evaluation based on established criteria. Healthcare providers assess symptoms, frequency, and duration to differentiate between episodic and chronic migraine. AHS emphasizes the importance of considering comorbidities like coronary artery disease and cardiovascular risk factors during evaluation. Diagnostic procedures may include reviewing medical history, conducting physical exams, and, if necessary, ordering imaging studies.
Additionally, AHS suggests keeping an accurate headache diary to track symptoms and identify patterns. Proper diagnosis guides the selection of acute medications and episodic migraine prevention strategies, ensuring effective management and improved quality of life for individuals with migraines.
What is included in the treatment guidelines for migraine?
The treatment of migraines involves a comprehensive approach to alleviate symptoms, prevent future attacks, and improve the quality of life for individuals affected. These guidelines, compiled from reputable sources including the American Headache Society and American Academy of Family Physicians, offer essential recommendations for healthcare providers:
- Acute treatment options:
- Over-the-counter medications such as NSAIDs or acetaminophen.
- Triptans for moderate to severe migraines.
- Combination medications for refractory migraines.
- Patient education and lifestyle modifications:
- Encourage consistent sleep patterns and stress management.
- Identify and avoid migraine triggers.
- Educate patients on the importance of regular exercise and hydration.
- Individualized treatment plans:
- Tailor treatment based on migraine frequency, severity, and patient preference.
- Consider comorbidity and potential medication overuse headache.
- Preventive therapy:
- Offer preventive medications for patients with frequent or disabling migraines.
- Discuss the potential benefits and risks of preventive treatments.
- Regular follow-up and monitoring:
- Schedule follow-up appointments to assess treatment effectiveness and adjust as needed.
- Monitor for medication overuse and adherence to treatment plans.
For further details and evidence-based recommendations, refer to the sources provided by the American Headache Society and American Academy of Family Physicians.
How does the template work?
Healthcare providers use this template to gather essential patient information, diagnose migraines accurately, and recommend appropriate treatments. Here's a breakdown of the process:
Step 1: Patient information collection
Healthcare providers gather essential patient details, including their name, age, gender, medical history, and any known allergies. This step ensures a personalized approach to migraine management.
Step 2: Diagnostic methods and tests
The template outlines various diagnostic approaches, such as clinical evaluation, physical examination, and headache diaries. These tools help assess the severity and frequency of migraine attacks to guide treatment decisions.
Step 3: Recommended/common treatments
Based on the patient's clinical presentation, the template recommends acute and preventive migraine treatments. This may include medications, lifestyle modifications, and preventive therapies to reduce frequency and severity.
Step 4: Migraine-related ICD and/or CPT codes
The template includes relevant codes for migraine-related diagnoses and procedures to ensure accurate documentation and billing. This helps streamline coding and reimbursement processes for healthcare services.
Step 5: Additional comments
Healthcare providers can add personalized comments or recommendations based on clinical judgment and patient preferences. This section further clarifies treatment plans and addresses any specific concerns.
Benefits of having treatment guidelines for migraines
Established migraine treatment guidelines facilitate standardized care, improve patient outcomes, reduce healthcare costs, enhance physician confidence, and promote ongoing education and training in migraine management. Here are its benefits:
- Standardized care: Treatment guidelines provide a standardized approach for healthcare providers to diagnose and manage migraines effectively, ensuring consistency and quality of care across different healthcare settings.
- Improved patient outcomes: By following evidence-based guidelines, healthcare providers can optimize treatment strategies, leading to better symptom management, reduced migraine commonness, and improved patient satisfaction and quality of life.
- Reduction of Healthcare costs: Treatment guidelines help streamline healthcare delivery by promoting appropriate, cost-effective interventions. By minimizing unnecessary diagnostic tests and treatments, guidelines contribute to healthcare cost containment without compromising patient care.
- Enhanced Physician Confidence: Guidelines serve as a valuable resource for healthcare providers, offering evidence-based recommendations and treatment algorithms. This helps increase physician confidence in diagnosing and managing migraines, leading to more efficient and effective patient care.
- Education and training: Migraine treatment guidelines serve as educational tools for healthcare professionals, providing valuable insights into current best practices and emerging treatments. They help disseminate knowledge and promote continuous learning, ultimately improving the quality of care for patients with migraines.
Also, you can use the Clinical Evaluation Template to assess patient health and diagnose conditions accurately. To track and manage headache symptoms, the Headache Diary Template is a valuable tool for documenting frequency, intensity, and potential triggers. Combining these templates can enhance your diagnostic process and patient care. Regular use of both tools can lead to more effective treatment plans and improved patient outcomes.
Treatment options for migraine attacks
Here are some treatment options for migraine:
- Over-the-counter medications: Over-the-counter (OTC) medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for mild to moderate migraine attacks. Naproxen Sodium, for instance, helps alleviate pain and inflammation associated with migraines. Its purpose is to provide quick relief from migraine symptoms and improve patient comfort during an attack.
- Prescription triptans: Triptans are a class of prescription medications specifically designed to treat migraine attacks. They work by narrowing blood vessels and blocking pain pathways in the brain. Sumatriptan, for example, is highly effective in relieving migraine symptoms, including severe headache and nausea. Its purpose is to provide fast and targeted relief from acute migraine attacks, helping patients resume normal activities sooner.
- Combination medications: Combination medications, such as Excedrin Migraine, contain acetaminophen, aspirin, and caffeine. These medications work synergistically to provide comprehensive relief from migraine symptoms. The purpose of combination medications is to address multiple symptoms simultaneously, including headache pain, nausea, and sensitivity to light and sound, offering convenience and effectiveness for patients experiencing migraines.
- Anti-nausea medications (e.g., Metoclopramide): Severe nausea is a common and debilitating symptom of migraines. Anti-nausea medications like metoclopramide can help alleviate nausea and vomiting during migraine attacks. By targeting nausea directly, these medications improve patient comfort and reduce the overall impact of migraines on daily functioning.
- Alternative therapies (e.g., acupuncture or niofeedback): In addition to conventional medications, alternative therapies such as acupuncture or biofeedback may offer relief for some migraine sufferers. These approaches focus on holistic methods to reduce migraine frequency and severity, addressing underlying factors such as stress and muscle tension.
References
Silberstein , S., JR, S., & FG, F. (2016). Migraine diagnosis and treatment. https://americanheadachesociety.org/wp-content/uploads/2018/05/NAP_for_Web_-_Acute_Treatment_of_Migraine-1.pdf
Mayans, L., & Walling, A. (2018). Acute Migraine Headache: Treatment Strategies. American Family Physician, 97(4), 243–251. https://www.aafp.org/pubs/afp/issues/2018/0215/p243.html#general-treatment-principles
Commonly asked questions
Migraines typically present with moderate to severe headaches, often accompanied by nausea, vomiting, and sensitivity to light and sound. Some individuals may experience an aura—transient neurological symptoms—before the onset of the headache.
Migraines are neurological conditions characterized by recurrent, often disabling headaches, whereas tension headaches are generally milder and result from muscle tension or stress.
Diagnosis of migraines is primarily based on clinical evaluation, including a thorough assessment of symptoms, medical history, and physical examination. Additional tests, such as imaging studies, may be conducted to rule out other potential causes of headaches.