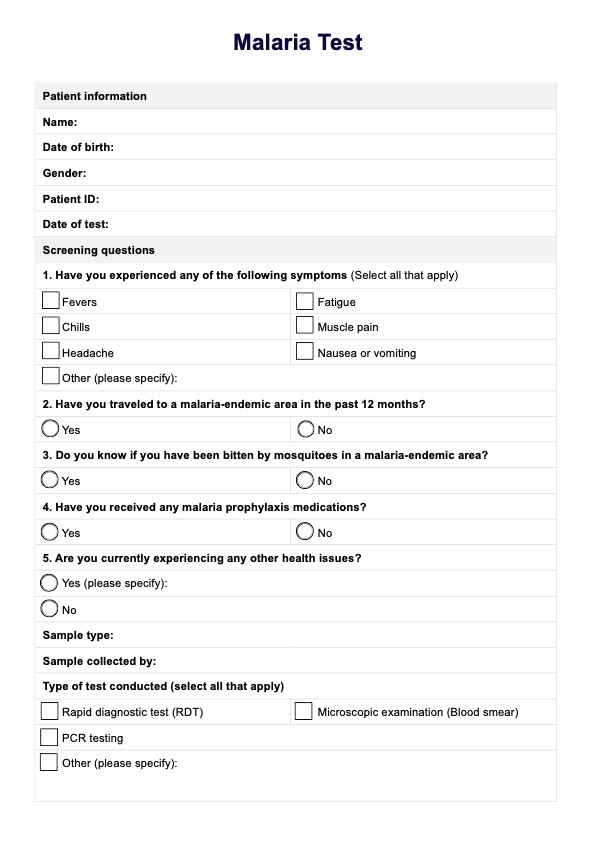
To check for malaria, a healthcare provider will typically order a blood test, such as an RDT or microscopic examination, to detect the presence of malaria parasites. Symptoms like fever, chills, and fatigue should prompt immediate testing for accurate malaria diagnosis.
Malaria
Discover a comprehensive guide to Malaria Tests, including examples and Carepatron's free PDF download. Learn more about how malaria is diagnosed and treated.
Use Template
Malaria Template
Commonly asked questions
Yes, malaria can be detected in blood tests, which identify malaria parasites in the bloodstream. Tests like malaria microscopy and PCR testing are effective in confirming the diagnosis.
A positive malaria report indicates an active malaria infection, showing that malaria antigens are present in the blood. This finding requires prompt treatment with antimalarial medications to manage and control the disease.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











