Lupus Anticoagulant Test
Unlock the mysteries of the Lupus Anticoagulant Test with our comprehensive guide—your go-to resource for understanding, testing, and implications.


What does the Lupus Anticoagulant Test measure?
Despite its name, the Lupus Anticoagulant (LA) test does not measure anticoagulant activity. Instead, it is a test that detects the presence of antibodies that interfere with the normal clotting process. Lupus anticoagulant is one type of antiphospholipid antibody.
Here's a more detailed explanation of what the test measures:
- Antiphospholipid antibodies: The test primarily looks for lupus anticoagulant, which targets phospholipids. Phospholipids are components of cell membranes, and the presence of antibodies against them can lead to abnormal clotting.
- Clotting time: The test measures the time it takes for blood to clot. Lupus anticoagulant interferes with the normal clotting process, prolonging the clotting time in the laboratory setting.
- Russell viper venom time (RVVT): In some cases, a specific method called Dilute Russell Viper Venom Time (dRVVT) is used to detect lupus anticoagulants. This test involves adding a dilute form of Russell viper venom to the blood sample to assess clotting time.
Activated partial thromboplastin time (aPTT): The Lupus Anticoagulant Test is often part of the activated partial thromboplastin time (aPTT) test. The aPTT measures the time it takes for blood to clot in a test tube and is used to evaluate the intrinsic pathway of the clotting cascade. Lupus anticoagulant can prolong the aPTT.
Lupus Anticoagulant Test Template
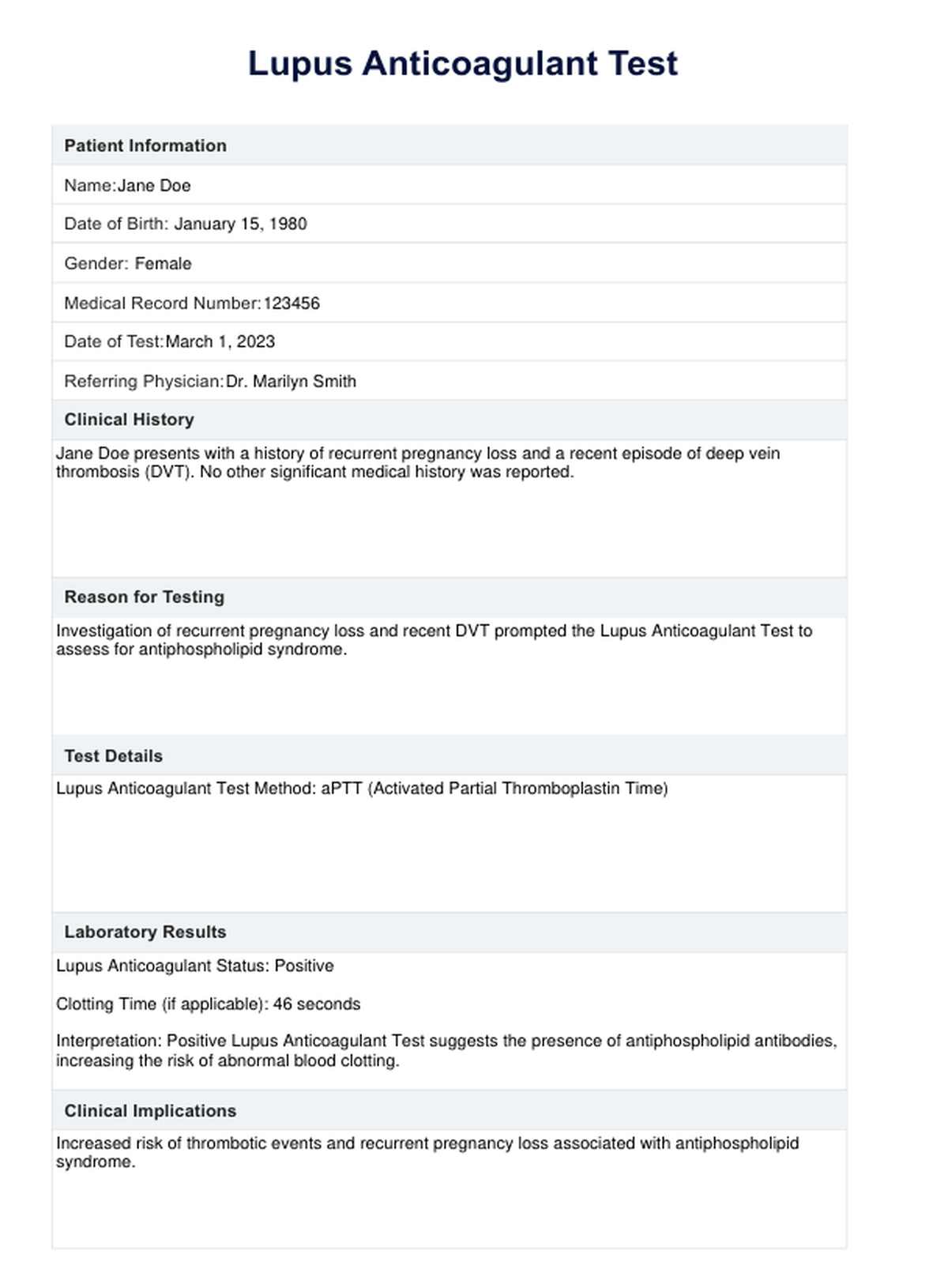
Lupus Anticoagulant Test Example
Other blood tests
When evaluating a patient for Lupus Anticoagulant (LA) or antiphospholipid syndrome (APS), healthcare professionals may order a combination of blood tests to provide a comprehensive assessment. In addition to the Lupus Anticoagulant Test, some other relevant tests for APS and related conditions include:
- Anticardiolipin antibodies (ACA): These antibodies target a type of lipid called cardiolipin. Elevated levels may be associated with increased blood clotting risk.
- Anti-beta-2 glycoprotein I antibodies: Similar to anticardiolipin antibodies, these antibodies are associated with APS and may contribute to abnormal blood clotting.
- Antiphospholipid antibody panel: This may include tests for lupus anticoagulant, anticardiolipin antibodies, and anti-beta-2 glycoprotein I antibodies, providing a more comprehensive evaluation for APS.
- Activated partial thromboplastin time (aPTT): This test is often used with the test and can be prolonged in the presence of lupus anticoagulant.
- Prothrombin time (PT): It measures the time it takes for blood to clot and may be used to assess the extrinsic coagulation pathway.
- Thrombin time: Evaluates the conversion of fibrinogen to fibrin and can help assess coagulation disorders.
- Complete blood count (CBC): Helps assess for anemia, thrombocytopenia, or other blood abnormalities that may be associated with APS.
- D-dimer: Elevated levels of D-dimer may indicate the presence of blood clots, and this test can be used in conjunction with other tests to assess clotting activity.
Healthcare professionals should interpret these tests in the context of the patient's clinical presentation and medical history. The combination of these tests helps healthcare providers diagnose and manage conditions related to abnormal blood clotting, such as APS.
If lupus anticoagulant antibodies or other antiphospholipid antibodies are detected, additional testing and evaluation may be required to determine the appropriate course of treatment and management.
What do the test results mean?
Interpreting Lupus Anticoagulant Test results involves considering the specific laboratory findings in the context of the patient's clinical history and other test results. Here's a general guideline for interpreting test results:
- Positive: A positive result on the test indicates the presence of lupus anticoagulant, an antibody that interferes with normal blood clotting. This result is associated with an increased risk of abnormal blood clotting, which can lead to conditions such as deep vein thrombosis (DVT), pulmonary embolism, stroke, and recurrent miscarriages.
- Negative: A negative result suggests the absence of lupus anticoagulant in the blood. However, a negative impact does not rule out the possibility of other antiphospholipid antibodies being present, and further testing (such as anticardiolipin antibodies and anti-beta-2 glycoprotein I antibodies) may be needed for a more comprehensive evaluation.
- Indeterminate: In some cases, results may be indeterminate, requiring additional testing or a repeat of the test for clarification.
- Clinical correlation: The interpretation should always involve clinical correlation with the patient's symptoms and medical history, regardless of the specific result. Positive results, especially when accompanied by clinical signs, may lead to an antiphospholipid syndrome (APS) diagnosis.
Follow-up testing and consultation: Positive results often warrant further testing and consultation with specialists, such as hematologists. Follow-up testing may include additional assessments of the clotting system and other antiphospholipid antibodies.
What might affect the test results?
Several factors can influence Lupus Anticoagulant Test results. Healthcare providers must know these factors when interpreting results and making clinical decisions. Here are some factors that might affect the accuracy of the test:
- Anticoagulant medications: Anticoagulant medications, such as heparin or warfarin, can affect test results. It's essential to consider the timing of the last dose before performing the test.
- Presence of antiphospholipid antibodies: The Lupus Anticoagulant Test is specific to lupus anticoagulant, but there are other antiphospholipid antibodies, such as anticardiolipin antibodies and anti-beta-2 glycoprotein I antibodies. The presence of these antibodies can influence test results and may be evaluated alongside the test.
- Certain medical conditions: Infections, inflammation, and liver disease can affect the test results.
- Pregnancy: Testing can be influenced by pregnancy, and results may vary during different stages of gestation.
- Technical issues in the laboratory: Improper handling of blood samples, incorrect laboratory techniques, or equipment malfunctions can affect test results.
- Other medications: Some medications, including certain antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs), may interfere with coagulation test results.
- Age and gender: Some studies suggest that lupus anticoagulant prevalence may be influenced by age and gender, with a higher prevalence in specific populations.
- Underlying medical conditions: Autoimmune diseases, such as systemic lupus erythematosus (SLE), can affect test results.
- Smoking: Smoking has been associated with changes in blood coagulation parameters and may influence test results.
Blood-thinning medications
Blood-thinning medications, also known as anticoagulants or antiplatelet drugs, are prescribed to reduce the risk of blood clots. These medications interfere with the body's normal blood clotting process. They are commonly used to prevent blood clots or treat conditions such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and certain heart conditions. Here are some common blood-thinning medications:
Warfarin (coumadin)
Warfarin is an oral anticoagulant that interferes with the synthesis of clotting factors in the liver. It requires regular monitoring of the International Normalized Ratio (INR) to ensure therapeutic levels. Warfarin interacts with many foods and medications; dosages may need frequent adjustments.
Some common foods and drinks that might interact with warfarin include cranberries or cranberry juice, grapefruit, alcohol, garlic, and black licorice.
Warfarin also interacts with many supplements, such as feverfew, fish oil/omega-3, three fatty acids, garlic, ginger, ginkgo, turmeric/curcumin, and vitamin E. It's important to speak to your doctor or nurse before changing what you eat or taking any supplements while on warfarin.
Heparin
Heparin is an anticoagulant often used in hospitals and administered through injections or intravenous. It acts more rapidly than warfarin and is used in acute situations, such as during hospitalization or surgery.
Monitoring activated partial thromboplastin time (aPTT) is required to adjust the dosage. The initial dose of heparin is at least 150 units/kg; 300 units/kg is frequently used for procedures estimated to last less than 60 minutes or 400 units/kg for methods estimated to last more than 60 minutes.
Low molecular weight heparins (LMWHs)
Low molecular weight heparins (LMWHs) are a class of anticoagulants used therapeutically for treating thrombosis and prophylaxis in situations that lead to a high risk of thrombosis. Examples include Enoxaparin (Lovenox) and dalteparin (Fragmin).
LMWHs have a more predictable anticoagulant effect and often do not require frequent monitoring. LMWHs can be self-administered at home via subcutaneous injection, reducing or eliminating hospital stays. LMWHs are recommended over unfractionated heparin (UFH) for patients with massive pulmonary embolism and initial treatment.
Direct oral anticoagulants (DOACs)
Direct oral anticoagulants (DOACs) are a newer class of medications that include apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban (Savaysa). These medications are taken orally and have a more predictable anticoagulant effect. Monitoring requirements are generally less frequent compared to warfarin.
DOACs have several advantages over traditional vitamin K antagonists (VKAs) like warfarin, such as fewer monitoring requirements, less frequent follow-up, and more immediate drug onset and offset. However, in specific clinical situations and for particular patient populations, testing may be helpful for patient management.
Antiplatelet medications
Antiplatelet medications, such as aspirin, clopidogrel (Plavix), and prasugrel (Effient), are commonly used to prevent and treat conditions like heart attack, stroke, and coronary artery disease. They work by preventing blood clots from forming, thus decreasing the body's ability to form clots.
Aspirin is the most commonly used antiplatelet drug, and other examples include clopidogrel, ticagrelor, and prasugrel. These medications primarily inhibit platelet aggregation and are often prescribed to individuals with a history of cardiac events or those at high risk of developing blood clots.
Plasma exchange
Plasma exchange, also known as therapeutic plasma exchange (TPE) or plasmapheresis, is a procedure that can be used to treat autoimmune diseases, including those associated with antiphospholipid syndrome and lupus anticoagulant. TPE's primary mechanisms of action include removing circulating autoantibodies, immune complexes, complement components, cytokines, and adhesion molecules in blood cells and sensitization of antibody-producing cells to immunosuppressant agents.
Plasma exchange can be a part of the treatment approach for conditions associated with lupus anticoagulant and antiphospholipid syndrome, particularly in cases of lupus anticoagulant panel well-refractory disease or concurrent lupus nephritis and antiphospholipid syndrome. It is used to remove disease-causing proteins and antibodies from the plasma, and it has been reported to contribute to the improvement of renal function and the undetectability of lupus anticoagulant in some cases.
Does this test pose any risks?
The Lupus Anticoagulant Test, like any medical test, carries some potential risks and considerations, though they are generally minimal. Here are some factors to consider:
- Bleeding and bruising: Blood tests involve the insertion of a needle to collect a blood sample. While bleeding and bruising at the puncture site are usually minor, individuals who have a bleeding disorder or are taking anticoagulant medications may be at a slightly higher risk.
- Pain or discomfort: Some individuals may experience mild pain or discomfort during the blood draw. This can vary depending on factors such as individual pain tolerance and the skill of the person performing the test.
- Fainting or dizziness: Some people may feel lightheaded, dizzy, or faint during or after a blood draw. This is generally temporary and can be managed by staying well-hydrated and informing the healthcare provider if you have a history of such reactions.
- Infection at the puncture site: While rare, there is a minimal risk of disease at the puncture site. Healthcare providers take precautions to minimize this risk by using sterile equipment and following proper procedures.
- False positives or negatives: Interpretation of test results can be complex, and false positives or negatives may occur. Other factors, such as medications and certain medical conditions, can influence test results.
- Emotional distress: For some individuals, the process of undergoing medical tests can be emotionally distressing. Communicating concerns or anxieties with the healthcare provider ensures a more comfortable experience.
Discontinuing other medications
Discontinuing medications, especially those related to anticoagulation or other essential medical conditions, should only be done under the guidance and supervision of a healthcare professional. Abruptly stopping certain medications can have severe consequences and may lead to health complications.
If you are considering discontinuing any medications, including anticoagulants or other prescription drugs, it's essential to follow these steps:
- Consult your healthcare provider: Schedule an appointment with your healthcare provider to discuss your concerns and reasons for wanting to discontinue a medication. This may be due to side effects, changes in your health, or other factors.
- Review medical history: Your healthcare provider will review your medical history, including the reasons for starting the medication, its effectiveness, and any potential side effects.
- Assess current health status: Your health status and any existing medical conditions will be considered when evaluating the appropriateness of discontinuing a medication.
- Potential alternatives: If discontinuation is being considered due to side effects or other issues, your healthcare provider may discuss alternative medications or treatment approaches that better suit your needs.
- Gradual tapering (if necessary): Certain medications may require a gradual tapering schedule rather than abrupt discontinuation to prevent withdrawal symptoms or a rebound effect.
Monitoring and follow-up: Your healthcare provider will establish a plan for monitoring your health after discontinuation. This may involve follow-up appointments, additional tests, or ongoing assessments to ensure your well-being.
How can Carepatron help with Lupus Anticoagulant Testing?
Revolutionize Lupus Anticoagulant Testing with Carepatron! Our Lab Values Chart app simplifies lab results tracking within electronic health records, seamlessly connecting with essential services to elevate overall practice efficiency.
Experience the convenience of our Coagulation Factor Test, specifically designed for assessing coagulation disorders, including those linked to testing. Our versatile platform integrates various lab results, ensuring comprehensive, patient-centered care.
Elevate your practice with Carepatron – where efficiency meets excellence in healthcare.

Commonly asked questions
The blood test assesses the presence of lupus anticoagulant, an antibody associated with an increased risk of abnormal blood clotting.
The test is performed to diagnose or monitor conditions such as antiphospholipid syndrome, recurrent thrombosis, and unexplained pregnancy complications.
The test typically involves measuring clotting times, such as activated partial thromboplastin time (aPTT) or dilute Russell Viper Venom Time (dRVVT), before and after adding patient plasma.