It's a series of tests conducted by a healthcare professional to assess the function of the nerves in your legs and feet. This helps diagnose nerve damage, muscle weakness, or other neurological issues.
Lower Extremity Neuro Exam
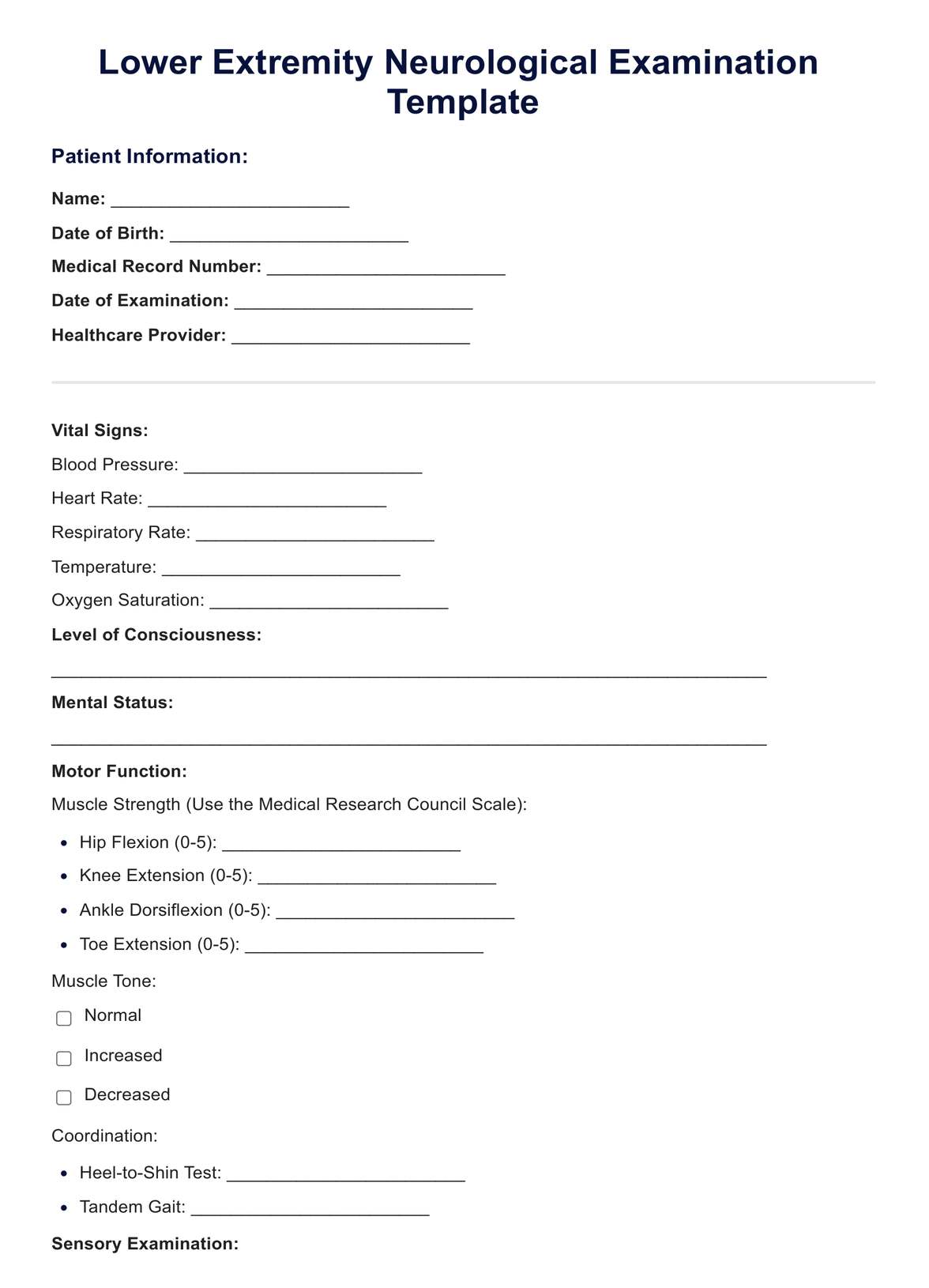
Utilise our comprehensive lower extremity neuro exam to assess motor, sensory, and reflex functions for effective patient care
Use Template
Lower Extremity Neuro Exam Template
Commonly asked questions
You'll typically sit or lie down while the healthcare professional performs tasks like observing, palpation, testing reflexes, sensory testing, and balance and coordination tests.
Early detection and treatment of nerve problems in the legs can prevent complications like muscle weakness, pain, and difficulty walking. This exam helps identify the cause of these issues and guide appropriate treatment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











