Insulin Blood
Get accurate Insulin Blood Test results for diabetes and metabolic health. Learn what your insulin levels mean.


What is an Insulin Blood Test?
An insulin blood test, also known as a serum insulin test, is a medical diagnostic procedure that measures insulin concentration in a person's bloodstream. Insulin is a hormone produced by the pancreas, and its primary function is to regulate glucose (sugar) levels in the blood. This hormone plays a crucial role in maintaining normal blood sugar levels by facilitating glucose uptake into cells, where it can be used for energy or stored for later use.
Healthcare professionals typically order the test to assess the pancreas's functioning and diagnose or monitor various conditions related to blood sugar regulation. It can provide valuable information for individuals with diabetes, hypoglycemia (low blood sugar), or other metabolic disorders.
Additionally, it may be used to evaluate insulin resistance, a condition where the body's cells do not respond effectively to insulin, which is often associated with type 2 diabetes.
The test involves drawing a blood sample, usually from a vein in the arm, which is then sent to a laboratory for analysis. The results indicate the amount of insulin in the blood at a specific moment. Abnormal results, whether high or low insulin levels, can help healthcare providers make informed decisions about treatment plans, medication adjustments, or lifestyle modifications to manage or improve a patient's condition.
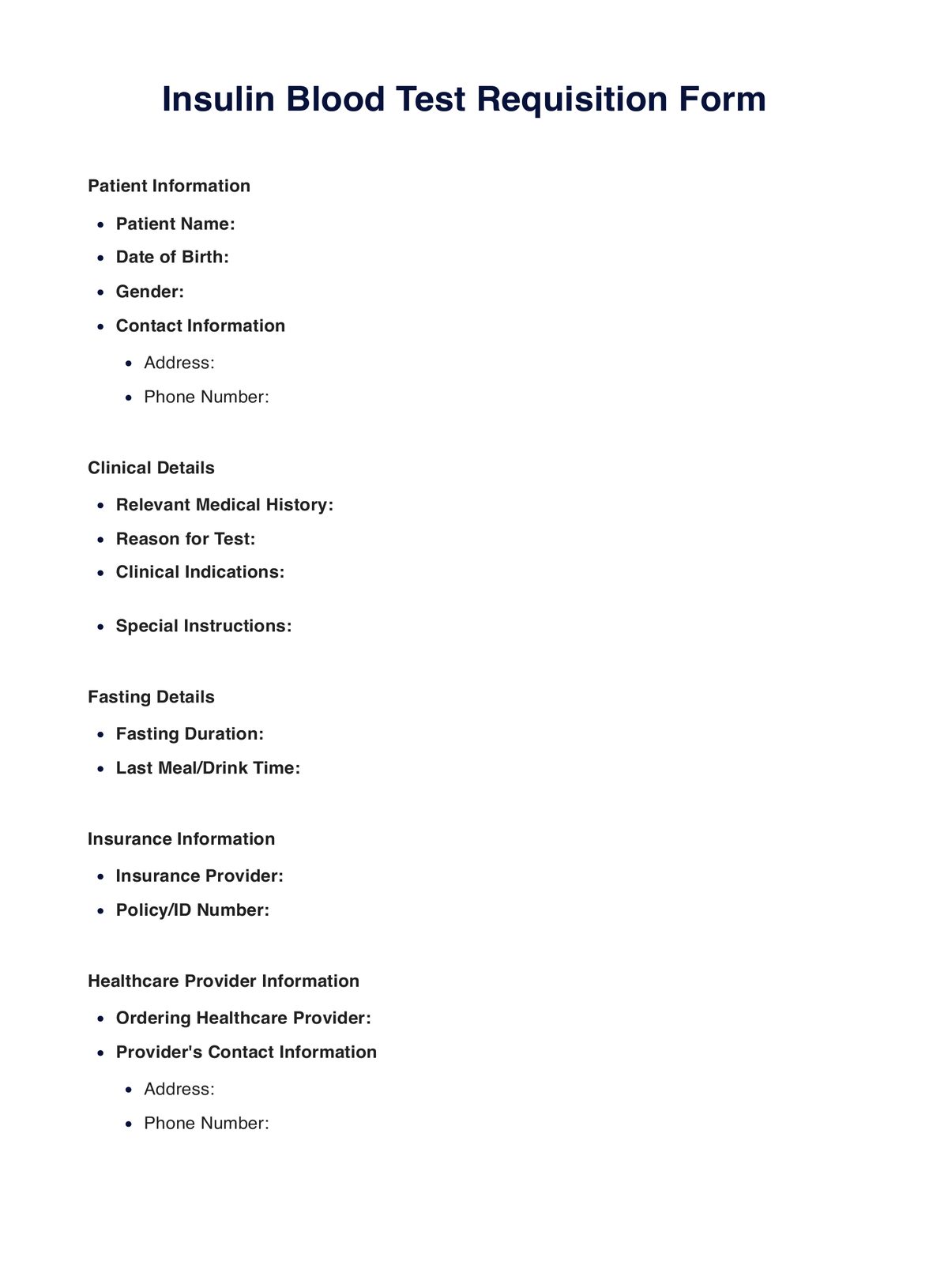
Insulin Blood Template
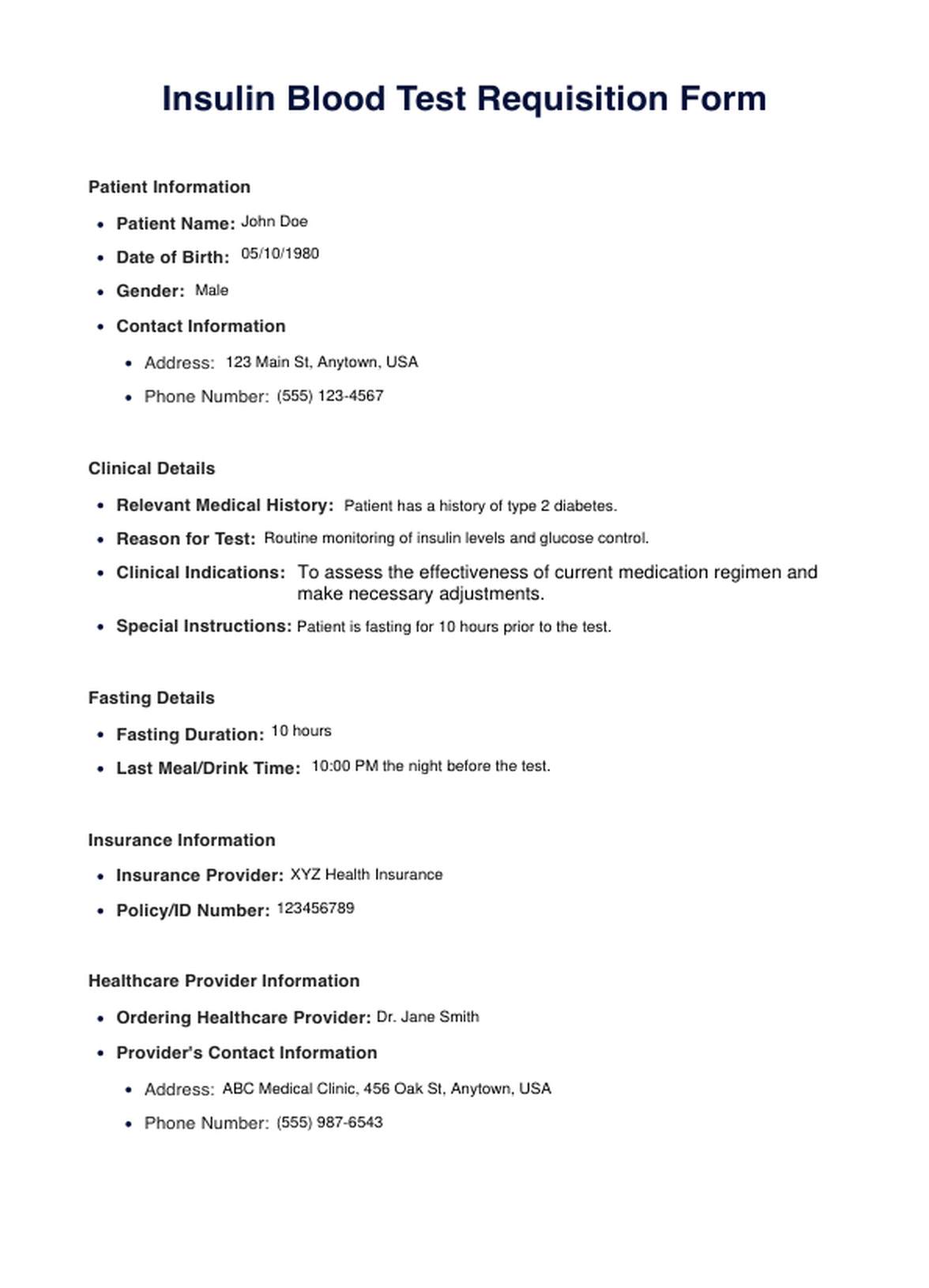
Insulin Blood Example
How Does it Work?
An insulin blood test is a diagnostic procedure that assesses insulin concentration in a person's bloodstream, which plays a pivotal role in regulating blood sugar levels. This test is crucial for individuals with diabetes, hypoglycemia, or other metabolic disorders and for evaluating insulin resistance, often linked to type 2 diabetes. The procedure involves several key steps:
Medical Requisition
To begin, a healthcare provider issues a prescription for the insulin blood test, specifying the need for this assessment.
Fasting Requirement
Patients must typically fast for 8 to 12 hours before the test. Fasting ensures that blood glucose levels are stable and provides accurate insulin measurements.
Lab Visit
Patients visit a laboratory or healthcare facility on the appointed day, presenting the medical requisition.
Blood Sample Collection
Trained phlebotomists or healthcare professionals draw a blood sample, usually from a vein in the patient's arm, using a sterile needle and vial.
Sample Identification
To maintain sample integrity, the collected blood sample is accurately labeled with the patient's name, date of birth, and a unique identification number.
Sample Processing
The blood sample undergoes processing in the laboratory, separating the serum (the liquid component) from cellular components.
Insulin Measurement
Specialized immunoassays are employed to measure the concentration of insulin in the serum.
Result Reporting
The results, typically reported in international units per milliliter (IU/mL) or picomoles per liter (pmol/L), are conveyed to the healthcare provider who ordered the test.
Interpretation
Healthcare providers interpret the results regarding the patient's medical history and overall health. Abnormal insulin levels may indicate specific medical conditions or guide decisions regarding diagnosis and treatment.
The insulin blood test is essential for managing and improving overall health, providing valuable insights into blood sugar regulation and metabolic health.
When would you use this test?
An insulin blood test is a valuable diagnostic tool employed by various healthcare practitioners to assess a patient's insulin levels and, by extension, their metabolic health. This test is particularly appropriate in multiple clinical scenarios and for different medical professionals:
- Diabetes Management: Endocrinologists frequently use insulin blood tests to diagnose and monitor diabetes. They assess the effectiveness of insulin therapy and adjust treatment plans accordingly.
- Insulin Resistance: Endocrinologists employ this test to determine the extent of resistance and guide treatment for patients showing signs of insulin resistance.
- Routine Health Checkups: Primary care physicians may include insulin blood tests as part of regular checkups for patients with risk factors for diabetes, such as obesity, family history, or high blood sugar.
- Unexplained Symptoms: When patients present with unexplained symptoms like excessive thirst or frequent urination, primary care physicians may order this test to investigate underlying causes.
- Pancreatic Disorders: Gastroenterologists use insulin blood tests to evaluate pancreatic function. Abnormal insulin levels may suggest pancreatic disorders, including tumors or pancreatitis.
- Cardiometabolic Risk Assessment: Cardiologists may request this test to assess cardiometabolic risk factors. High insulin levels are associated with increased cardiovascular risk, particularly in patients with insulin resistance.
- Gestational Diabetes: During pregnancy, insulin blood tests help screen for gestational diabetes, a temporary form of diabetes that can develop during pregnancy.
- Dietary Guidance: Nutritionists may recommend insulin blood tests to individuals struggling with weight management, as these tests can uncover underlying issues like insulin resistance that may impede weight loss efforts.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS often experience insulin resistance. Rheumatologists use insulin blood tests to evaluate and manage metabolic concerns in such cases.
- Athlete Assessment: In sports medicine, insulin blood tests can help assess athletes' metabolic health, particularly nutritional needs and performance optimization.
What do the Results Mean?
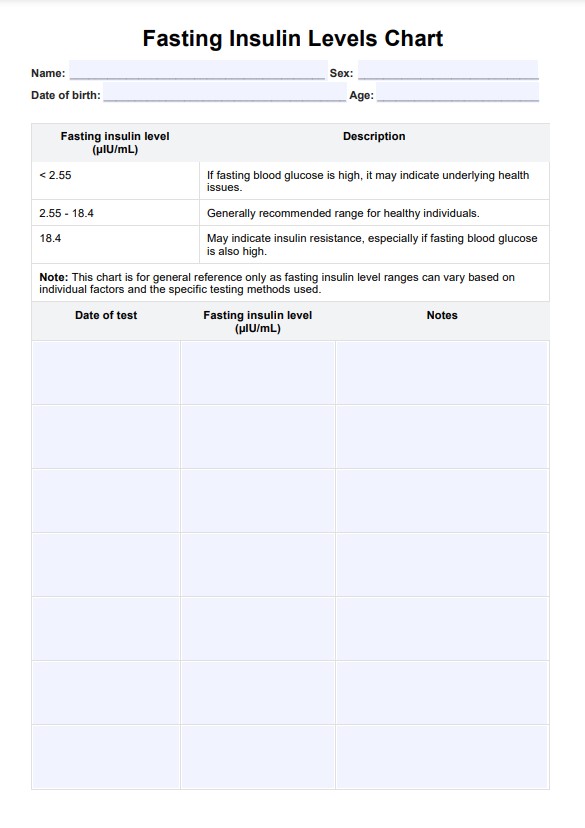
Interpreting the results of an insulin blood test is crucial for understanding a patient's metabolic health and guiding treatment decisions. Here are expected results and their implications:
Normal Insulin Levels
Normal fasting insulin levels typically range from 2 to 25 microinternational units per milliliter (μIU/mL) or 14 to 174 picomoles per liter (pmol/L). In such cases, it suggests the body effectively regulates blood sugar. This is an optimal outcome and indicates good metabolic health.
High Insulin Levels
Elevated insulin levels can signal various conditions:
- Insulin Resistance: High insulin and high blood sugar (glucose) are often seen in insulin-resistant individuals. It implies that the body's cells are not responding well to insulin, possibly leading to type 2 diabetes.
- Prediabetes or Diabetes: High insulin with high blood glucose levels is characteristic of prediabetes or diabetes. This indicates an inability to maintain normal blood sugar levels.
- Polycystic Ovary Syndrome (PCOS): Elevated insulin levels can be linked to PCOS, a condition common in women, often leading to irregular menstrual cycles and insulin resistance.
Low Insulin Levels
Low insulin levels may be seen in certain conditions:
- Type 1 Diabetes: In individuals with type 1 diabetes, insulin production is insufficient or absent, resulting in low insulin levels. These individuals require insulin therapy.
- Hypoglycemia: Low insulin with low blood glucose can indicate hypoglycemia, characterized by abnormally low blood sugar levels, potentially causing dizziness and confusion.
Other Scenarios
- Gestational Diabetes: In pregnant women, elevated fasting insulin levels may indicate gestational diabetes, requiring management during pregnancy.
- Pancreatic Disorders: Abnormal insulin levels could suggest pancreatic disorders, such as tumors or pancreatitis, requiring further evaluation.
Research & Evidence
The history of insulin testing is intimately connected to the discovery of insulin itself. In 1921, Sir Frederick Banting Charles Best and other collaborators isolated and purified insulin for the first time. This groundbreaking discovery paved the way for understanding the hormone's role in blood sugar regulation.
Following the discovery of insulin, research rapidly expanded to understand diabetes better. Scientists conducted numerous studies to explore the link between insulin and diabetes, including type 1 and type 2 diabetes. This research solidified the crucial role of insulin in these conditions.
Over the decades, as technology and medical science progressed, the accuracy and reliability of insulin blood tests improved. Immunoassays, such as enzyme-linked immunosorbent assays (ELISAs), became standard for measuring insulin levels.
Insulin blood tests for diagnosing and monitoring diabetes and related metabolic disorders became a well-established practice. Numerous clinical studies and trials supported the accuracy of these tests, leading to their widespread use in clinical settings.
Insulin blood tests are not only diagnostic but also serve as a critical tool for monitoring the efficacy of insulin therapy in diabetic patients. By regularly measuring insulin levels, healthcare providers can make informed decisions about treatment adjustments.
Research efforts have also expanded to investigate insulin resistance, a condition where the body's cells don't respond effectively to insulin. Studies examining insulin resistance and its association with various health outcomes, including obesity and cardiovascular disease, have further demonstrated the importance of insulin testing.
References
- Buppajarntham, S., MD. (n.d.). Insulin: reference range, interpretation, collection, and panels. https://emedicine.medscape.com/article/2089224-overview?form=fpf
- Connecticut Children’s. (2009, January 23). Blood Test: Insulin - Connecticut Children's. https://www.connecticutchildrens.org/health-library/en/parents/test-insulin/
- Lu, C. M., MD PhD. (2022, November 29). Insulin test - testing.com. Testing.com. https://www.testing.com/tests/insulin/
- Novkovic, B. (2023). Fasting Insulin Test: Normal Range + Low & High Levels. SelfDecode Labs. https://labs.selfdecode.com/blog/fasting-insulin-test/
- Portea, U. K. M. M. D. M. D., & Portea, U. K. M. M. D. M. D. (n.d.). Insulin fasting test - normal range, procedure, results & more. www.portea.com. https://www.portea.com/labs/diagnostic-tests/insulin-fasting-test-225/
- Rosenthal, J. (2022). Understanding your lab work: Fasting insulin test. Knew Health. https://knewhealth.com/understanding-your-lab-work-fasting-insulin-test/
- Yashoda hospitals. (2023, September 21). Yashoda Hospitals. https://www.yashodahospitals.com/diagnostics/insulin-test/
Commonly asked questions
Healthcare providers, including endocrinologists, primary care physicians, and specialists, typically request Insulin Blood Tests.
Insulin Blood Tests are used to diagnose and monitor diabetes, assess insulin resistance, evaluate metabolic health, and monitor the effectiveness of insulin therapy.
A blood sample is drawn, usually from a vein in the arm, and sent to a laboratory. Specialized immunoassays are used to measure insulin levels in the serum.