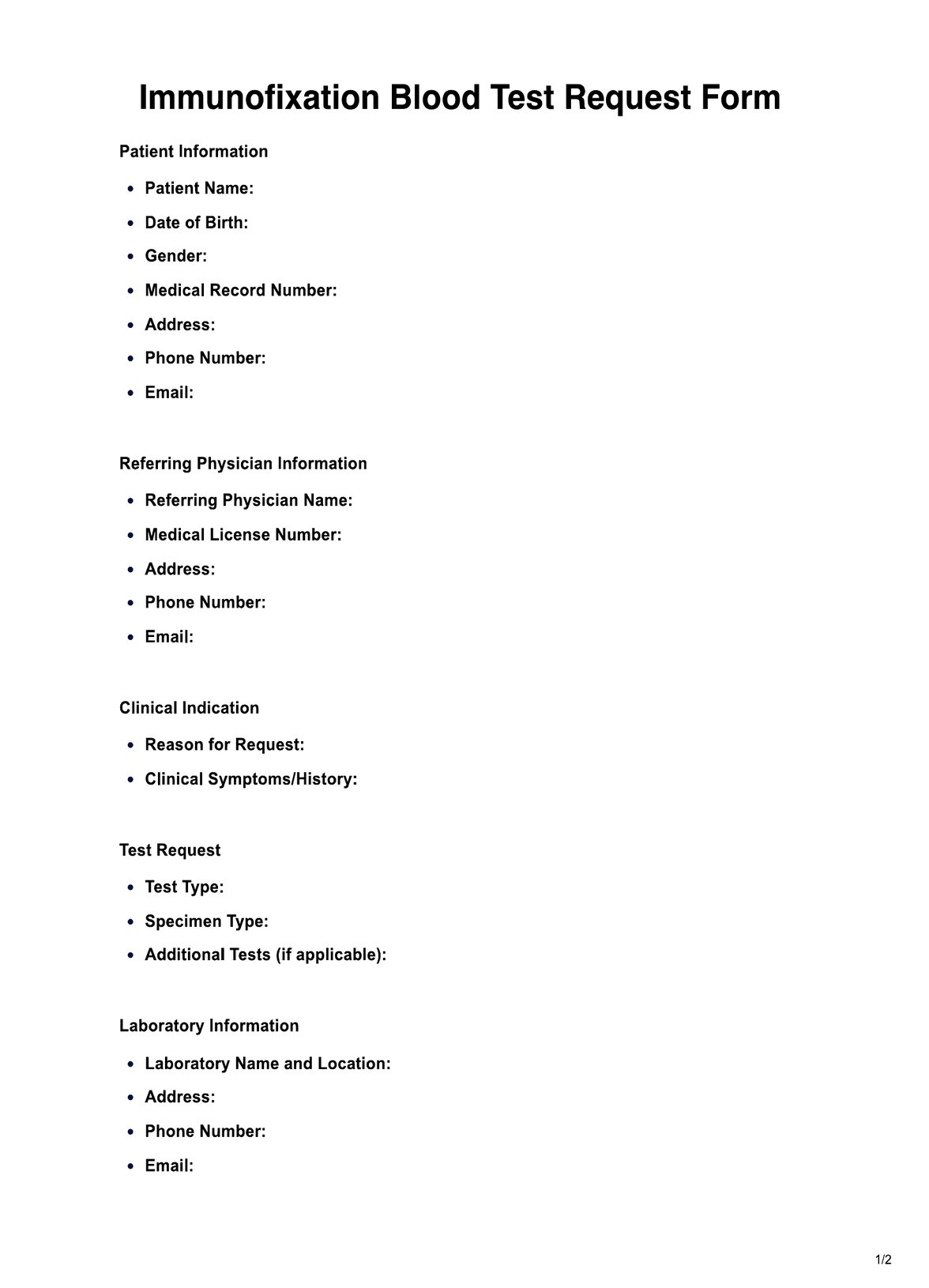
Immunofixation Blood Tests are typically requested by hematologists, nephrologists, oncologists, rheumatologists, and primary care physicians to diagnose and monitor conditions like multiple myeloma, kidney diseases, autoimmune disorders, and certain infections.