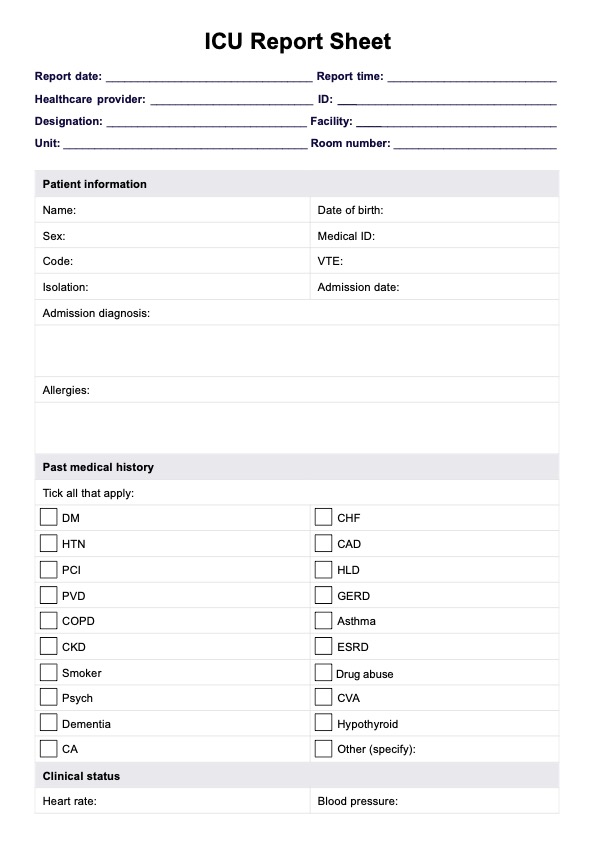
The template includes sections for patient information, vital signs, diagnoses, medications, and procedures. How the template is completed should be to your unit's specific needs and protocols, and to the specific patient care provided.
ICU Report Sheet Template
Access a comprehensive ICU Report Sheet Template for streamlined ICU nursing reports. Enhance communication and documentation in the intensive care setting.
ICU Report Sheet Template Template
Commonly asked questions
Templates are used during shift handovers, daily rounds, and emergencies. They serve as a quick reference for healthcare professionals to communicate all the details of a patient's care and status to a new nurse or doctors, and to document essential patient information.
Healthcare providers fill out templates with relevant patient details, including vital signs, medications, and upcoming events. The templates ensure standardized communication during transitions of care and support efficient decision-making. They may be attached to other assessments and reports such as a nursing brain sheet.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











