Food Allergies List Template
Download Carepatron's free Food Allergies List PDF template and example to help track patient allergens effectively.


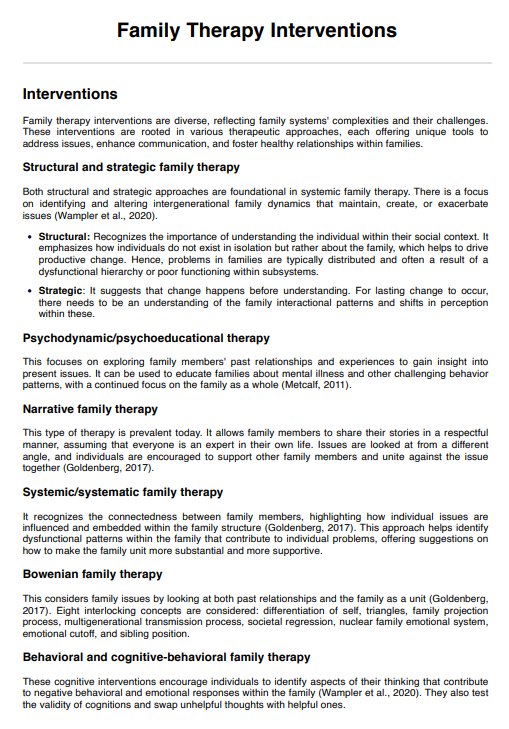
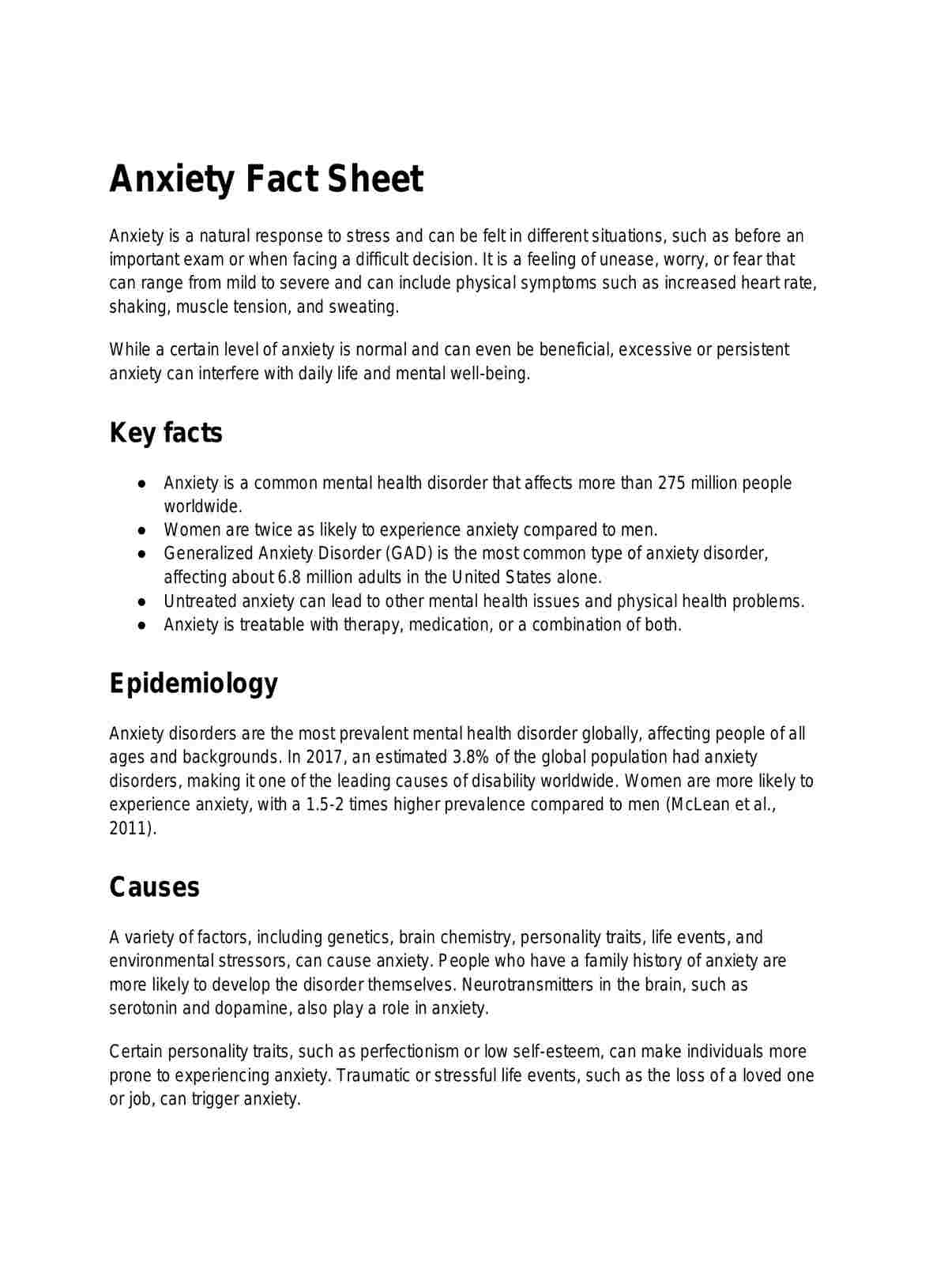
What are food allergies?
A food allergy is an immune system response in which specific food proteins are mistakenly identified as threats, triggering allergic reactions (Yu et al., 2016). These responses vary in severity, including skin rashes, gastrointestinal distress, respiratory issues, or a severe allergic reaction such as anaphylaxis (Cianferoni & Muraro, 2012).
Most food allergies present shortly after ingestion, though delayed onset is possible. The most common food allergies—often referred to as the “Big 9”—include milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame (U.S. Department of Agriculture, 2023). However, food allergy reactions can also be caused by less common triggers, including food additives and preservatives. Accurate identification is critical, as repeated exposure can increase the risk of sensitization and severity.
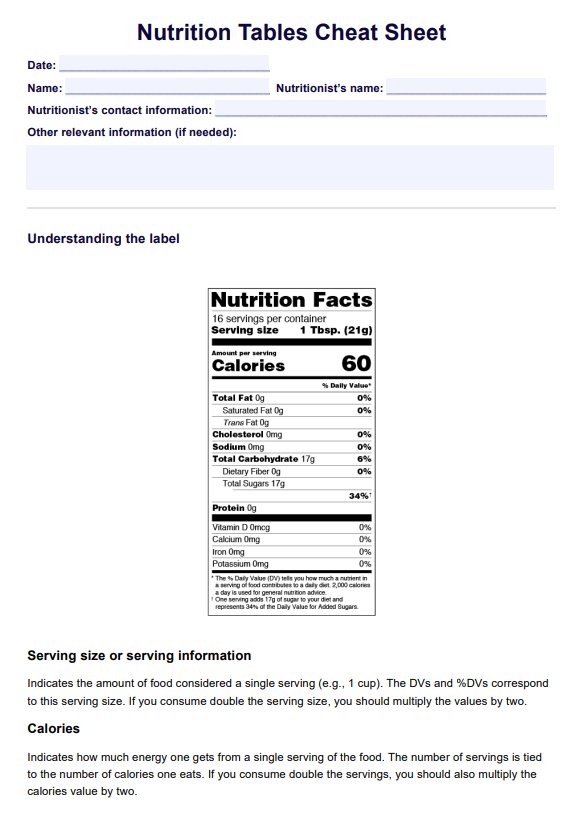
Medical professionals must carefully evaluate patient history, symptom presentation, and exposure timelines. Emphasis should also be placed on educating patients to read food labels, as hidden allergens are a significant concern. Understanding the mechanism behind most food allergies is essential in preventing life-threatening complications.
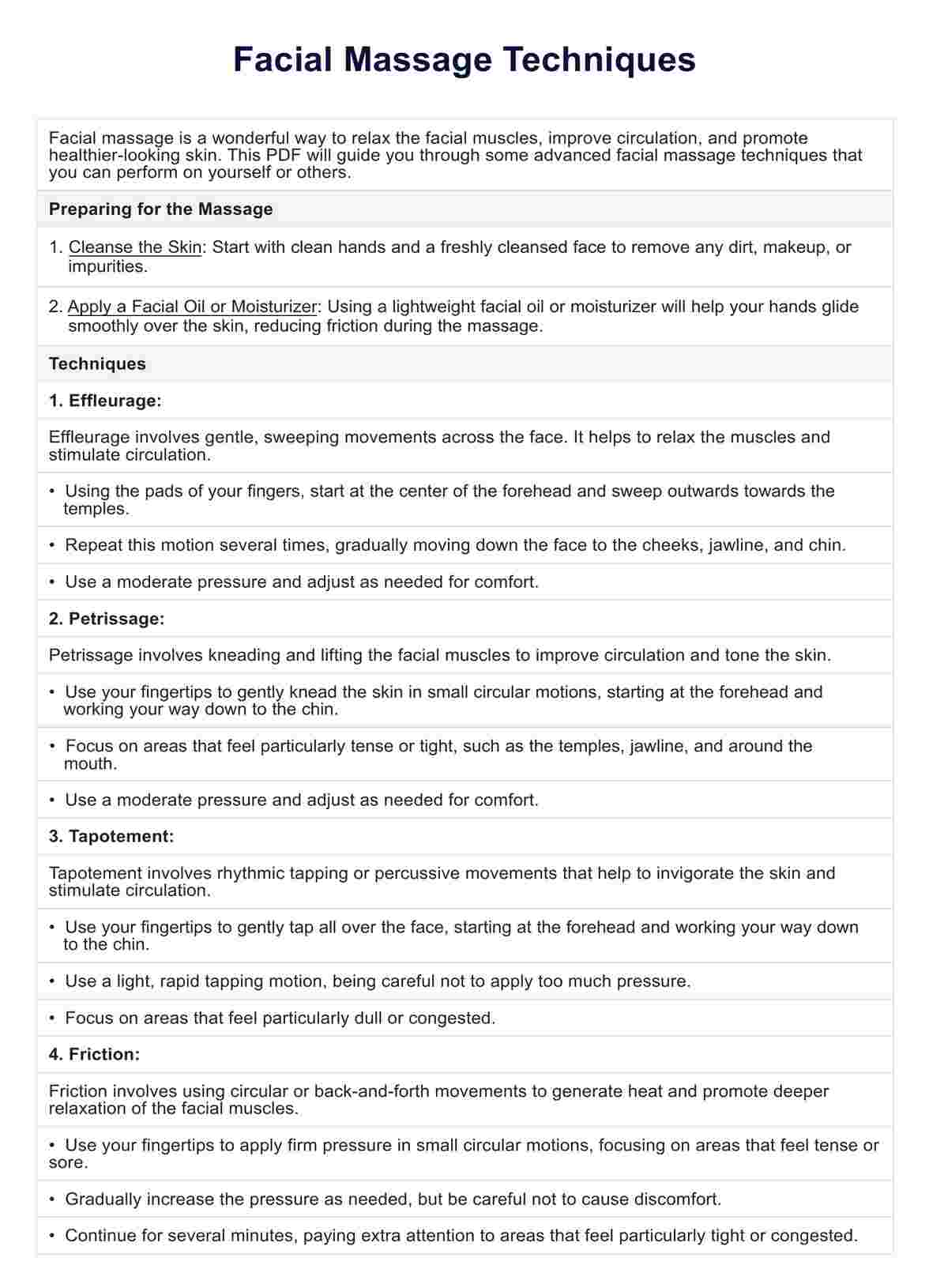
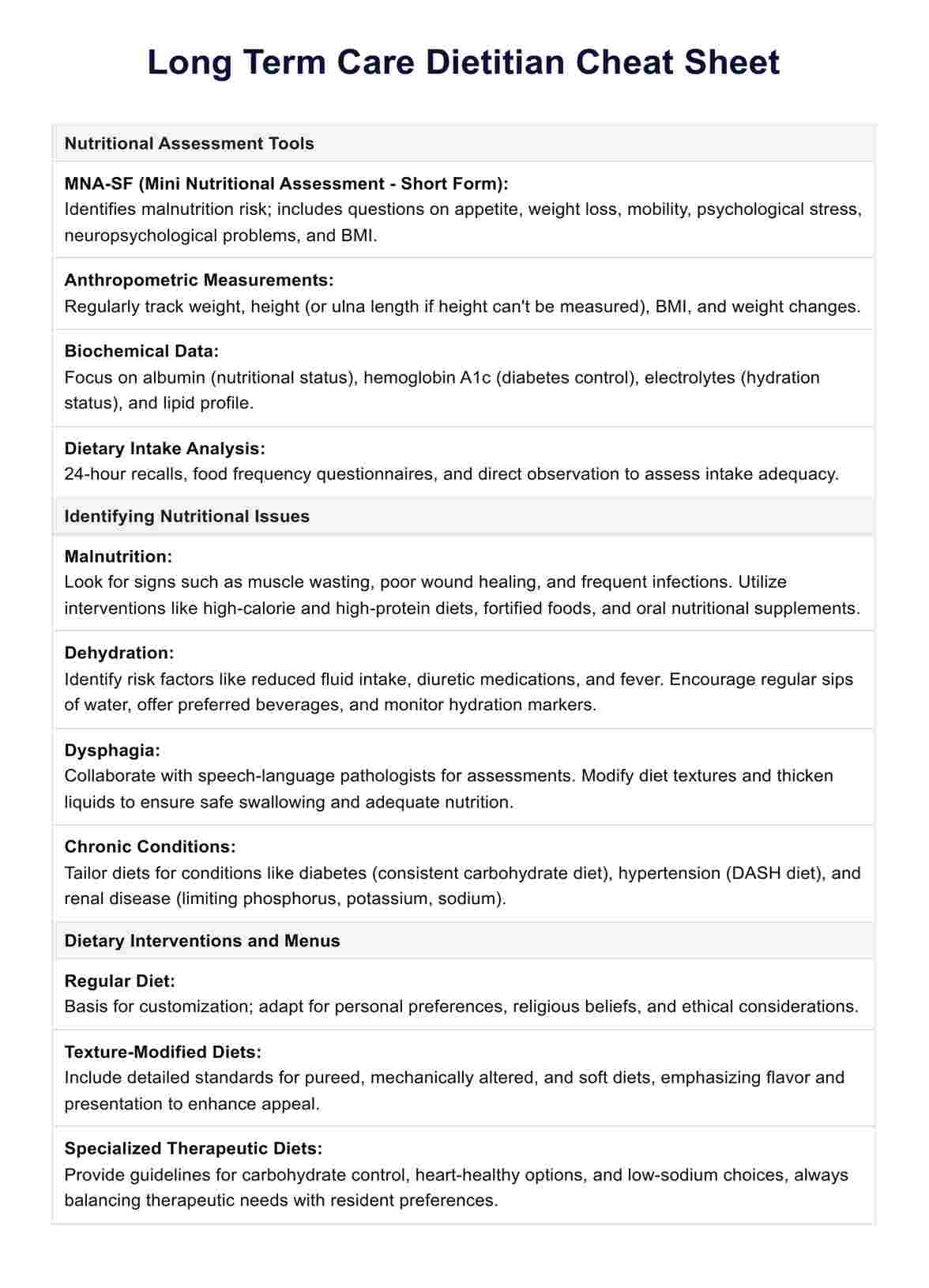
Food Allergies List Template
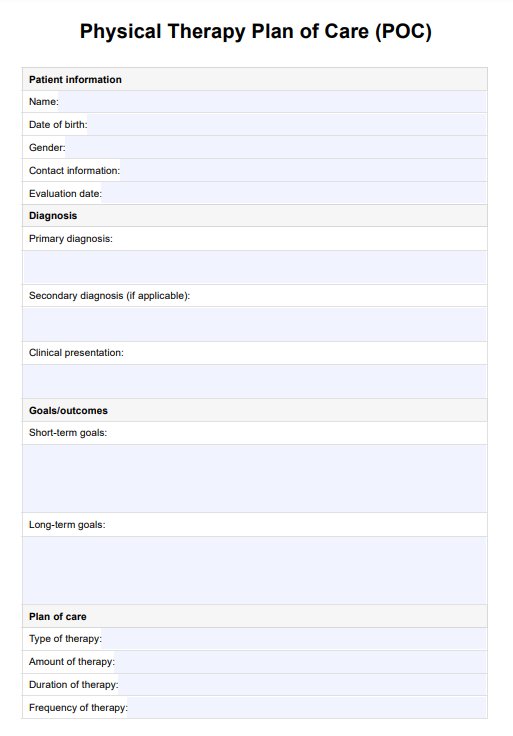
Food Allergies List Template Example
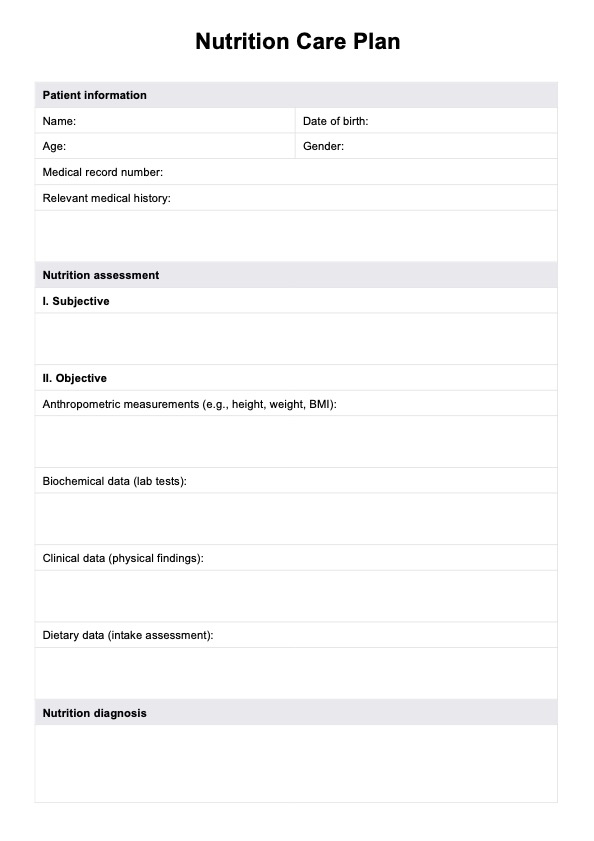
What is a Food Allergy List?
A Food Allergy List is a clinical tool healthcare practitioners use to identify, track, and manage adverse reactions caused by specific foods. It helps differentiate between a true food allergy and other conditions such as food poisoning or food intolerances. The list categorizes allergens based on prevalence and type, supporting targeted dietary assessment, diagnosis, and patient education.
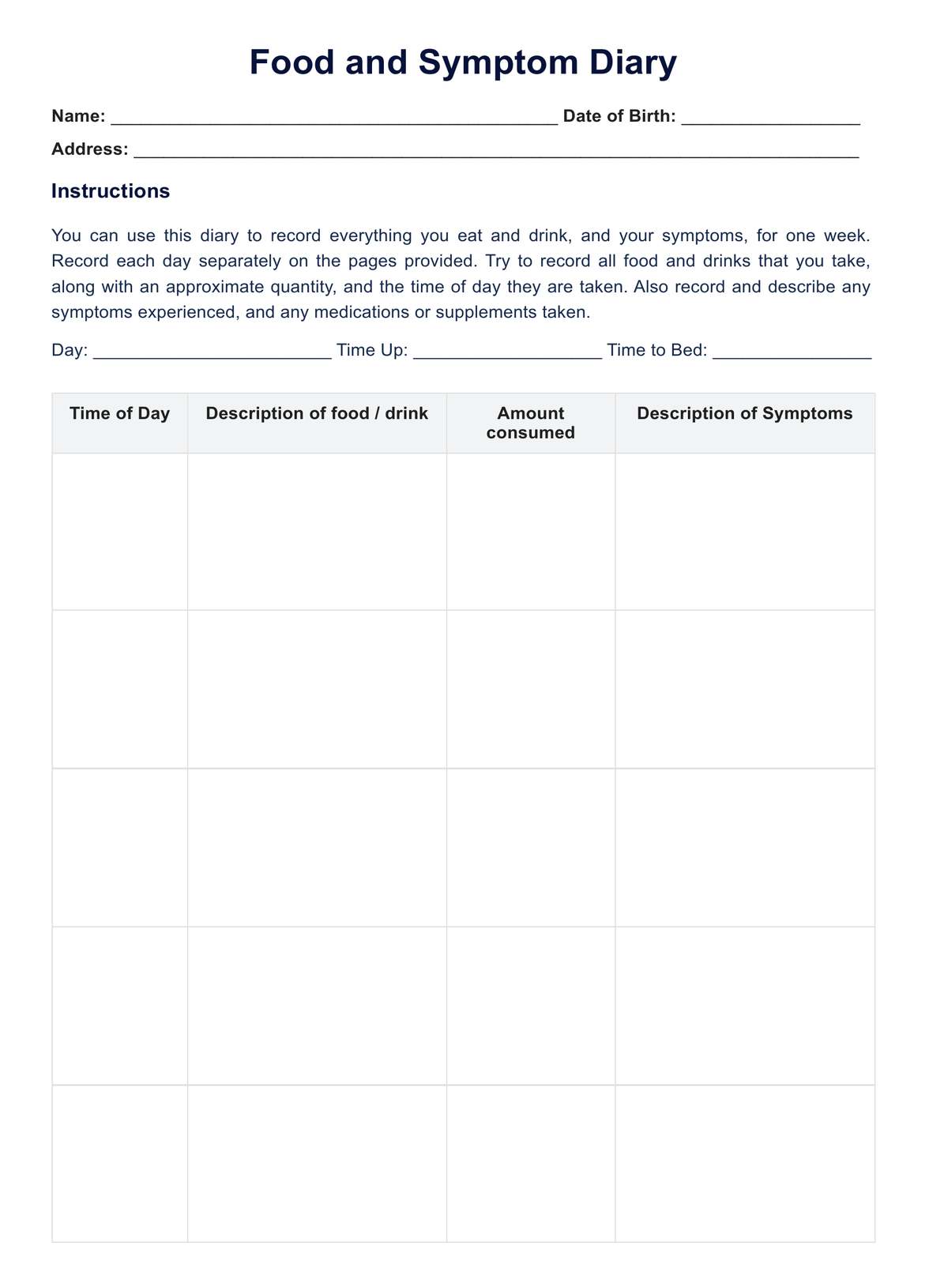
Because certain foods account for most allergic responses, especially in individuals with conditions like peanut allergy, celiac disease, or egg allergy, a Food Allergy List can be essential in reducing the risk of a severe reaction. It also aids in identifying potentially life-threatening triggers in patients with a history of anaphylaxis symptoms or fluctuating blood pressure during allergic episodes. When used with food diaries and diagnostic testing, this tool improves safety, particularly in patients consuming packaged foods or products containing natural flavoring and additives.
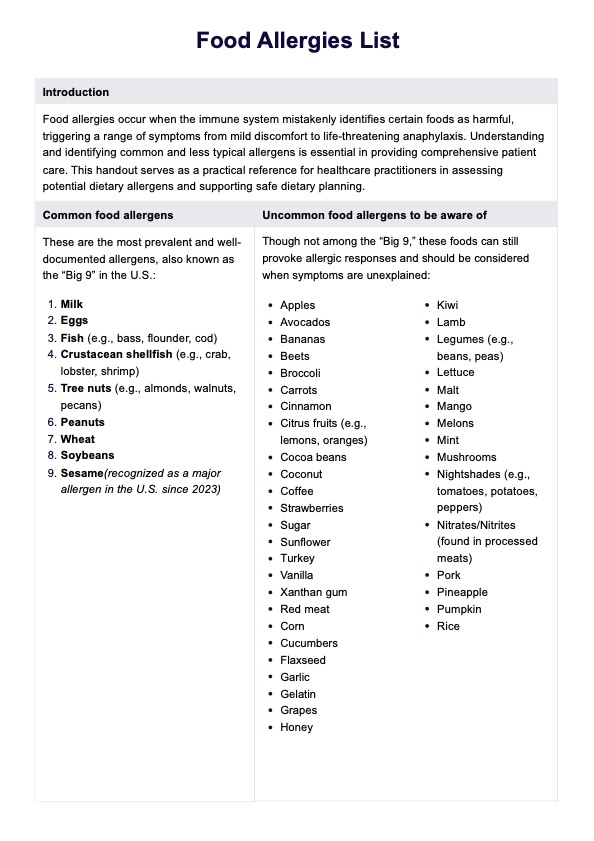
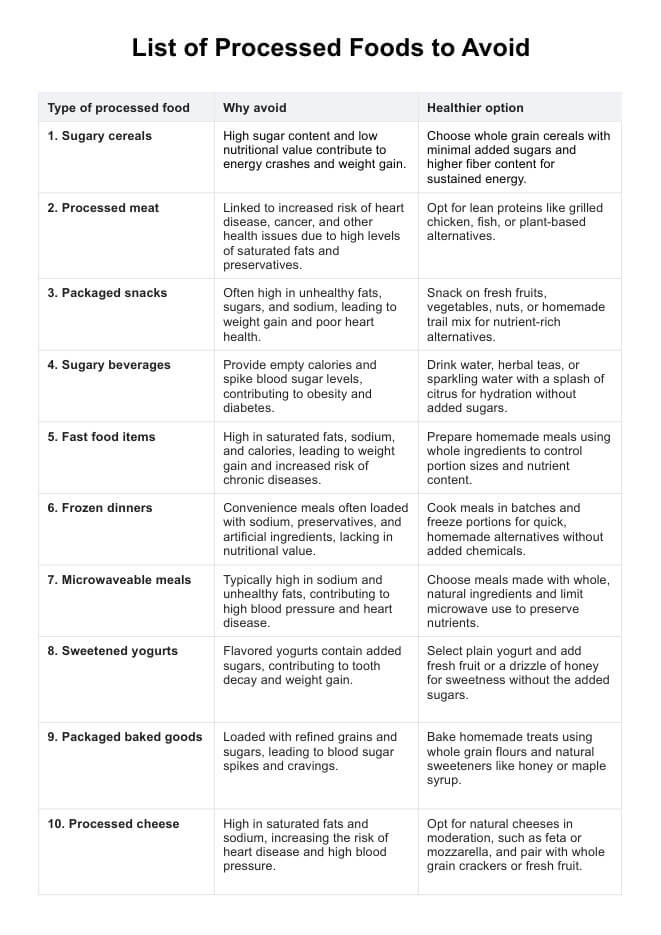
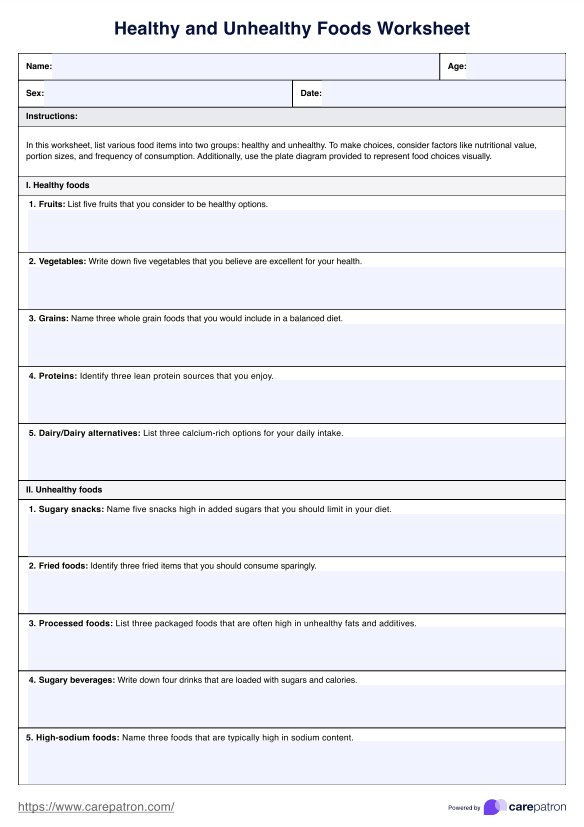
Common food allergens
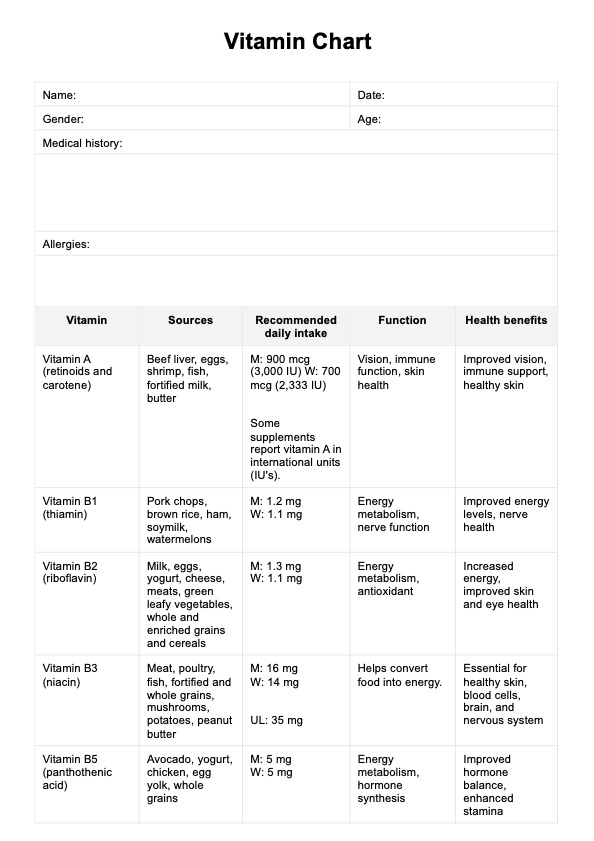
Common food allergens, also known as the “Big 9,” are responsible for most true food allergy cases in the United States. These include cow’s milk, eggs, peanuts, tree nuts, wheat, soybeans, fish, crustacean shellfish, and sesame.
Milk, egg, peanut, tree nut, wheat, and soy allergies are especially common in pediatric populations. These allergens are legally required to be listed on packaged foods due to their potential to cause a severe reaction or anaphylaxis symptoms. Crustacean shellfish and fish allergies are more prevalent in adults and can trigger gastrointestinal distress, respiratory issues, or drops in blood pressure. Because these foods are responsible for most allergic responses in children and adults, they are classified as major allergens.
Uncommon food allergens to be aware of
In addition to the Big 9, healthcare providers should consider uncommon food allergens when familiar sources do not explain the patient's allergic response. These include fruits (e.g., bananas, kiwis, strawberries), vegetables (e.g., carrots, cucumbers, nightshades), proteins like turkey and lamb, and even condiments or thickeners like xanthan gum (Hoffmann-Sommergruber, 2021). These foods may not be significant allergens legally, but they can still cause a severe reaction in sensitized individuals.
Symptoms are sometimes linked to oral allergy syndrome, particularly in patients with pollen sensitivities. Other uncommon allergens—like coconut, honey, coffee, or pumpkin—may be masked in natural flavoring or present in fermented or processed foods. For celiac disease or gluten allergy patients, reactions to grains like barley, rye, and malt may also occur. Accurate history-taking and awareness of these less typical triggers are essential to preventing adverse reactions and ensuring safe dietary planning.
Other food allergens
Other food allergens are caused by processing methods, environmental interactions, or cross-reactivity with non-food allergens (Verhoeckx et al., 2015). These often involve food additives, preservatives, spices, or fermented products that can lead to histamine intolerance or mimic a food allergy. Patients with latex sensitivity, for example, may exhibit allergic responses to avocados, chestnuts, or bananas due to protein similarities—a condition known as latex-fruit syndrome. Likewise, oral allergy syndrome is triggered by cross-reactivity between pollens and raw fruits or vegetables.
Fermented foods and aged cheeses may also cause adverse reactions in patients with histamine sensitivity. Additionally, hidden ingredients in sauces, international cuisine, or packaged foods can result in unexpected anaphylaxis symptoms. While these allergens are less common, they are clinically significant and potentially life-threatening. A thorough review of food labels and ingredient lists is crucial, especially when evaluating unexplained allergic responses in complex cases.
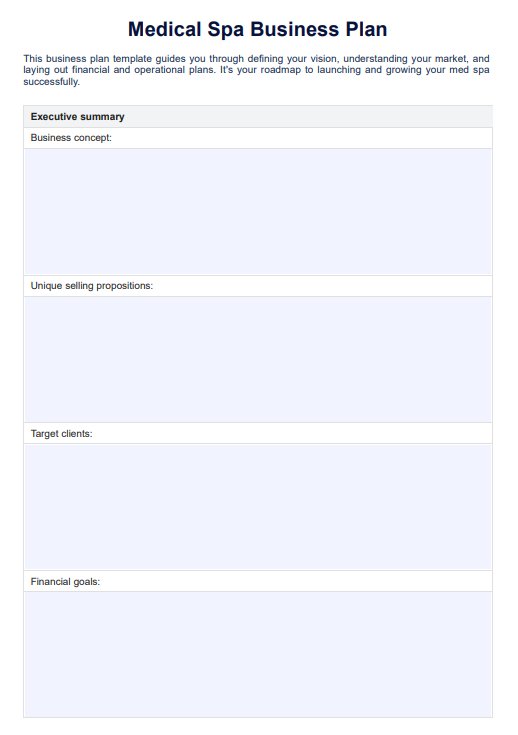
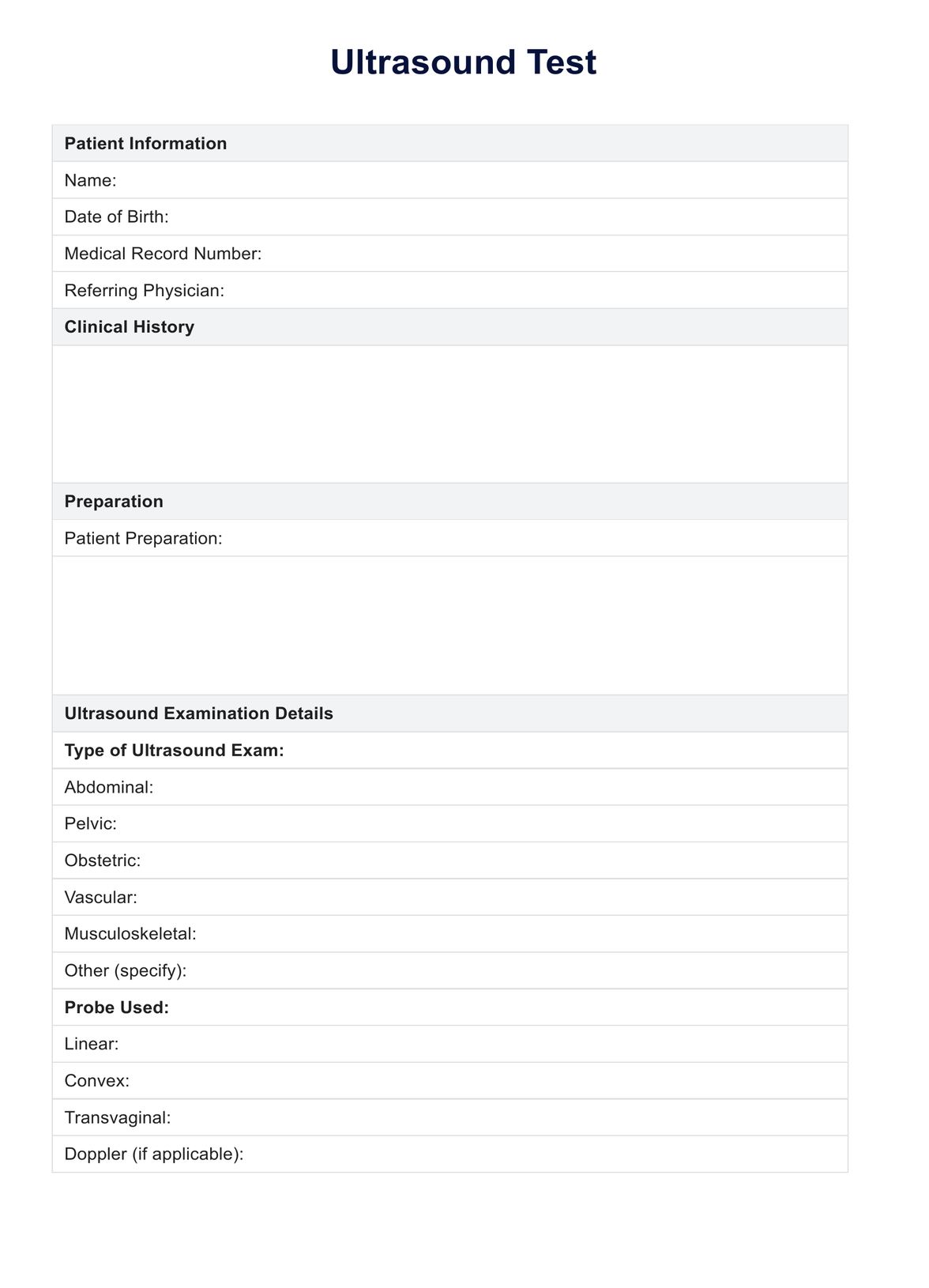
How does it work?
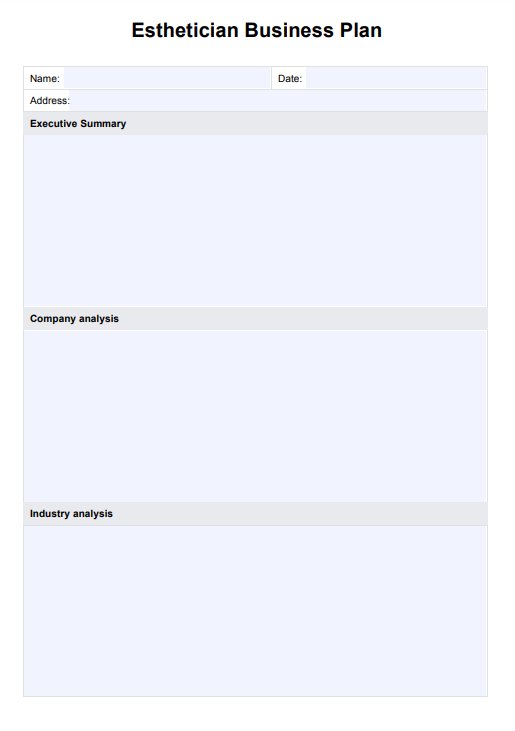
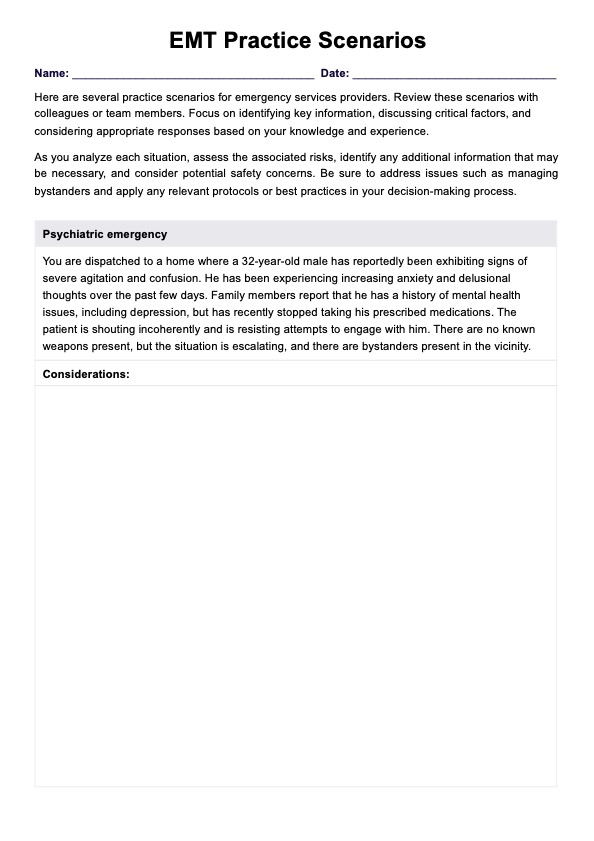
Carepatron’s Food Allergies List is designed to integrate seamlessly into your clinical workflow. It supports allergy assessments, dietary planning, and patient education with structured, easy-to-reference data. By following a few simple steps, healthcare professionals can use this resource efficiently during consultations and follow-up care.
Step 1: Access the handout
Click the “Use template” button to immediately access the Food Allergies List within the Carepatron platform. You’ll be directed to download the Carepatron app if you haven’t already done so. Once inside, the template will be ready for use with no setup or formatting required.
Step 2: Use the handout in patient consultation
During consultations, use the Food Allergies List to identify potential allergens based on patient-reported symptoms or medical history. It can guide clinical questioning and help streamline differential diagnosis, particularly when evaluating true food allergy versus food intolerance or food poisoning.
Step 3: Discuss how the handout works
Explain how the handout categorizes allergens—common, uncommon, and other—to provide a comprehensive overview. Clarify which allergens may trigger a severe reaction or anaphylaxis symptoms and encourage patients to monitor packaged foods and natural flavoring for hidden risks.
Step 4: Provide additional patient support and next steps
Use the handout to support long-term dietary planning, label reading, and symptom tracking. Recommend follow-up allergy testing, nutritional counseling, or an emergency management plan if necessary. The handout helps ensure patients understand their risks and remain vigilant about potential exposures.
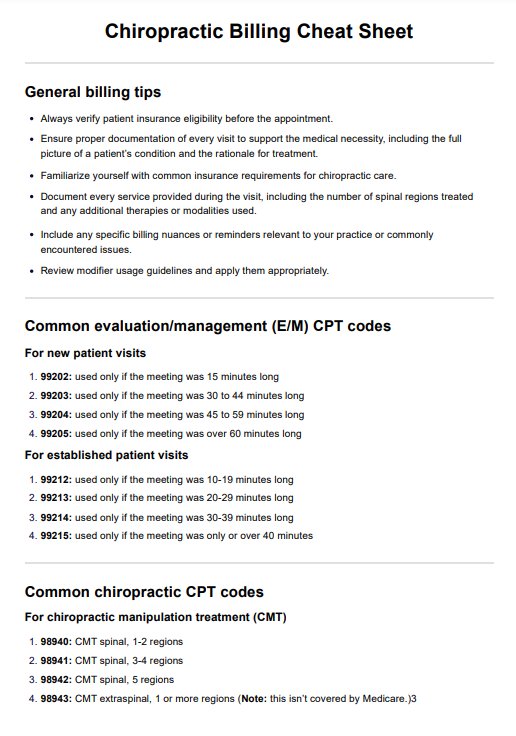
Benefits of using this handout
Using the Food Allergies List handout streamlines clinical assessment by providing a clear, categorized reference of foods known to cause allergic reactions. It supports faster identification of potential triggers by highlighting both common and less typical allergy causing proteins, including those found in patients with a shellfish allergy or other significant sensitivities.
This tool allows medical professionals to correlate symptoms with the offending food more accurately, improving diagnostic accuracy and reducing the risk of overlooking key allergens. It also reinforces patient education around strict avoidance of known triggers and emphasizes the importance of checking food products for hidden ingredients.
By enabling more structured conversations during consultations, it helps reduce the likelihood of re-exposure that can lead to life-threatening symptoms. Additionally, it promotes efficiency in dietary planning and allergy documentation, ensuring consistent care when the body produces an immune response to problematic foods. This ultimately enhances safety, accuracy, and workflow for healthcare providers.
References
Cianferoni, A., & Muraro, A. (2012). Food-induced anaphylaxis. Immunology and Allergy Clinics of North America, 32(1), 165–195. https://doi.org/10.
Hoffmann-Sommergruber, K. (2021). Rare food allergens. Allergologie Select, 5(1), 29–32. https://doi.org/10.5414/alx02135e
U.S. Department of Agriculture. (2023). Food allergies: The “Big 9” | Food Safety and Inspection Service. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/food-allergies-big-9
Verhoeckx, K. C. M., Vissers, Y. M., Baumert, J. L., Faludi, R., Feys, M., Flanagan, S., Herouet-Guicheney, C., Holzhauser, T., Shimojo, R., van der Bolt, N., Wichers, H., & Kimber, I. (2015). Food processing and allergenicity. Food and Chemical Toxicology, 80, 223–240. https://doi.org/10.1016/j.fct.2015.03.005
Yu, W., Freeland, D. M. H., & Nadeau, K. C. (2016). Food allergy: Immune mechanisms, diagnosis, and immunotherapy. Nature Reviews Immunology, 16(12), 751–765. https://doi.org/10.1038/nri.2016.111
Commonly asked questions
The 14 major food allergens include milk, eggs, peanuts, tree nuts, soy, wheat, fish, crustacean shellfish, sesame, celery, mustard, lupin, mollusks, and sulfites. These allergens are responsible for most food-related allergic reactions and must be clearly labeled on food products in many regions.
Allergens in food are specific proteins that trigger an immune response in individuals with a food allergy. These proteins cause allergic reactions ranging from mild to potentially life-threatening symptoms like anaphylaxis.
Ten rare food allergies include red meat, coconut, corn, sunflower seeds, gelatin, mango, mushrooms, vanilla, flaxseed, and lettuce. Though uncommon, these foods can still cause severe allergic responses in sensitized individuals.
Common food allergy symptoms include hives, itching, swelling, abdominal pain, vomiting, wheezing, and difficulty breathing. In severe cases, symptoms can escalate quickly and result in anaphylaxis, requiring immediate medical attention.