DSM 5 Criteria for Binge Eating Disorder
Explore the DSM-5 Criteria for Binge Eating Disorder with our comprehensive template. Understand the diagnosis, impact, and treatment options for BED.


What is a binge eating disorder?
Binge eating disorder (BED) is a serious eating disorder characterized by recurrent episodes of eating large quantities of food in a short period, often to the point of discomfort. Unlike other eating disorders, individuals with BED do not regularly engage in compensatory behaviors like purging or excessive exercise to counteract binge eating. This disorder is marked by feelings of loss of control, shame, guilt, and distress following binge episodes.
The exact cause of BED is unknown, but it is believed to be a combination of various factors:
- Genetic predisposition: Research by Manfredi et al. (2021) and Trace et al. (2013) suggests that genetics may play a role in BED development.
- Psychological factors: Low self-esteem, body dissatisfaction, and a history of dieting can contribute to the onset of the disorder.
- Emotional triggers: Stress, anxiety, and depression are often linked to binge eating episodes.
- Sociocultural influences: Pressure to conform to societal beauty standards and exposure to media that promotes thinness can increase the risk of developing BED.
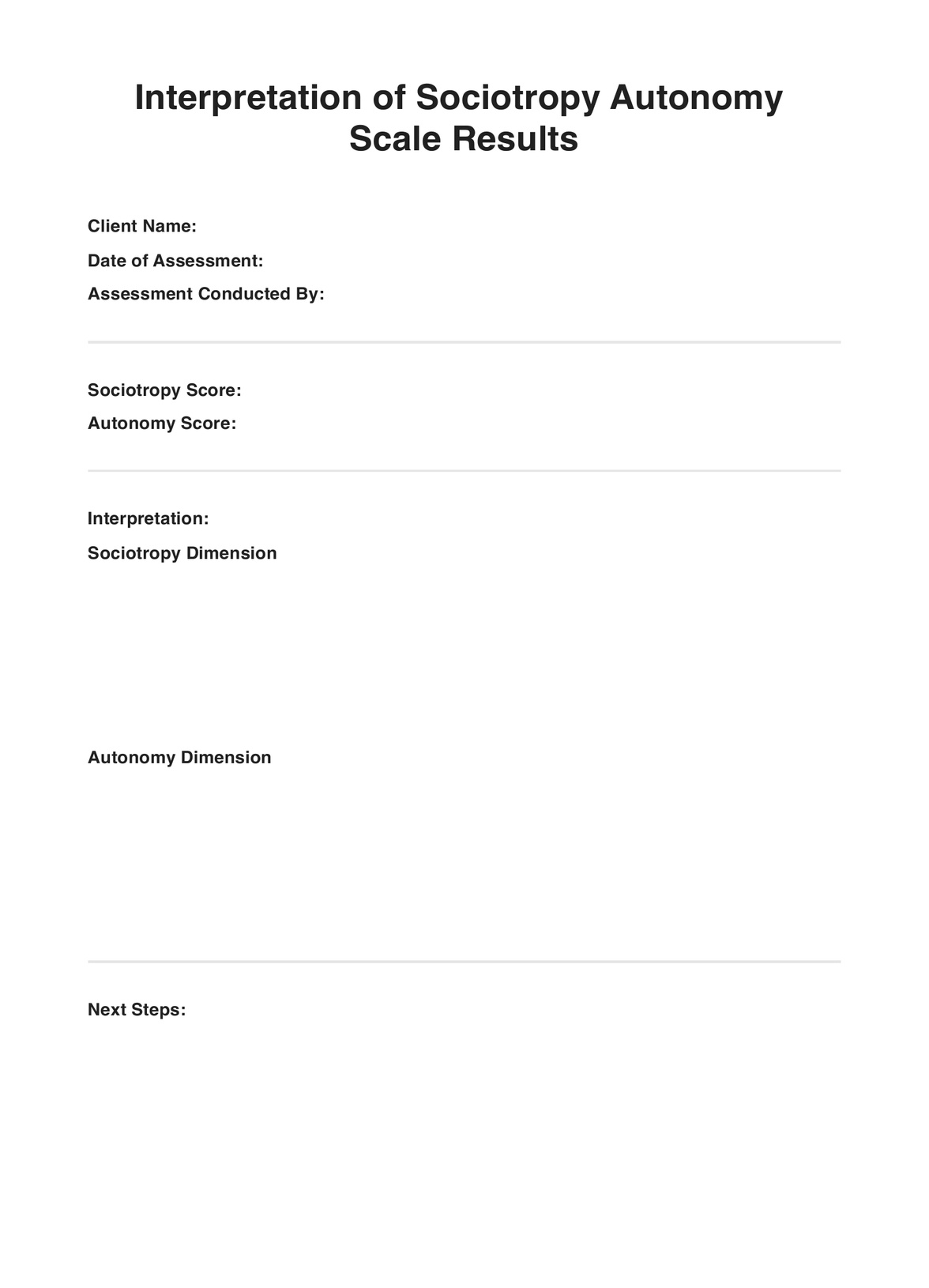
DSM 5 Criteria for Binge Eating Disorder Template
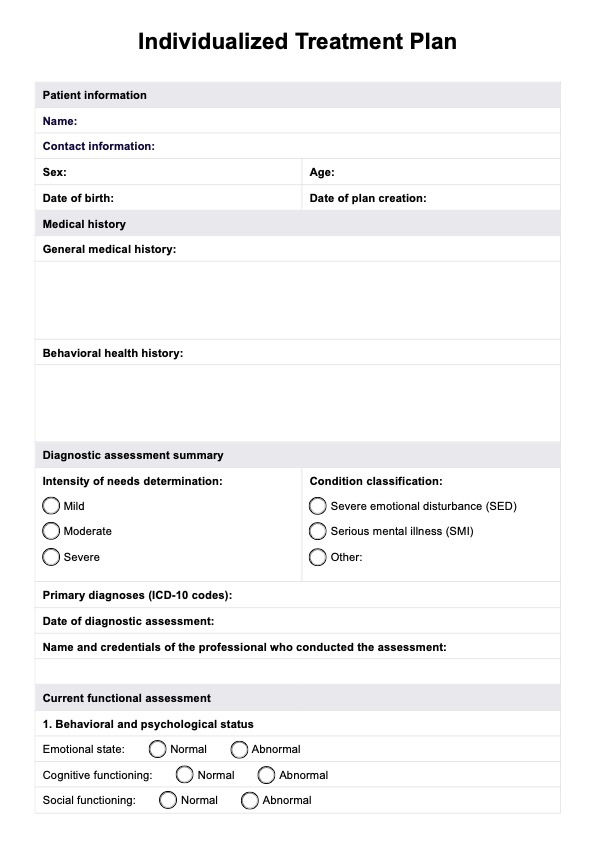
DSM 5 Criteria for Binge Eating Disorder Example
What are the effects of binge eating disorder on a person?
The impact of BED extends beyond the psychological distress of the episodes themselves, significantly affecting an individual's physical health:
- Obesity: BED often leads to weight gain and obesity due to the consumption of large amounts of high-calorie foods during binge episodes. Obesity, in turn, increases the risk of numerous health problems, including heart disease, type 2 diabetes, and certain cancers.
- Cardiovascular disease: The excessive intake of unhealthy fats and sugars can contribute to the development of heart disease, high blood pressure, and high cholesterol levels.
- Type 2 diabetes: Regular binge eating can lead to insulin resistance, a precursor to type 2 diabetes, due to the body's inability to effectively manage sugar levels.
- Digestive issues: BED can cause gastrointestinal problems such as acid reflux, bloating, and constipation due to the overconsumption of food and the stress placed on the digestive system.
- Sleep disorders: People with BED may experience sleep disturbances, including insomnia and sleep apnea, which can be exacerbated by obesity and the discomfort of overeating.
In addition to these physical health consequences, BED can also lead to emotional and social impairments, such as feelings of shame, isolation, and difficulties in relationships. The comprehensive impact of BED underscores the importance of seeking professional help for diagnosis and treatment to mitigate these adverse effects and improve overall well-being.
How is binge eating disorder diagnosed?
Diagnosing BED involves a detailed evaluation by a mental health professional or healthcare provider. Here's a more specific breakdown of the process:
- Clinical interview: A thorough interview discusses the individual's eating habits, emotional state, and any binge eating patterns. This interview helps to gather comprehensive information about the symptoms and their impact on the person's life.
- Psychological assessments: Specific standardized tests and questionnaires are used to assess the symptoms of BED and distinguish it from other eating disorders or mental health conditions. Some common assessments include the Eating Disorder Examination (EDE) or the Binge Eating Scale (BES).
- Physical examination: A healthcare provider may perform a physical exam to check for signs of health issues related to binge eating, such as obesity, high blood pressure, or type 2 diabetes. Blood tests may also assess cholesterol levels, blood sugar levels, and overall metabolic health.
- Review of eating patterns: The individual may be asked to take a quiz or keep a food diary to record their eating patterns, including the frequency, quantity, and circumstances of binge eating episodes.
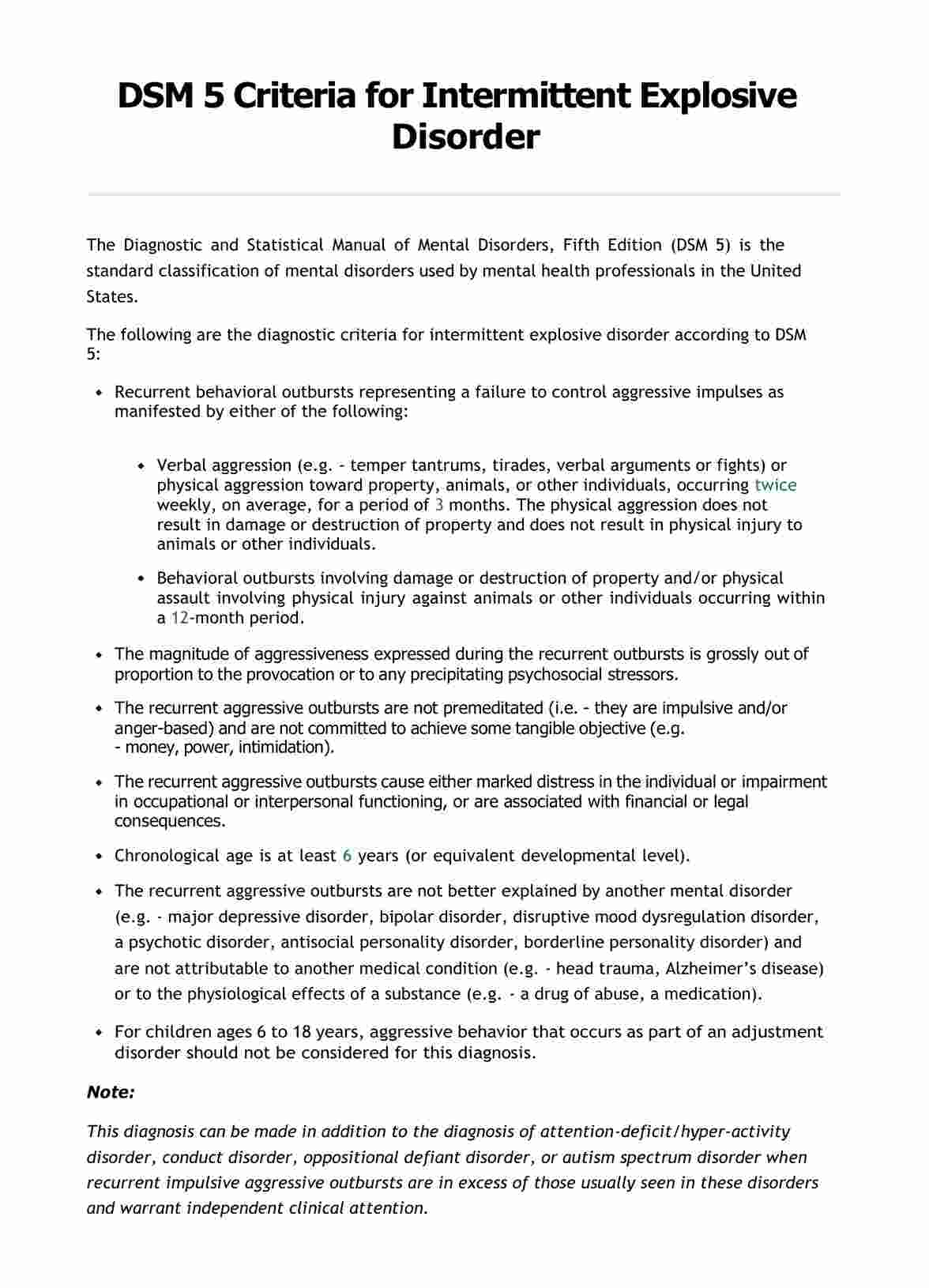
- DSM 5 criteria: The mental health professional will refer to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), to ensure that the individual meets the specific criteria for BED. These criteria include recurrent episodes of binge eating, a lack of control during these episodes, and significant distress or impairment in functioning.
- Assessment of co-occurring conditions: Many individuals with BED also experience other mental health disorders, such as depression, anxiety, or substance abuse. Evaluating these conditions is essential for a comprehensive diagnosis and treatment plan.
- Family and social history: Gathering information about the individual's family dynamics, social environment, and any history of trauma or abuse can provide insights into the factors contributing to the development of BED.
By using a combination of these diagnostic methods, specialists can accurately diagnose BED and differentiate it from other eating disorders or related conditions, ensuring that individuals receive the appropriate treatment and support for their specific needs.
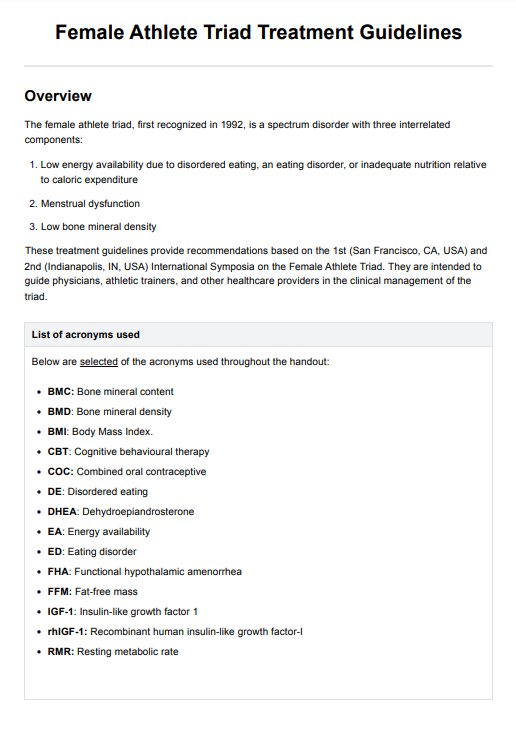
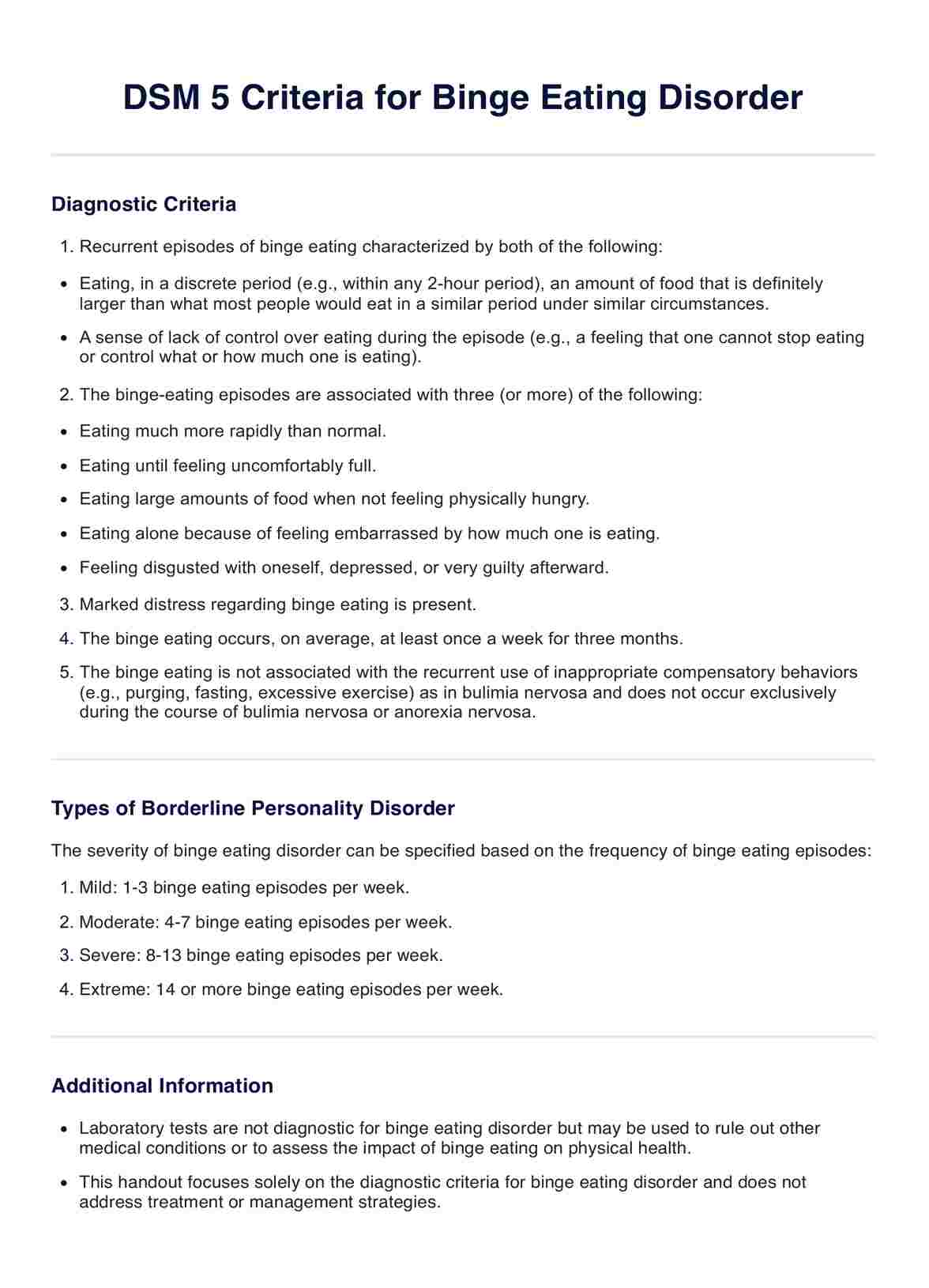
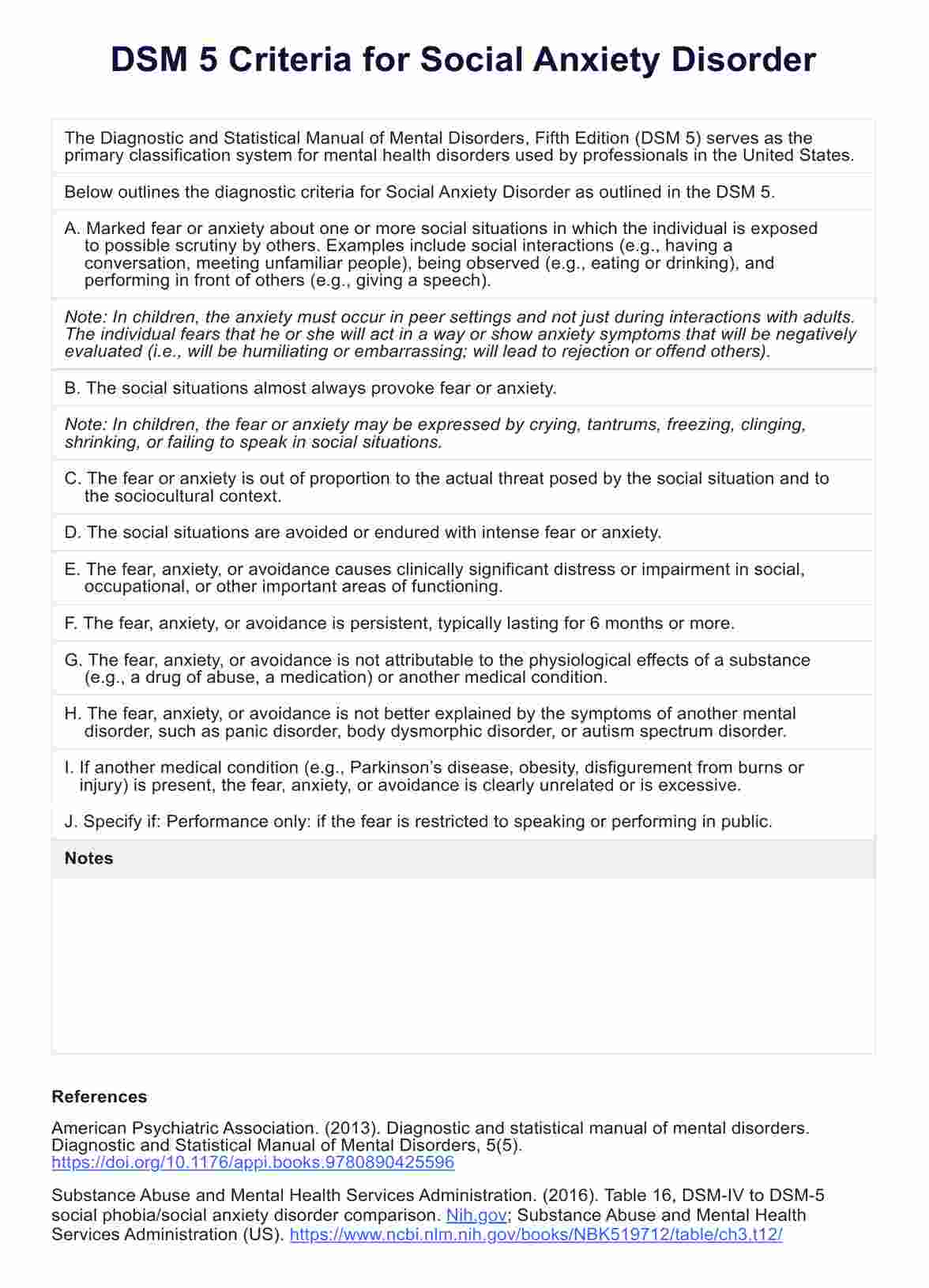
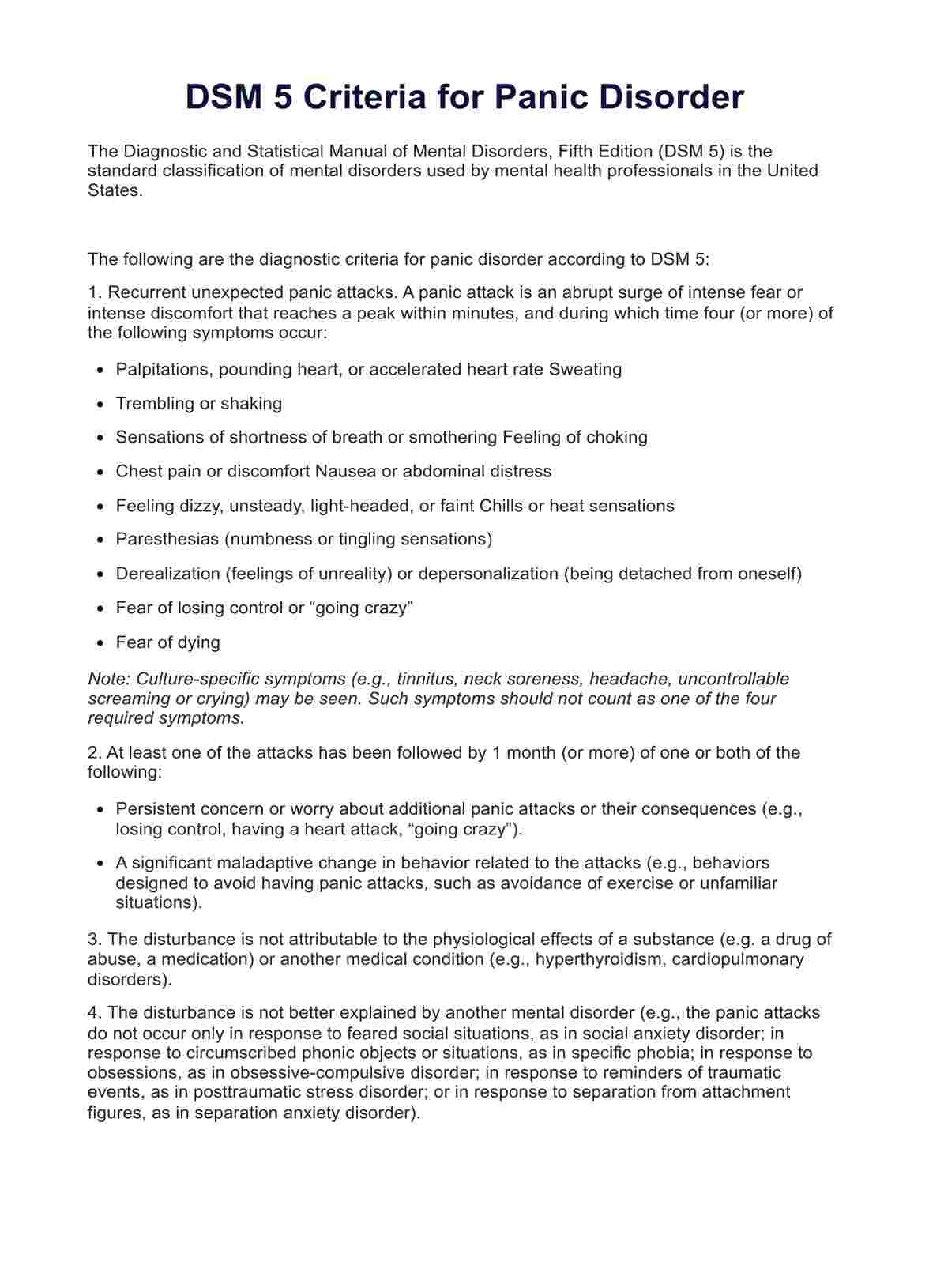
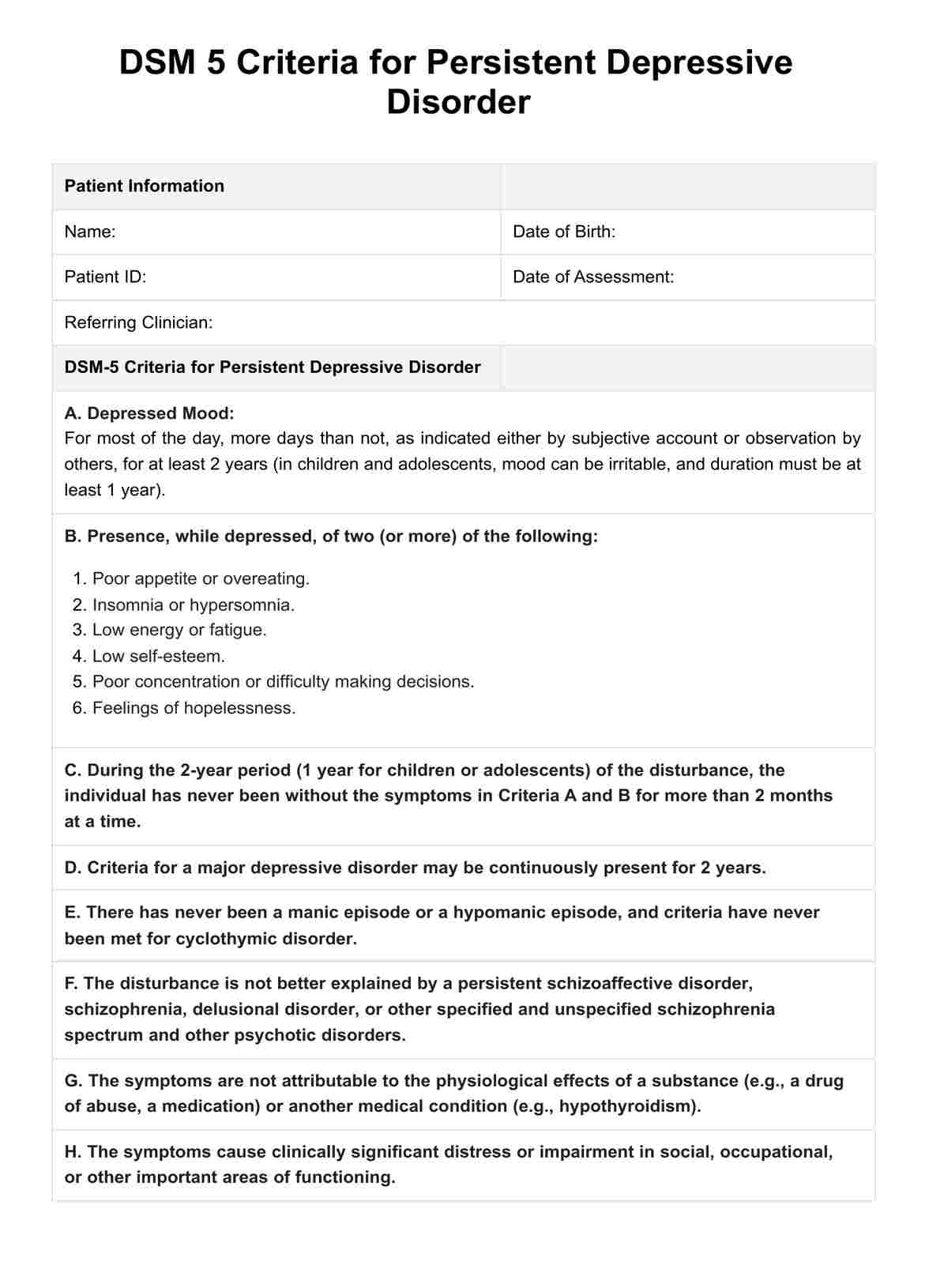
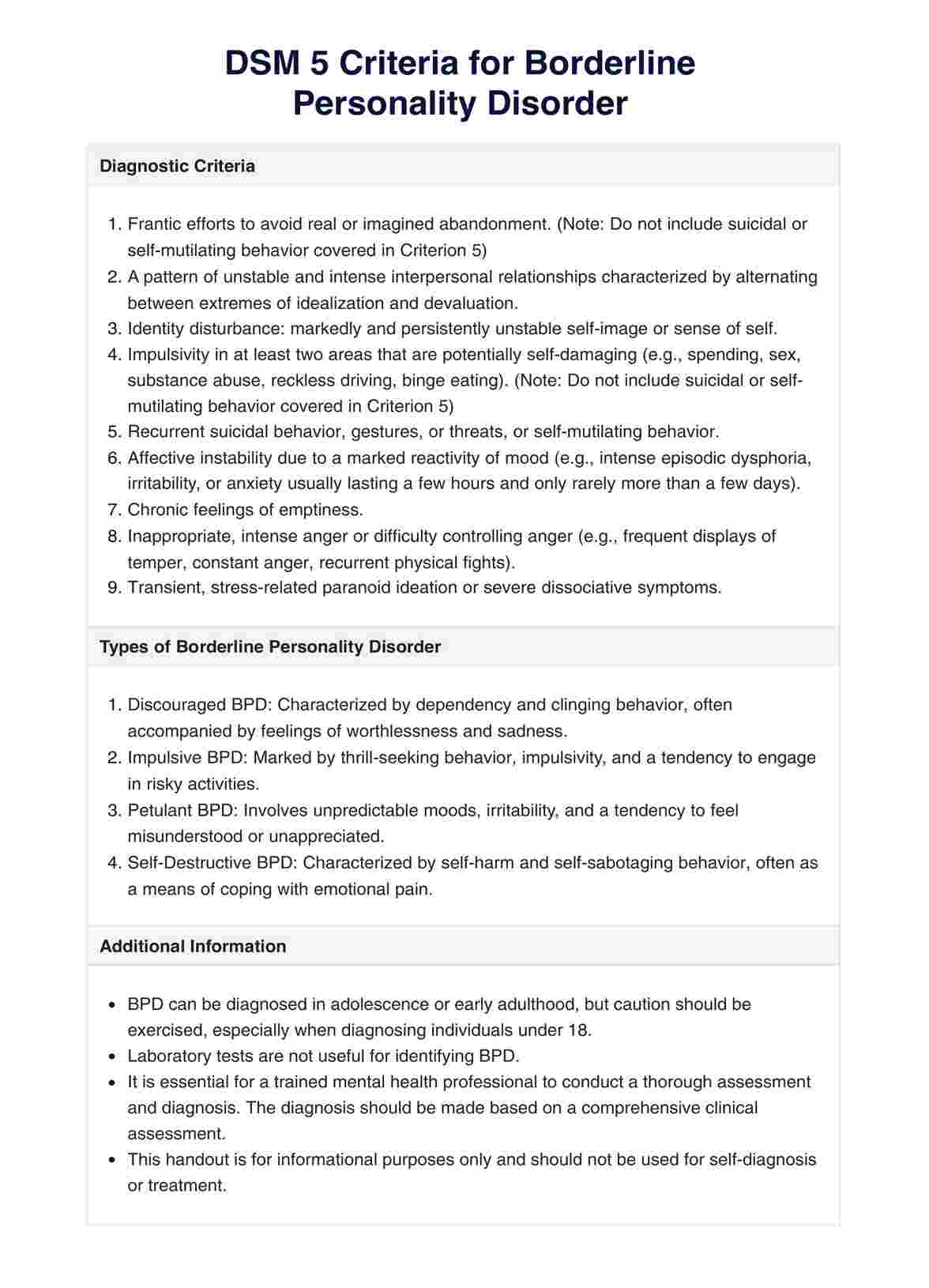
DSM criteria for binge eating disorder
The DSM 5 was mentioned in the process of diagnosing BED earlier. Simply put, the DSM serves as the manual by which disorders can be diagnosed. The manual was created to improve the reliability and validity of psychiatric diagnoses, facilitate research, and guide clinical practice. This makes the DSM a critical tool in psychiatry and psychology, providing a standardized classification system for mental disorders.
The American Psychiatric Association (APA) developed the DSM, with the first edition published in 1952. Over the years, the DSM has undergone several revisions to incorporate new findings and evolving perspectives in mental health. The most recent edition, the DSM-5, was published in 2013 and includes updated criteria and classifications to reflect the current understanding of mental disorders.
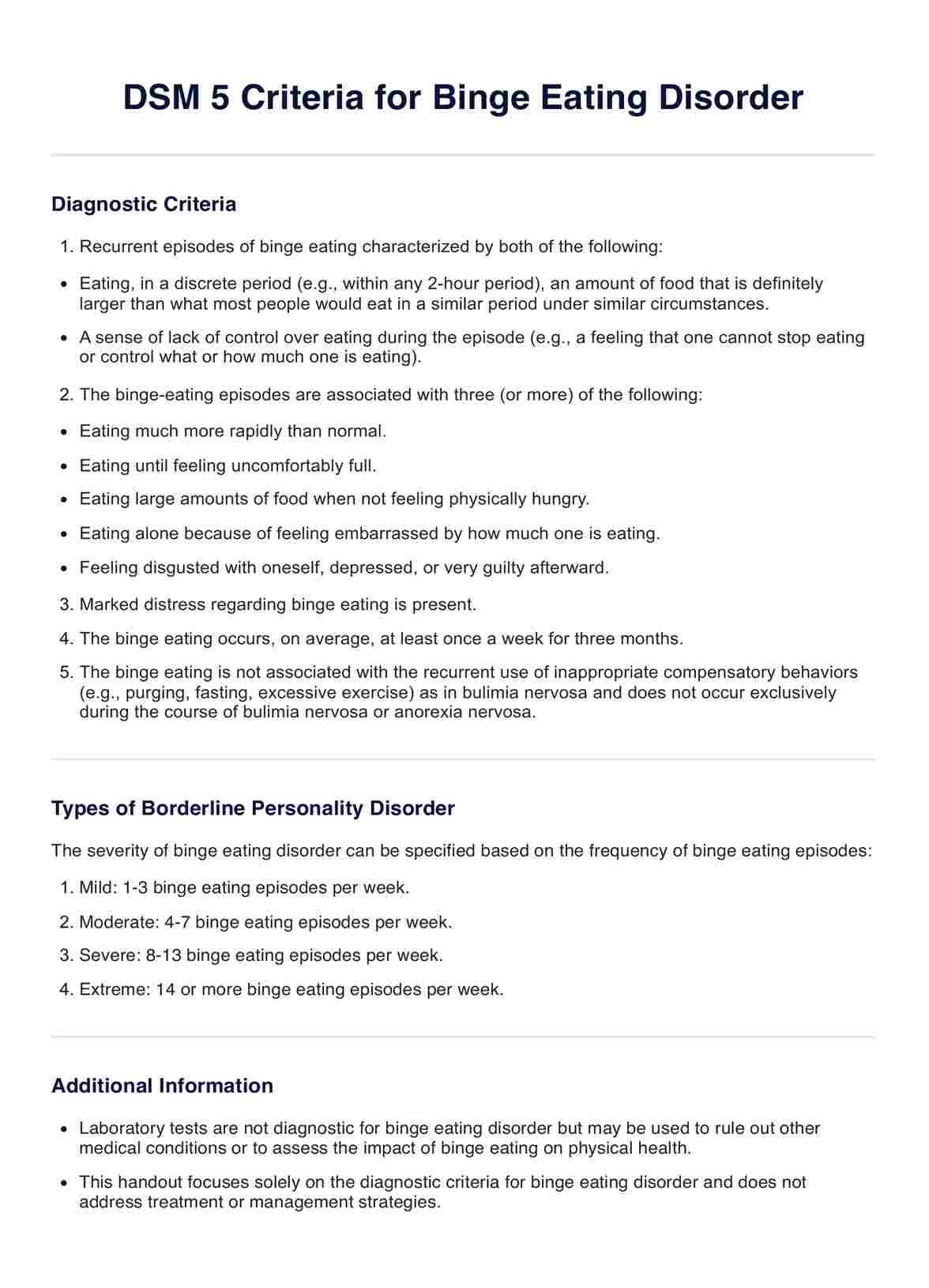
According to DSM 5, here are the criteria for binge eating disorder:
- Recurrent episodes of binge eating: An episode of binge eating is characterized by both of the following:some text
- Eating, in a discrete period of time (e.g., within any 2-hour period), an amount of food that is definitely larger than what most people would eat in a similar period under similar circumstances.
- A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
- The binge eating episodes are associated with three (or more) of the following:some text
- Eating much more rapidly than normal.
- Eating until feeling uncomfortably full.
- Eating large amounts of food when not feeling physically hungry.
- Eating alone because of feeling embarrassed by how much one is eating.
- Feeling disgusted with oneself, depressed, or very guilty afterward.
- Marked distress regarding binge eating: The binge eating occurs, on average, at least once a week for three months.
- The binge eating is not associated with the recurrent use of inappropriate compensatory behaviors (e.g., purging, fasting, excessive exercise) as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa.
Difference between the DSM 4 and 5's criteria for binge eating disorder
The DSM-IV and DSM-5 diagnostic criteria for BED share many similarities, but there are some key differences that have implications for diagnosis and treatment. Here's what changed:
- Frequency and duration: DSM 5 makes it easier for more people to be diagnosed and receive help, by lowering the frequency and shortening the duration of observation.some text
- DSM-IV: Binge eating occurs at least 2 days a week for 6 months.
- DSM-5: Binge eating occurs at least 1 day a week for 3 months.
- Severity grading: With DSM 5, a scale is introduced, helping doctors understand how serious the disorder is and plan treatment better.some text
- DSM-IV: No severity grading scale for BED.
- DSM-5: Introduces a severity grading scale based on the number of binge eating episodes per week, ranging from mild to extreme.
How is binge eating disorder treated?
BED requires a comprehensive treatment approach, often involving a team of specialists. Here's a detailed look at the treatment options:
- Cognitive behavioral therapy (CBT): Considered the gold standard for treating BED, CBT helps individuals identify and change negative thought patterns and behaviors related to binge eating. Therapists work with patients to develop coping strategies for dealing with triggers and emotions that lead to binge episodes.
- Interpersonal psychotherapy (IPT): IPT addresses the interpersonal issues that may contribute to binge eating, such as relationship conflicts or social isolation. The therapy focuses on improving communication skills and building healthier relationships to reduce emotional distress and binge eating.
- Dialectical behavior therapy (DBT): DBT teaches patients skills to regulate emotions, tolerate distress, and improve mindfulness. These skills are particularly useful for individuals who engage in binge eating as a way to cope with emotional instability.
- Medications: Although no medication is specifically approved for BED, certain medications like selective serotonin reuptake inhibitors (SSRIs) or the stimulant lisdexamfetamine (Vyvanse) may be prescribed to help reduce binge eating episodes and improve mood.
- Nutritional counseling: A registered dietitian can provide guidance on meal planning, portion control, and developing a balanced relationship with food. Nutritional counseling aims to normalize eating patterns and prevent dietary restrictions that can trigger binge eating.
- Support groups and peer support: Participating in support groups or peer support programs can offer a sense of community and shared understanding. These settings provide a safe space for individuals to discuss their experiences and learn from others who have faced similar challenges.
Effective treatment for BED often involves a combination of these approaches, tailored to the individual's specific needs and preferences. It's important for patients to work closely with their healthcare team to develop a treatment plan that addresses both the psychological and physical aspects of the disorder.
Research on binge eating disorder
Binge eating disorder has been a subject of extensive research, leading to significant advancements in understanding and treating the condition.
A recent study conducted by Derks et al. (2024) has shed light on the relationship between early childhood appetitive traits and the development of eating disorder symptoms in adolescence. The research utilized data from two longitudinal cohort studies, Generation R and Gemini, to explore the longitudinal associations between appetitive traits at age 4-5 years and eating disorder symptoms at age 12-14 years.
The study found that higher food responsiveness in early childhood was associated with an increased likelihood of binge eating symptoms, uncontrolled eating, emotional eating, restrained eating, and compensatory behaviors in adolescence. This suggests that children who exhibit a strong response to food cues may be at a higher risk of developing eating disorder symptoms later in life.
Another groundbreaking study in this field is by Burgess et al. (2016) at the University of Alabama at Birmingham, which explored the potential of transcranial direct current stimulation (tDCS) as a treatment for BED. The study found that tDCS targeting the right dorsolateral prefrontal cortex significantly reduced cravings for sweets, savory proteins, and overall food intake. This brain region is typically underactive in BED patients, and its stimulation may help improve cognitive inhibition and emotional regulation, reducing impulsiveness towards food.
References
Berkman, N. D., Brownley, K. A., Peat, C. M., Lohr, K. N., Cullen, K. E., Morgan, L. C., Bann, C. M., Wallace, I. F., & Bulik, C. M. (2015). Management and outcomes of binge-eating disorder. Comparative Effectiveness Reviews, 160. PubMed. https://www.ncbi.nlm.nih.gov/books/NBK338301/table/introduction.t1/
Burgess, E. E., Sylvester, M. D., Morse, K. E., Amthor, F. R., Mrug, S., Lokken, K. L., Osborn, M. K., Soleymani, T., & Boggiano, M. M. (2016). Effects of transcranial direct current stimulation (tDCS) on binge-eating disorder. International Journal of Eating Disorders, 49(10), 930–936. https://doi.org/10.1002/eat.22554
Burstein, D., Griffen, T. C., Therrien, K., Bendl, J., Venkatesh, S., Dong, P., Modabbernia, A., Zeng, B., Mathur, D., Hoffman, G., Sysko, R., Hildebrandt, T., Voloudakis, G., & Roussos, P. (2023). Genome-wide analysis of a model-derived binge eating disorder phenotype identifies risk loci and implicates iron metabolism. Nature Genetics, 55(9), 1462–1470. https://doi.org/10.1038/s41588-023-01464-1
Derks, I. P. M., Nas, Z., Harris, H. A., Kininmonth, A. R., Treasure, J., Jansen, P. W., & Llewellyn, C. H. (2024). Early childhood appetitive traits and eating disorder symptoms in adolescence: a 10-year longitudinal follow-up study in the Netherlands and the UK. The Lancet Child & Adolescent Health. https://doi.org/10.1016/S2352-4642(23)00342-5
Manfredi, L., Accoto, A., Couyoumdjian, A., & Conversi, D. (2021). A systematic review of genetic polymorphisms associated with binge eating disorder. Nutrients, 13(3), 848. https://doi.org/10.3390/nu13030848
Trace, S. E., Baker, J. H., Peñas-Lledó, E., & Bulik, C. M. (2013). The genetics of eating disorders. Annual Review of Clinical Psychology, 9(1), 589–620. https://doi.org/10.1146/annurev-clinpsy-050212-185546
Commonly asked questions
Binge eating refers to consuming large amounts of food in a short period while feeling a lack of control over eating. Feelings of distress, guilt, or shame often accompany it.
The DSM-5 recognizes three distinct eating disorders: Anorexia Nervosa, Bulimia Nervosa, and binge eating disorder. Each disorder has specific diagnostic criteria and patterns of disordered eating behaviors.
Yes, other specified feeding or eating disorder (OSFED) is in DSM-5. It encompasses eating disorders that do not meet the full criteria for Anorexia Nervosa, Bulimia Nervosa, or binge eating disorder but still cause significant distress or impairment.























-template.jpg)