Fever Nursing Care Plan
Carepatron's free PDF download provides a template for nursing care planning. It helps you understand the nursing diagnoses associated with fever and how to provide adequate care for patients.


What is a fever?
A fever, simply put, is a temporary elevation in the body's temperature beyond the normal range. The body's normal temperature typically hovers around 98.6°F (37°C), but it can vary slightly from person to person. When the body detects a threat, such as an infection, it responds by increasing its core temperature as a defense mechanism.
Infections commonly trigger fevers as many bacteria and viruses struggle to survive at higher temperatures.
Causes of a fever
Several factors can contribute to an elevated body temperature, including bacterial or viral infections, heat exposure, or inflammatory conditions. The hypothalamus in the brain is responsible when the body temperature rises in response to these stimuli.
Below are some common causes of fever:
- Infections: Bacterial, viral, fungal, or parasitic infections can all lead to fever. Examples include influenza, urinary tract infections, pneumonia, and tuberculosis.
- Inflammatory conditions: Inflammation within the body, such as in autoimmune diseases like rheumatoid arthritis or inflammatory bowel disease, can result in fever.
- Heat exposure: Excessive exposure to high temperatures or heat stroke can cause the body's temperature to rise rapidly, leading to fever.
- Medications: Some medications, particularly those that affect the immune system or have known side effects of fever, can induce elevated body temperatures.
- Cancer: Certain types of cancer, such as leukemia or lymphoma, can cause fever as a result of the body's response to the malignancy.
- Vaccinations: Some individuals may experience a low-grade fever as a normal response to vaccines as the body mounts an immune response.
- Increased heat production: This occurs during vigorous physical activity or in cases of certain medical conditions.
Signs and symptoms of a fever
Recognizing the signs and symptoms of a fever is essential for prompt identification and management. Fevers often present with a combination of characteristic indicators. Here are some common signs and symptoms:
- Elevated core body temperature: The most obvious sign of a fever is an increase in body temperature above the normal range, typically measured with a thermometer.
- Chills and shivering: Many individuals with fever experience chills or shivering as their bodies attempt to generate heat to combat the elevated temperature.
- Sweating: As the body works to regulate its temperature, sweating may occur, leading to damp or clammy skin.
- Headache: Fever can often accompany headaches or migraines, contributing to discomfort and malaise.
- Fatigue and weakness: Fever can cause tiredness and weakness, impacting overall energy levels and daily activities.
- Body aches: Muscular discomfort or body aches are common symptoms of fever, often contributing to feelings of soreness or discomfort.
- Loss of appetite: Fever may suppress appetite, leading to decreased food intake and potential weight loss.
- Irritability or confusion: In some cases, particularly in children or older adults, fever may manifest as irritability, confusion, or altered mental status.
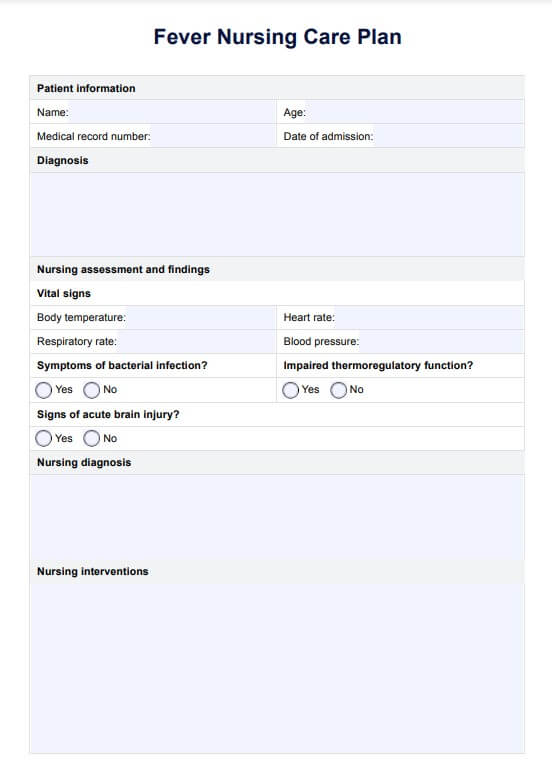
Fever Nursing Care Plan Template
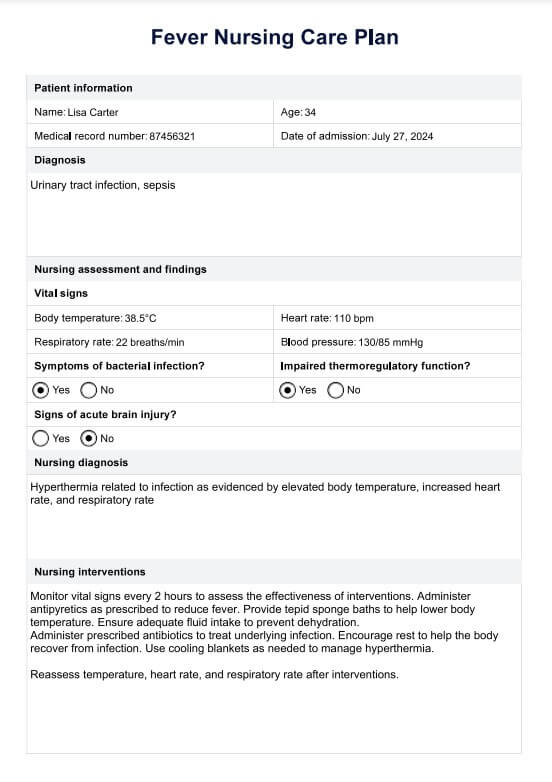
Fever Nursing Care Plan Example
How do nurses assess and diagnose a fever
Assessing and diagnosing a fever is a critical aspect of nursing care. It requires a systematic approach to gathering information and identifying underlying causes. Nurses employ various techniques and tools to assess and diagnose fevers accurately, ensuring appropriate nursing interventions and patient care.
1. Initial assessment
Nurses begin by obtaining a comprehensive health history, including recent illnesses, medications, and exposure to infectious agents. They also assess vital signs, including temperature, heart rate, respiratory rate, and blood pressure. Comparing the patient's temperature to the normal body temperature range provides an initial indication of fever.
2. Temperature measurement
Depending on the patient's age, condition, and clinical setting, nurses use various methods to measure body temperature, such as oral, tympanic, axillary, or rectal thermometers. Obtaining a core temperature, considered the most accurate representation of body temperature, may be necessary for precise nursing diagnosis.
3. Physical examination
A thorough physical examination helps nurses identify additional signs and symptoms of fever, such as chills, sweating, or localized inflammation. Assessing for specific risk factors, such as recent travel or exposure to individuals with infectious diseases, aids in narrowing down potential causes.
4. Diagnostic tests
Depending on the clinical presentation and suspected underlying cause, nurses may order diagnostic tests, such as blood cultures, urinalysis, or imaging studies, to confirm or rule out bacterial infections or other contributing factors.
Next steps
Once a fever is assessed and diagnosed, nurses collaborate with healthcare providers to develop a comprehensive nursing care plan. This plan may include implementing appropriate nursing interventions to manage fever, monitoring vital signs, administering medications as prescribed, and educating patients on fever management and infection control measures. Regular reassessment of the patient's condition is essential to monitor response to treatment and adjust nursing care as needed.
How to use our Fever Nursing Care Plan template?
Our Fever Nursing Care Plan template is designed to assist medical practitioners in efficiently managing and treating patients with fevers. Follow these steps to utilize the template effectively:
Nursing assessment
Conduct a thorough nursing assessment to gather essential information about the patient's condition. Assess vital signs, including body temperature, heart rate, respiratory rate, and blood pressure. Identify any signs or symptoms suggestive of bacterial infection, such as localized inflammation or recent travel history.
Diagnosis and identification of underlying causes
Use the nursing diagnosis section of the template to diagnose the fever and identify potential underlying causes accurately. Consider factors such as impaired thermoregulatory function, bacterial infections, or acute brain injury that may contribute to fever development.
Nursing interventions
Select appropriate nursing interventions to address the patient's fever based on the assessment findings and diagnosis. We'll cover more of this in a later section.
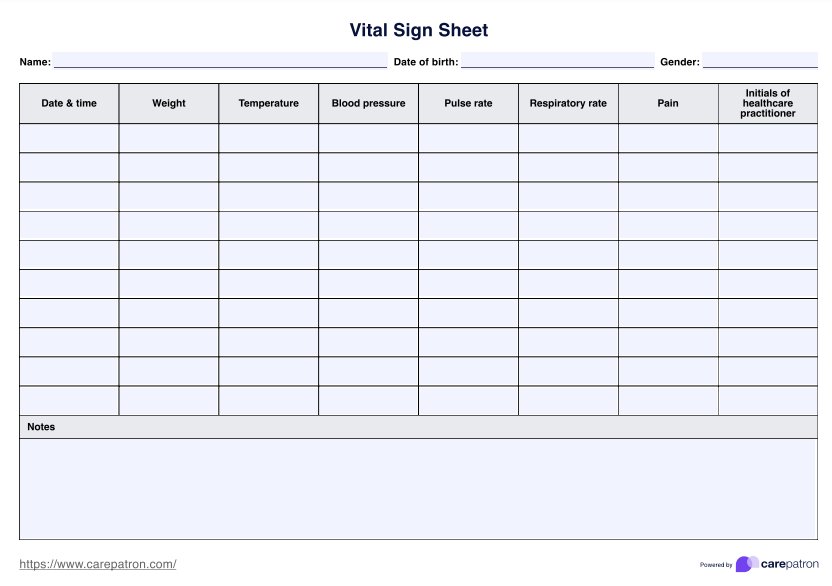
Monitoring and evaluation
Continuously monitor the patient's response to nursing interventions and assess for any changes in symptoms or vital signs. Evaluate the effectiveness of the implemented nursing care plan in reducing fever and improving the patient's overall condition. Monitoring body temperature closely and identifying underlying causes, such as bacterial infections, are crucial aspects of fever management protocols.
Documentation
Thoroughly document all nursing assessments, interventions, and patient responses in the provided sections of the template. This documentation ensures continuity of care and facilitates communication among healthcare team members.
Common nursing interventions for a fever
Nurses play a crucial role in managing fevers and alleviating associated symptoms. Below are common nursing interventions employed in the care of patients with fever:
1. Administering antipyretic medications
Antipyretic medications, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), are often prescribed to reduce fever by lowering the body's temperature. These medications work by inhibiting the production of prostaglandins, which regulate body temperature. Nurses should carefully administer these medications according to the dosage and frequency, considering factors such as the patient's age, weight, and underlying health conditions.
2. Implementing physical cooling methods
Physical cooling methods can help lower body temperature and relieve fever-related discomfort. Tepid sponge baths, where the patient is gently sponge-bathed with lukewarm water, can reduce body temperature. Cooling blankets or packs may also be applied to specific body areas to regulate temperature. Nurses should closely monitor the patient's response to these interventions to prevent overcooling or adverse reactions.
3. Monitoring fluid intake and output
Fever can increase the body's demand for fluids, leading to dehydration if not adequately managed. Nurses should encourage patients to increase their fluid intake to prevent dehydration and maintain fluid balance. Monitoring fluid intake and output, including urine output and signs of dehydration such as dry mouth or decreased skin turgor, is essential. Intravenous (IV) fluid therapy may be necessary for patients unable to maintain adequate oral hydration.
4. Assessing for underlying causes
Identifying and addressing the underlying cause of the fever is essential for effective management. Nurses should conduct a thorough nursing assessment to evaluate signs and symptoms suggestive of bacterial or viral infections, inflammatory conditions, or other contributing factors. Diagnostic tests, such as blood cultures or imaging studies, may be ordered to confirm the diagnosis and guide treatment.
5. Providing comfort measures
Fever can be accompanied by chills, headache, muscle aches, and fatigue, significantly impacting the patient's comfort and well-being. Nurses should implement comfort measures, such as providing extra blankets for chills, administering pain relief medications for headaches and muscle aches, and ensuring a quiet and restful environment to promote relaxation and healing.
6. Educating patients and caregivers
Patient and caregiver education is crucial for empowering individuals to manage fever effectively at home and prevent complications. Nurses should provide information on fever management strategies, including when to seek medical attention, how to monitor for signs of worsening symptoms, and the importance of adhering to prescribed treatments. Education should be tailored to the patient's specific needs and preferences to ensure comprehension and adherence.
Benefits of having comprehensive care plans
Comprehensive care plans are essential tools in healthcare settings, providing structured guidelines for delivering high-quality patient care. Here are the benefits of having comprehensive care plans:
1. Improved patient outcomes:
Comprehensive care plans facilitate coordinated and holistic care delivery, improving patient outcomes. By addressing multiple aspects of patient care, including medical, nursing, and psychosocial needs, these plans help optimize treatment effectiveness and promote faster recovery.
2. Enhanced communication and collaboration:
Care plans serve as communication tools, ensuring that all healthcare team members are aware of the patient's goals, preferences, and care requirements. This promotes seamless collaboration among healthcare providers, leading to more efficient care delivery and reduced risk of errors or omissions.
3. Personalized care delivery:
Comprehensive care plans are tailored to each patient's individual needs and preferences, allowing for personalized care delivery. By considering factors such as the patient's medical history, cultural background, and social support network, these plans ensure that interventions are relevant and practical, enhancing patient satisfaction and engagement in care.
4. Standardization of care practices:
Care plans provide standardized guidelines for evidence-based care, promoting consistency and quality across healthcare settings. These plans help ensure that all patients receive optimal care regardless of the care provider or setting by outlining recommended interventions, assessments, and monitoring parameters.
5. Efficient resource utilization:
Comprehensive care plans help optimize resource utilization by guiding the allocation of healthcare resources based on patient needs and priorities. By identifying necessary interventions and monitoring parameters upfront, these plans minimize unnecessary testing, procedures, and hospital stays, leading to cost savings and improved healthcare efficiency.
Commonly asked questions
Firstly, they administer antipyretic medications, such as acetaminophen or ibuprofen, to reduce body temperature and alleviate discomfort. Additionally, nurses implement physical cooling methods, such as tepid sponge baths or the application of cooling blankets, to assist in temperature reduction.
A common nursing diagnosis for fever is "risk for imbalanced body temperature" related to the body's inability to regulate temperature due to infection or inflammation. However, nursing diagnoses are not as commonly used in real-life clinical settings today.
Nursing interventions for yellow fever include supportive care to manage symptoms such as fever, nausea, and vomiting, ensuring adequate hydration and fluid balance, and monitoring for signs of complications such as liver damage or hemorrhage.