Cardiac Output Equation
Ensure you show your work correctly with our handy Cardiac Output Equation PDF for simple calculations involving stroke volume and heart rate.


What is cardiac output?
Cardiac output is the volume of blood ejected by the left ventricle into the aorta per minute. It is a crucial measure of the cardiovascular system's ability to deliver oxygen-rich blood to tissues and organs. Normal cardiac output ranges from 4 to 8 liters per minute (L/min) in a healthy individual at rest (Klabunde, 2012).
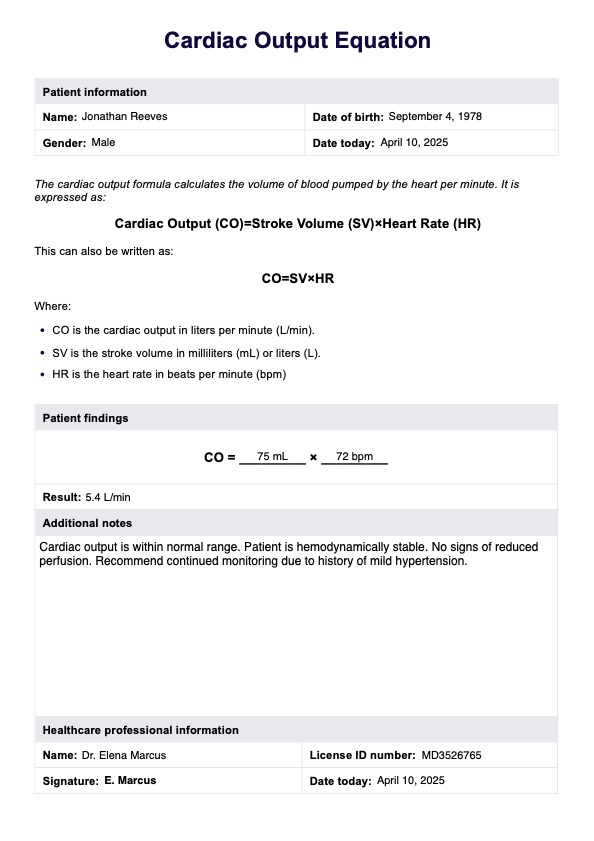
Cardiac Output Equation Template
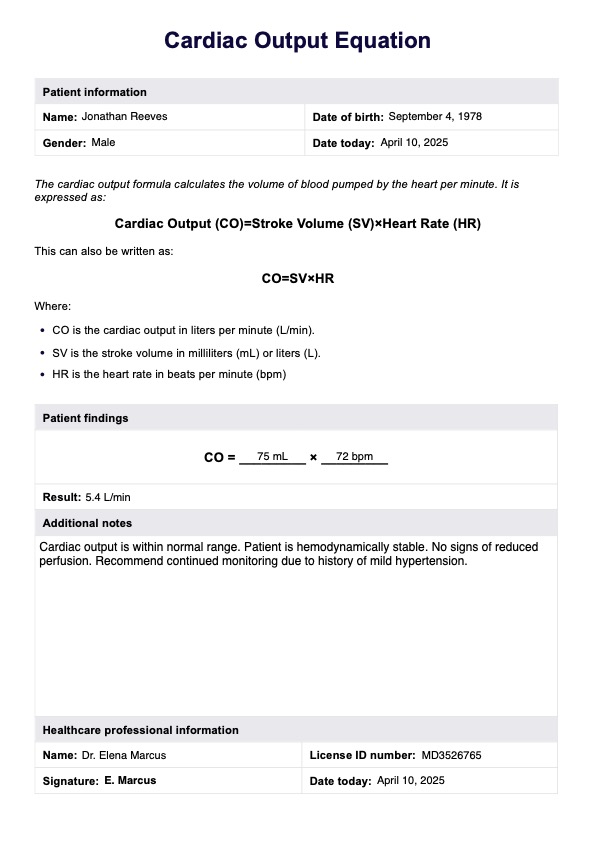
Cardiac Output Equation Example
How do you calculate cardiac output?
To calculate cardiac output, you need to know the heart rate and stroke volume. Heart rate is the number of heartbeats per minute, while stroke volume is the amount of blood ejected by the left ventricle during each contraction. Stroke volume is influenced by factors such as preload (the amount of blood returning to the heart), afterload (the resistance against which the heart must pump), and contractility (the heart muscle's ability to generate force) (Hall & Hall, 2021).
The cardiac output equation is a fundamental concept in cardiovascular physiology that helps us understand and quantify the heart's performance. Cardiac output (CO) refers to how much blood the heart pumps per minute, and it is determined by two factors: heart rate (HR) and stroke volume (SV). The equation is expressed as:
Cardiac Output (CO) = Heart Rate (HR) × Stroke Volume (SV)
Cardiac index
The cardiac index is another important measure related to cardiac output. The cardiac output is normalized for body surface area, expressed in liters per minute per square meter (L/min/m²). This adjustment accounts for differences in body size, making it easier to compare cardiac output values across individuals (Klabunde, 2012).
Fick method
Several methods are available for measuring cardiac output, each with advantages and limitations. The most accurate method is the Fick principle, which involves measuring the oxygen consumption and the difference in oxygen content between arterial and venous blood.
The Fick equation for calculating cardiac output is:
Cardiac Output = Oxygen Consumption / (Arterial Oxygen Content - Venous Oxygen Content)
Oxygen consumption is the amount of oxygen utilized by the body's tissues per minute. It can be measured directly by analyzing the inhaled and exhaled air or estimated based on the individual's age, sex, and body surface area.
Arterial oxygen content represents the amount of oxygen the blood carries from the lungs. In contrast, venous oxygen content represents the amount of oxygen in the blood returning to the lungs. These values are obtained by taking arterial and venous blood samples and analyzing the oxygen saturation and hemoglobin concentration.
To measure cardiac output using the Fick method, the following steps are typically followed:
- Measure the patient's oxygen consumption.
- Obtain arterial and venous blood samples.
- Analyze the blood samples for oxygen content and hemoglobin concentration.
- Substitute the values into the Fick equation to calculate cardiac output.
To calculate the cardiac output using this method, check out this comprehensive Fick Equation Cardiac Output, optimized for printed and digital use.
What is the normal cardiac output?
The normal range of cardiac output in a healthy individual at rest is typically between 4 and 8 liters per minute (L/min) (Klabunde, 2012). However, cardiac output and blood pressure can vary based on several factors, including age, body size, physical activity level, and overall health status.
A higher cardiac output is often observed in certain situations or conditions where the body's demand for oxygen and nutrients increases. Some scenarios that may lead to a higher cardiac output include:
- Exercise: During physical activity, the body requires more oxygen and nutrients to be delivered to the muscles, resulting in an increased cardiac output to meet these demands.
- Pregnancy: Pregnant women typically have a higher cardiac output to support the growing fetus and the additional metabolic demands of pregnancy.
- Fever: In response to a fever, the body's metabolic rate increases, leading to a higher cardiac output to meet the increased oxygen and nutrient demands.
- Anemia: In cases of anemia, where there is a reduced number of red blood cells or hemoglobin, the heart may pump more blood to compensate for the decreased oxygen-carrying capacity.
It's important to note that while a higher cardiac output may be a normal physiological response in certain situations, an excessively high or persistently elevated cardiac output can also be a sign of underlying cardiovascular conditions, such as heart failure or sepsis, and may require medical attention.
Clinical significance and application
Measuring cardiac output holds significant clinical importance when looking into the condition of a patient's cardiovascular system. This provides insights into the heart's pumping ability and the body's circulatory dynamics. Cardiac output measurement can then guide diagnostic and therapeutic decisions.
Systemic vascular resistance
When combined with systemic vascular resistance and arterial pressure assessments, cardiac output measurements can reveal valuable information about the overall hemodynamic status. In conditions like hypertension or vascular disorders, these parameters aid in understanding the relationship between blood flow, resistance, and pressure within the systemic circulation (Rowland, 2005).
Pulmonary blood flow
Calculating this can also shed light on blood flow dynamics in the pulmonary artery and right heart function. In conditions affecting pulmonary circulation, such as pulmonary hypertension or lung diseases, cardiac output measurements can provide insights into the right ventricle's ability to pump blood effectively into the pulmonary vasculature.
Cardiac function
Cardiac output measurements, combined with assessments of end-diastolic volume (EDV) and end-systolic volume (ESV), can be used to calculate essential parameters like ejection fraction (EF). EF is a crucial indicator of the heart's pumping efficiency and cardiovascular function and can aid in evaluating various cardiac conditions, such as heart failure or cardiomyopathies (Pinsky, 2003).
Circulatory system
Determining cardiac output is crucial for maintaining proper perfusion and oxygen delivery to vital organs, including the central nervous system, kidneys, and other tissues. This helps healthcare professionals better understand the circulatory system's ability to meet the body's metabolic demands and ensure optimal organ function.
Valvular heart diseases and arrhythmias
In conditions like aortic stenosis, where the heart must pump against increased resistance, cardiac output measurements can quantify the impact on the heart's workload and pumping capacity. Similarly, in arrhythmias like atrial fibrillation, assessing cardiac output can help evaluate the heart's ability to maintain adequate blood flow despite irregular rhythms (Kresoja et al., 2019).
Arterial compliance
Arterial compliance, which refers to the elasticity and distensibility of arteries, can influence cardiac output and blood flow dynamics. Measuring arterial pressure, such as through radial artery assessment, can provide additional context for interpreting cardiac output measurements and understanding the interplay between central and peripheral circulation.
How does it work?
Feel free to utilize this editable cardiac output formula, which can be digitally filled, printed, and completed by hand. Follow these steps to ensure accurate cardiac output calculations every time:
Step 1: Enter the end-diastolic volume (EDV)
If you already have the stroke volume value, skip to step four and enter it in the SV box of equation two. Otherwise, input the end-diastolic volume (EDV) in milliliters into the designated EDV box in equation one.
Step 2: Enter end-systolic volume (ESV)
Next, insert the milliliter end-systolic volume into the ESV box in equation one.
Step 3: Calculate stroke volume
Once you have the EDV and ESV filled in in equation one, subtract the ESV from the EDV to give you a value for stroke volume in milliliters.
Step 4. Copy the stroke volume into equation two (in liters)
Watch out for the units on this one! The next step is to copy the stroke volume value into the SV box in equation two but in liters.
Step 5: Enter heart rate
In equation two, input the heart rate value in beats per minute (bpm) into the HR box.
Step 5: Calculate cardiac output
The final step involves multiplying the stroke volume and heart rate, or the values in the HR and SV boxes in equation two. This computation will yield the cardiac output in liters per minute.
What do the results mean?
It's good to remember that when assessing a patient's cardiac health, relying on a single number doesn't give the whole picture. Cardiac output is incredibly dynamic and can be influenced by various factors like exercise, hormones, or even body temperature. This means that each person will have a unique baseline for heart function, and what's considered normal can vary widely.
A commonly cited stroke volume for a healthy adult hovers around 70mL per beat. Combined with a typical resting heart rate ranging from 60 to 80 beats per minute, you get a ballpark figure for 5 liters per minute cardiac output. However, these values are just averages, and individual values can fall anywhere within this spectrum.
If a healthy individual's cardiac output is lower than expected, it could signal an underlying heart condition like congestive heart failure or cardiomyopathy. Alternatively, a higher-than-expected cardiac output might be due to factors like hyperthyroidism, stress, or just the aftermath of a rigorous workout.
This underscores the importance of not taking a solitary cardiac output value at face value; it needs to be considered in the broader context to understand if there's an underlying health issue. So, the next time you look at cardiac output numbers, remember, it's not just about the digits—it's about the story they're telling in the context of a person's overall health.
Applying this medical record template can enhance your practice and client achievements. It guides clients in establishing actionable steps for their improvement.
References
Hall, J. E., & Hall, M. E. (2021). Guyton and Hall textbook of medical physiology (14th ed.). Elsevier - Health Science.
Klabunde, R. E. (2012). Cardiovascular physiology concepts (2nd ed.). Lippincott Williams & Wilkins.
Kresoja, K. P., Faragli, A., Abawi, D., Paul, O., Pieske, B., Post, H., & Alogna, A. (2019). Thermodilution vs estimated Fick cardiac output measurement in an elderly cohort of patients: A single-centre experience. PloS One, 14(12), e0226561. https://doi.org/10.1371/journal.pone.0226561
Pinsky M. R. (2003). Why measure cardiac output? Critical Care, 7(2), 114–116. https://doi.org/10.1186/cc1863
Rowland, T. W. (2005). Circulatory responses to exercise. Chest, 127(3), 1023–1030. https://doi.org/10.1378/chest.127.3.1023
Commonly asked questions
End-systolic volume (ESV) and end-diastolic volume (EDV) are measures of the amount of blood in the left ventricle at the end of systole (contraction) and diastole (relaxation), respectively. ESV represents the volume of blood remaining in the ventricle after ejection, while EDV represents the total blood volume before contraction.
Cardiac output equations calculate the blood pumped by the heart per minute, a crucial measure of cardiovascular function. These equations help assess the heart's ability to deliver oxygen-rich blood to the body's tissues and organs, and they are used in clinical practice to evaluate and monitor various cardiovascular conditions.
The time required to calculate cardiac output using an equation depends on the method used to obtain the necessary input values, such as heart rate and stroke volume. If these values are readily available, the calculation takes only a few seconds. However, the process may take longer if additional measurements or tests are required, such as blood sampling or imaging techniques.