Asthma Action Plans
Asthmatics should always have a written/printed asthma action plan so they can assess the severity of their asthma and take the appropriate action! Here is an example of what one would normally look like!


What is an Asthma Action Plan?
Asthma Action Plans are battle plans written by pulmonologists, allergists, and other related healthcare practitioners to help asthmatics combat the severity of their asthma! These plans usually provide you with information on how an asthmatic can determine the severity of their asthma and provide instructions on how to deal with it based on the severity.
If you have never written an Asthma Action Plan before (perhaps you have just started your practice), this guide will show you what one would normally look like. If you’ve been treating asthma for a long time, perhaps you might want to check this template out for a more organised and concise version to imitate or use. This one is based on the Asthma Action Plan that was created by the Asthma and Allergy Foundation of America.
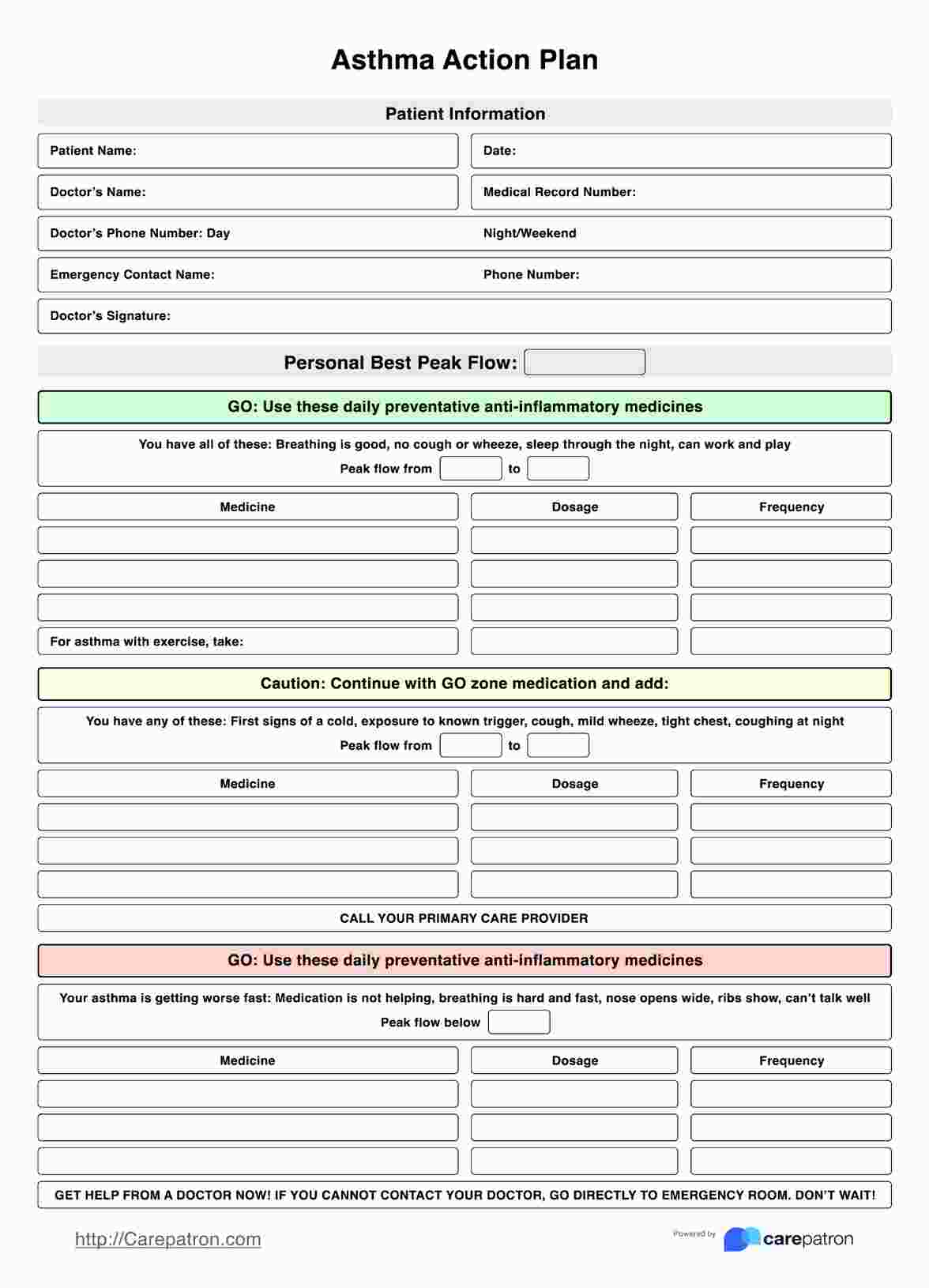
Asthma Action Plans Template
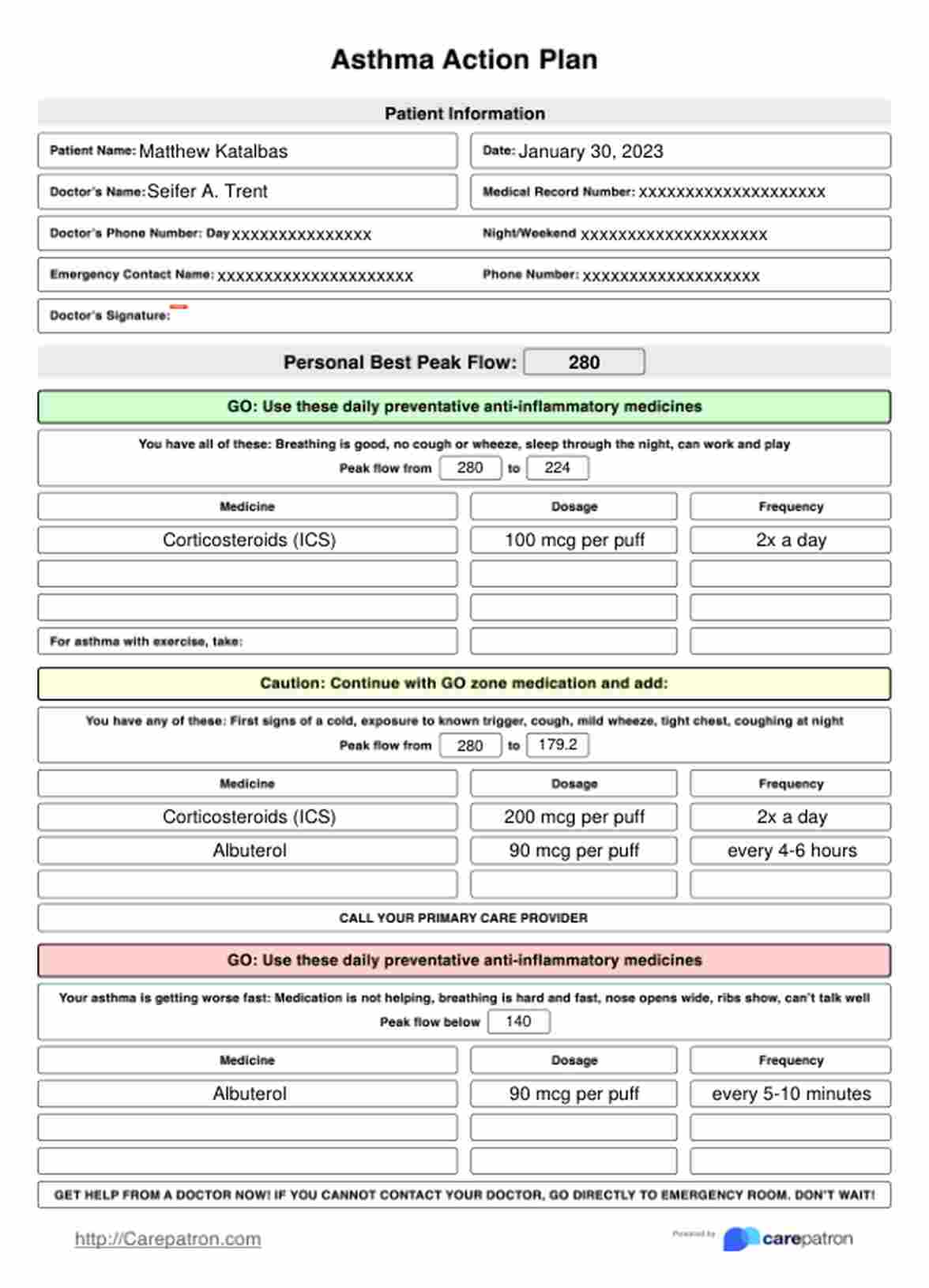
Asthma Action Plans Example
How to use this Asthma Action Plan:
Write down basic information regarding your patient and yourself.
Let’s say that a parent and her child visit you to have the child checked for their asthma (they are already diagnosed). They visit you to get an asthma action plan to get a headstart before something triggers it or they enter the season when their asthma is usually active. The first thing that you have to fill up on this template is basic information regarding you and your patient:
- Your patient’s full name
- The date of their consultation with you
- Your full name
- The asthma action plan document’s medical record number
- Your contact number during the day
- Your contact number at night/during the weekend
- The patient’s emergency contact and contact number
- Your signature
While these are just basic things you’d find on almost any medical document, these are necessary in case of emergencies. Asthmatics should always have their Asthma Action Plans ready wherever they may be.
Let’s say the child is at school, or an adult with asthma is at the office. Their teachers/peers can contact both the doctor and the emergency contact in case the child/adult’s asthma triggers and it’s severe.
Tell the patient about the severity levels.
One of the most noticeable parts of this free Asthma Action Plan is its severity indicator. It’s color-coded based on a traffic light!
Green means “GO!” This means that, despite the asthma being active, they are still well. The patient still has good breathing, is not coughing or wheezing, can sleep well, and can work and play without problems! Those in the Green Zone still need to take preventative medicine to make sure to stop asthma in its tracks before it gets any worse.
Yellow signals “CAUTION!” Patients who fall on this severity level have been exposed to their triggers, they develop the first signs of having a cold or they already have a cold, they cough (even at night), they have mild wheezes, and their chest tightens every now and then when they cough. Patients need to take their preventative medicines alongside other prescribed medications to help curb asthma’s effects.
Red is bad because it signifies “DANGER!” If your patient falls on this severity level, well, that’s not good! This means that preventative medicines and additional medicines are not working, the patient is having a hard time breathing (they breathe hard and fast), their nose opens wide, they can’t talk well, they wheeze more than normal, and they feel like something is strangling them while they cough. Patients in the Red Zone need to see a doctor. IMMEDIATELY.
Now that your patient knows about the severity levels, how do you determine which zone they’re at?
Peak Flow Test time!
In order to determine the severity level of their asthma, you must first write down their best Peak Flow result. You’re going to have to administer the test to them to get a baseline!
Here’s what you need to do:
- Grab a Peak Flow Meter and set the number to 0
- Hand the meter to your patient
- Have your patient stand up and inhale deeply
- While they’re holding their breath, have them place the meter between their teeth while their lips are sealed
- Have them blow out as hard and fast as they possibly can
- Write down the number result they got
- Have them do this two more times
- Then write the best result on the Personal Best Peak Flow field
Tell your patient (and their guardian/companion if they tagged along) to purchase a Peak Flow Meter for them to use at home, school, or the office so they can determine their asthma severity when the asthma triggers.
Fill out the zones!
The Asthma Action Plan template has preset sections for all three zones. Which zone the patient falls will depend on the following:
- Green Zone: if their Peak Flow hits 80% or more of their Personal Best Peak Flow
- Yellow Zone: if their Peak Flow hits between 50% - 79% of their Personal Best
- Red Zone: if their Peak Flow falls below 50% of their Personal Best
Each zone has a segment that says: “Peak Flow: from ________ (Personal Best) to _________ (their current Peak Flow).” Make sure to (have them) fill in the blanks.
You must also write down the medication they need to take for each zone, stating the specific medicine and their dosage as well as when/how often they have to take them.
For the Green Zone, you must list the preventative medicine they should use, especially when they exercise or do anything physically demanding.
For the Yellow Zone, they have to follow the medication listed for the Green Zone, but you have to list down additional medication they need to take. There’s also a default “Call your primary care provider” written on it.
As for the Red Zone, list what they need to take under “Take the following medicines and call your doctor NOW.”
And that pretty much covers the plan! Just remind them to follow the medication and the prompts depending on the zones and make copies they can take to school or work.
When does one typically use an Asthma Action Plan?
On the part of the healthcare practitioner, you fill this out when a patient consults with you about their asthma. Always have copies ready to be filled so you can complete a plan as you discuss things with your patient.
On the part of the patient, they will use this every time their asthma has triggered. They will act based on the zones they are in.
Who can use this printable Asthma Action Plan?
The following healthcare practitioners can use this printable Asthma Action Plan:
- Pulmonologists
- Pulmonary rehabilitation therapists
- Allergists
- Immunologists
- Pediatricians
So long as they specialize in treating asthma and are certified experts, they can make use of this plan.
Anyone with asthma will engage with this plan the most because they will follow the prompts and medication indicated by their doctors whenever their asthma is active.

What are the benefits of using this Asthma Action Plan?
It’s straightforward and easy to use!
The structure is set and the information needed is specific, so doctors don’t have to think about how to structure the Asthma Action Plan they want to use for their patients. Simply use this template, and you are good to go!
It gives the patient clear instructions for each zone.
Patients who receive an Asthma Action Plan that uses this template will be able to understand things clearly given that it is straightforward in its presentation. After self-administering a Peak Flow Test, they will know what to do depending on their zone.
Do they simply need to use preventative medicine? Do they need to use additional medicine? Are they in danger and need to see a doctor immediately?
These are the questions that are immediately answered by the Asthma Action Plan because the doctor already accounted for each severity level.
Patients can take it anywhere!
Whether the patient goes to school, work, or both, they can take their filled-out Asthma Action Plan anywhere. In the event that their asthma triggers while they’re in school or the office, and the zone they are in based on the Peak Flow Test is the Red Zone, their teachers, classmates, or colleagues can contact the patient’s doctor and/or emergency contact. And if those two contacts are not responding or cannot be reached for some reason, the prompt for this zone tells the patient to go to an emergency room immediately.
Commonly asked questions
Asthma Action Plans are highly reliable because they cover different severity levels, which are backed up and informed by Peak Flow Tests. Asthmatics will highly benefit from using Asthma Action Plans because they will know exactly what they need to take and do depending on the severity of their asthma.
No. While the medication will likely be the same, it’s still always best to base your medication choices for your patient on their tests and discussions with you. Some people require Albuterol, some don’t. Some people need to be nebulized, while some don’t. Also, the information in the sample was written for a fictional patient for demonstrative purposes only. It really is best not to copy the sample texts.
Yes. This will depend on the patient. If they have a severe asthma attack and the medication you listed down isn’t working at all (especially the ones listed specifically for the Red Zone), then you might have to adjust the dosages, change the prescribed medications to see if those work, or even employ the use of other means to treat lungs, like nebulizers.







-template.jpg)