SBAR Nursing Handoff Template
Make improving patient outcomes simple with the SBAR Nursing Handoff Template. Download it for free and incorporate it into your practice today!


What is the SBAR nursing handoff technique?
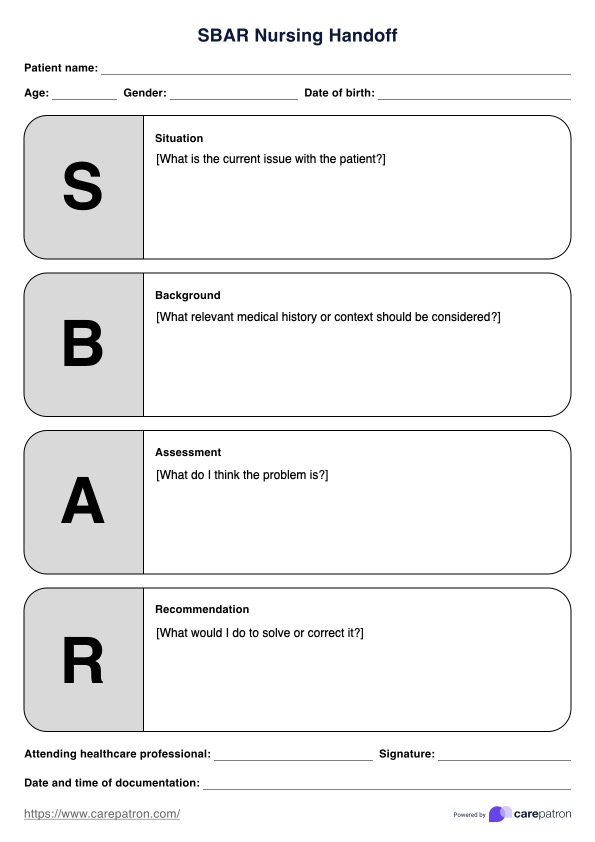
The SBAR Nursing Handoff technique is a communication tool that allows healthcare team members to provide essential, concise information about an individual's condition in an easy-to-remember way. SBAR stands for Situation, Background, Assessment, and Recommendation. Here's what's usually considered in each section:
- Situation (S): This section covers the patient's current issue. You can also include a brief introduction of yourself.
- Background (B): This may include admitting diagnosis, past medical history or context, and the date and time of admission.
- Assessment (A): The assessment reports what the SBAR communicator identifies as the problem based on background information, patient history, and observations.
- Recommendation (R): Recommendations include the initial suggestion, needed actions with timing, and confirming the provider's response for accuracy.
The SBAR technique was initially developed to facilitate communication between rapid response teams and other healthcare professionals. It has been widely recommended as a standardized handover method to improving patient safety, patient outcomes, and nurse satisfaction. SBAR has been shown to improve handover quality, particularly for telephonic handovers, and to increase communication satisfaction among healthcare providers.
SBAR Nursing Handoff Template
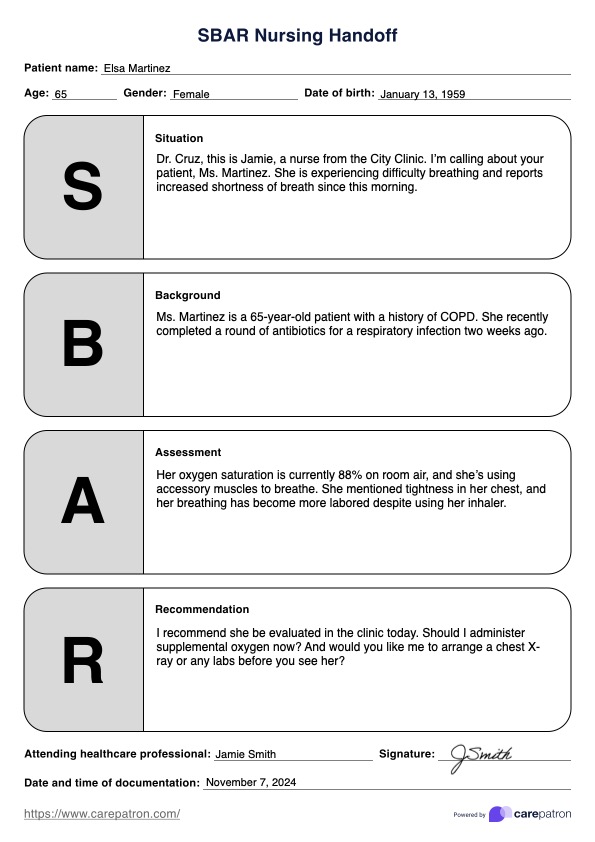
SBAR Nursing Handoff Template Example
How does this SBAR Nursing Handoff Template work?
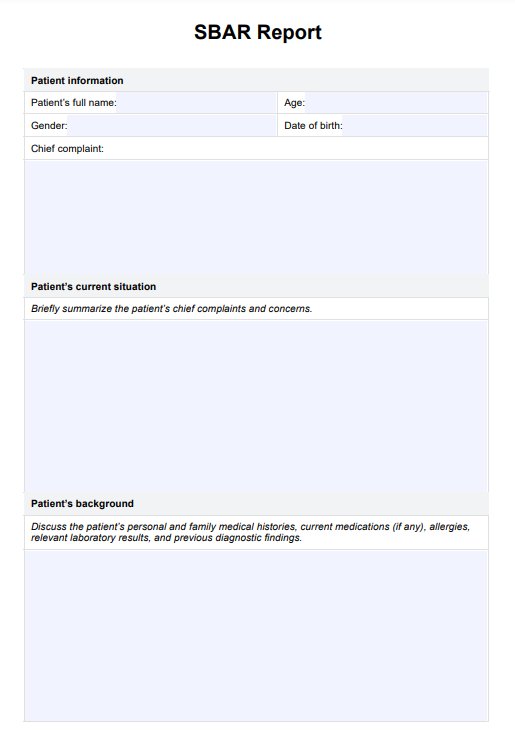
SBAR templates are helpful in different clinical settings, such as hospitals, rehabilitation centers, and nursing homes. They have significantly improved communication between nurses, physicians, and other healthcare providers, improving patient's care and outcomes. Here's how to incorporate the SBAR communication technique into your practice:
Step 1: Download the template
Begin by downloading the SBAR Nursing Handoff Template. A structured form can help you organize and deliver important details about the patient's current status, medical history, and care needs.
Step 2: Fill in each section with key details
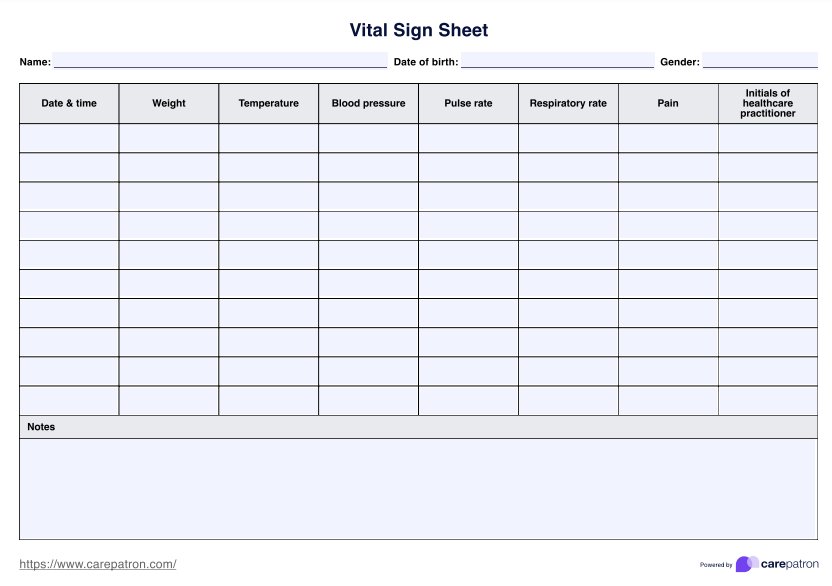
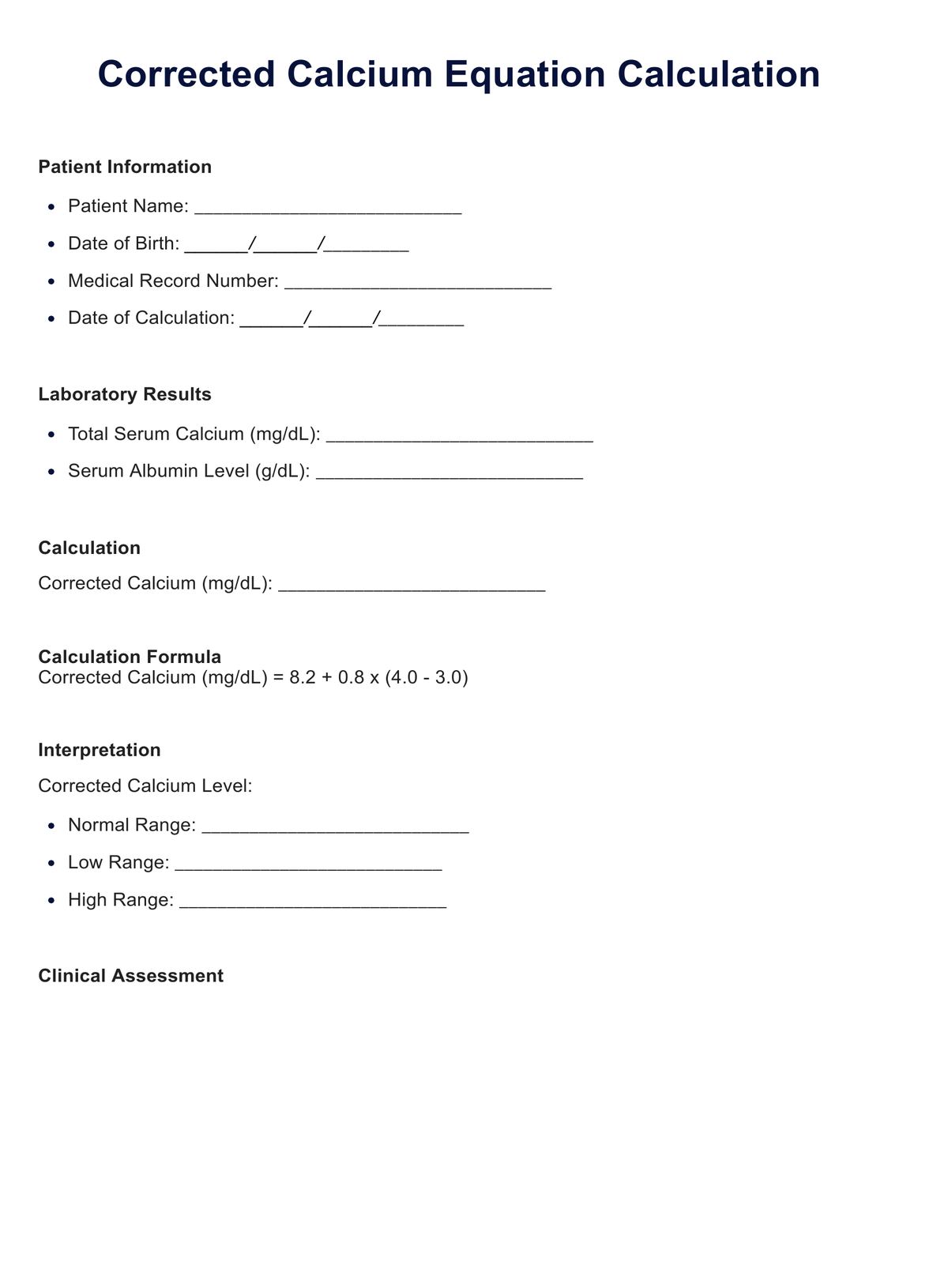
Begin by briefly describing the patient's current condition and the reason for calling or transferring care. Include essential details such as the patient's name, age, code status, and primary concern (e.g., patient's vital signs and symptoms).
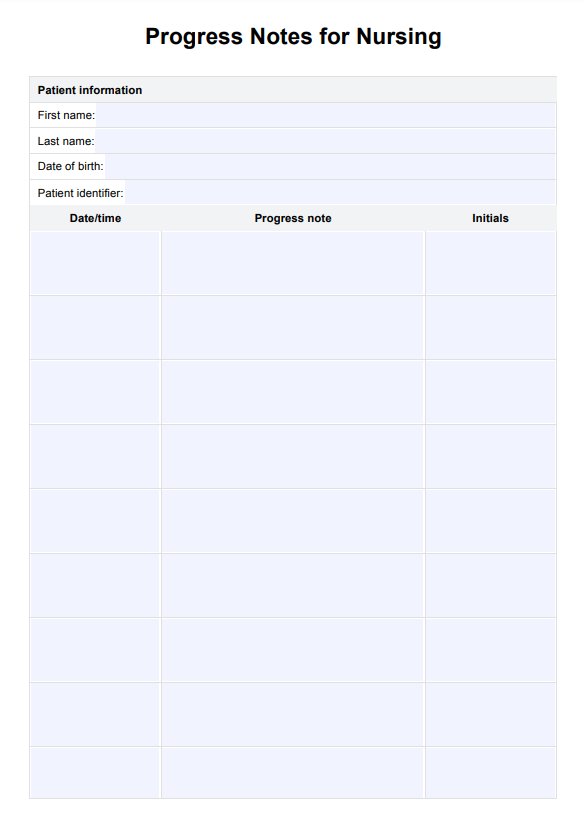
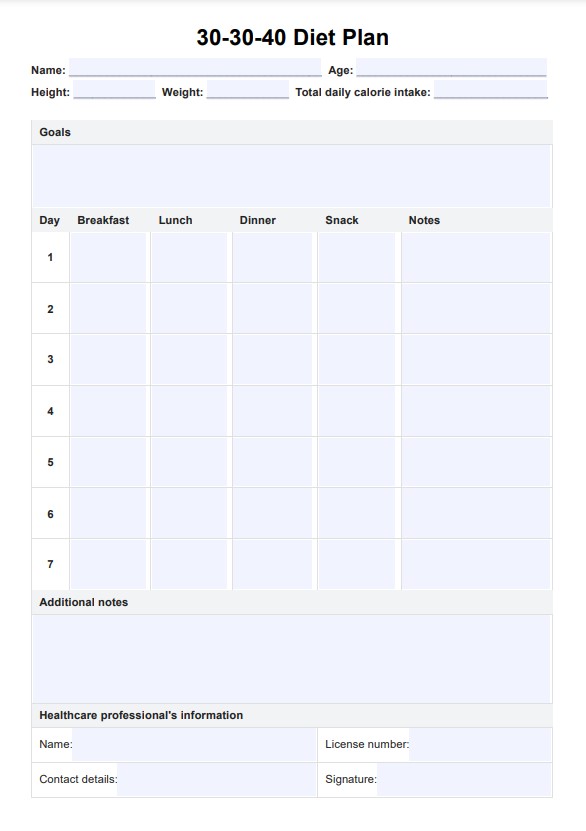
Next, summarize the patient's relevant medical history and recent treatments to contextualize their situation. Then, share your clinical findings, including any physical assessments, diagnostic tests, or observations that clarify the patient's status. Conclude with your recommendation for the next steps in the patient's care, confirming that the receiving provider understands and agrees with the plan.
Step 3: Confirm the handoff details
After completing the SBAR template, review it with the receiving provider or team to confirm that all information is accurate and understood. Repeat critical points as needed to avoid misunderstandings, and document the handoff for future reference.
When can you use the SBAR handoff template?
Here are some contexts where SBAR is especially beneficial in improving communication:
When facilitating handoffs and transfers
The SBAR Template is handy during handoffs and transfers of patient care between different healthcare providers or shifts.
Emergencies
In emergencies such as cardiac events or situations requiring immediate attention, the SBAR communication tool facilitates rapid communication. Healthcare providers can quickly understand the problem, assess vital signs, and implement necessary interventions.
Medication management
SBAR is valuable for managing medications, especially when patients are on antihypertensive drugs or have a history of taking daily medication.
Routine healthcare procedures
In standard healthcare procedures like ordering labs, maintaining a nursing care plan, or ensuring a regular diet, SBAR provides a standardized framework for communication.
Benefits of SBAR Nursing Handoff Template
The SBAR technique enhances communication and collaboration among healthcare team members in several ways:
Standardized communication
SBAR provides a structured framework for sharing information about a patient's condition, ensuring that essential details are communicated clearly and organized.
Concise expression of concerns
It allows individuals to express concerns concisely, making it particularly useful for critical situations that require immediate attention, such as when a patient's condition is rapidly deteriorating.
Interdisciplinary communication
SBAR communication promotes effective communication among healthcare professionals, including doctors, nurses, and other team members, leading to better collaboration and patient care.
Improved patient safety
SBAR facilitates standardized and clear communication, reducing the risk of miscommunication and errors and ultimately contributing to improved patient safety and outcomes.
Commonly asked questions
Yes, Situation, Background, Assessment, Recommendation (SBAR) is a mnemonic designed to structure information sharing during handoffs. This helps prevent communication failures and ensures a comprehensive exchange of vital details.
When giving a nursing handoff report using SBAR, identify yourself, the calling site nurse, the doctor, and the affected individual with their name and date of birth. State the reason for concern and details about symptom onset and severity.
In nursing and health care, a handoff refers to the crucial transfer of essential information and the responsibility for a patient's health care from one healthcare provider to another. This process is a pivotal component of effective communication within the healthcare system.