Anaphylaxis can cause respiratory distress, such as wheezing, shortness of breath, and swelling, often in the throat. Healthcare providers should assess cardiovascular status for symptoms like rapid pulse and low blood pressure. Early recognition is key to preventing further complications, such as cardiovascular collapse.
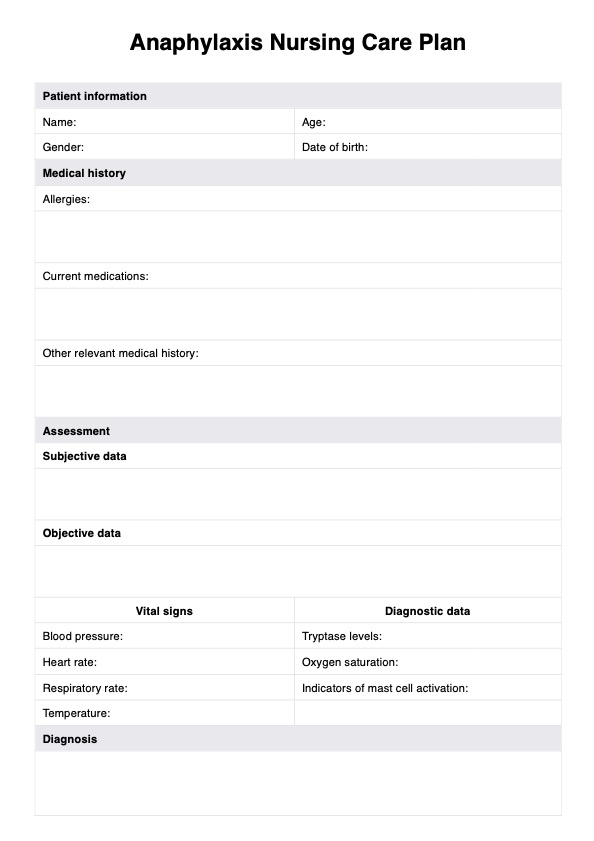
Anaphylaxis Nursing Care Plan
Explore effective anaphylaxis management strategies, symptoms, causes, and essential nursing interventions in our detailed guide.
Anaphylaxis Nursing Care Plan Template
Commonly asked questions
Epinephrine should be given immediately at the first sign of anaphylaxis. It helps reverse histamine-induced bronchospasm, improving breathing and stabilizing blood pressure. Quick administration prevents severe respiratory distress and cardiovascular collapse.
Yes, food allergies can cause anaphylaxis in adults. Common triggers like peanuts or shellfish may lead to respiratory distress and swelling. Immediate treatment with epinephrine is necessary to reverse histamine-induced bronchospasm and stabilize the patient’s condition.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments