Symptom Severity Scale
Access our free Symptom Severity Scale to assess, track, and manage symptom intensity effectively. A concise, reliable tool for better patient care and monitoring.


What is a Symptom Severity Scale (SSS) ?
A Symptom Severity Scale (SSS) is a structured tool designed to help healthcare professionals assess, quantify, and monitor the severity of symptoms reported by patients. This concise tool enables a systematic approach to understanding a patient’s physical, emotional, and functional experiences by assigning numerical values to each symptom based on its intensity, frequency, and impact on their daily life. The scale typically ranges from 0 to 10, where 0 represents no distress and 10 signifies severe distress. This standardized scoring system ensures consistent documentation, facilitates interpreting symptom severity scores, and enhances communication between patients and healthcare providers.
The primary purpose of our SSS is to enhance patient-centered care by providing a detailed snapshot of the patient’s symptom burden at a given time. It enables practitioners to assess and track symptoms, monitor symptom progression, identify patterns or triggers, and evaluate the effectiveness of treatments. Specific symptom categories such as pain, fatigue, nausea, and sleep disturbances are often included to capture a comprehensive picture of the patient’s well-being.
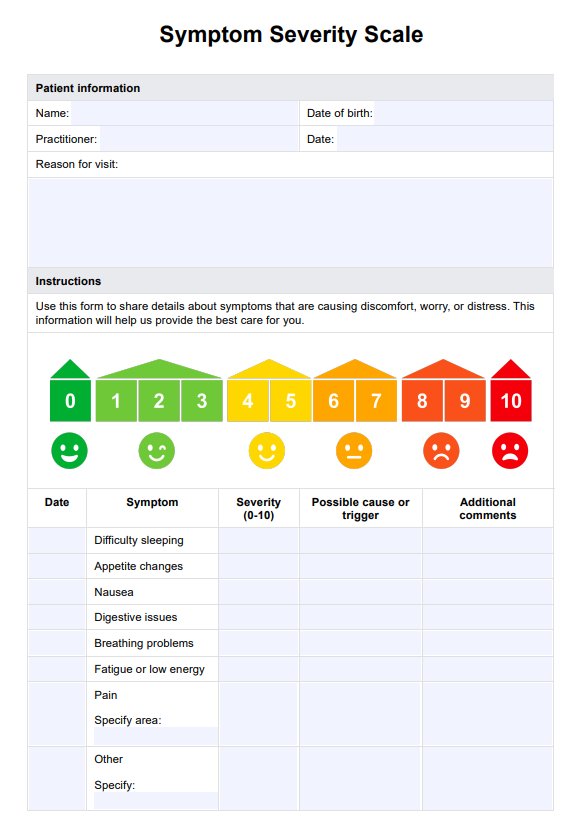
Symptom Severity Scale Template
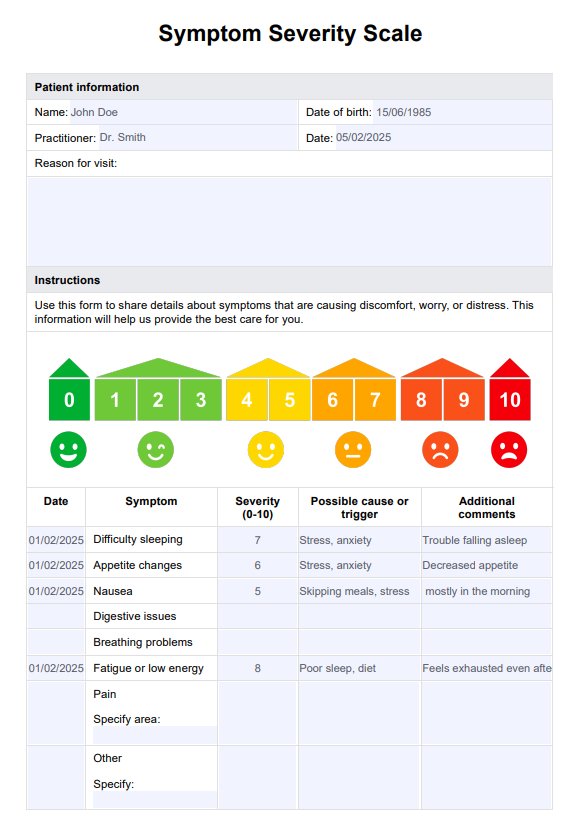
Symptom Severity Scale Example
How to use our Symptom Severity Scale?
Our Symptom Severity Scale template uses a general visual analog scale (VAS) to help your patients accurately communicate the intensity of their symptoms. Follow thes steps to use the template:
Step 1: Access the SSS template
The Symptom Severity Scale template is available as a customizable form within this guide. Click “Use template” to open it in the Carepatron app, where you can modify it to meet your specific requirements. Alternatively, a fillable PDF version can be downloaded for use in physical or digital formats.
Step 2: Introduce the SSS to the patient
At the start of the session or consultation, explain the purpose and structure of the Symptom Severity Scale. Highlight that the scale is designed to assess the severity of symptoms experienced by the patient on a scale from 0 to 10, with 0 indicating no distress and 10 indicating severe distress.
Step 3: Guide the patient through the SSS
Provide clear instructions on how to complete the scale. Explain that patients should rate each listed symptom based on its impact on their well-being and record the severity using the numeric scale provided. For symptoms not listed, they can use the “Other” section to document additional concerns. Ensure patients understand that they can include possible triggers or additional comments in the relevant sections to provide further context.
Step 4: Review and reflect on responses
After the patient completes the scale, review the responses to ensure all sections are filled out accurately. Where appropriate, discuss the most significant or severe symptoms and how they are affecting the patient’s daily life. Use this opportunity to explore potential treatment strategies or interventions.
Step 5: Securely store completed SSS forms
Once the form is complete, ensure the document is stored securely to maintain confidentiality. For digital records, considering use Carepatron’s secure patient record system, which offers encrypted storage and controlled access. For physical copies, store them in a locked and restricted-access area. Proper storage safeguards patient privacy and ensures compliance with data protection standards.
Benefits of using our Symptom Severity Scale template
The Symptom Severity Scale offers numerous benefits for healthcare professionals and patients, providing a practical and reliable method for assessing and managing symptoms. By incorporating this concise tool into your practice, you can enhance patient care, improve treatment outcomes, and streamline clinical workflows. Key benefits include:
Comprehensive symptom assessment
The SSS allows healthcare professionals to systematically document and evaluate the symptom frequency and severity experienced by patients. With its clear structure and numeric rating scale (NRS), the SSS ensures that a wide range of symptoms—such as pain, fatigue, nausea, and difficulty sleeping—are consistently captured and analyzed.
Improved patient-provider communication
The SSS fosters better communication by enabling patients to rate their symptom severity in a structured and concise format. This reduces miscommunication, enhances collaboration, and ensures that healthcare teams understand the symptoms experienced by patients. This is particularly helpful in primary care settings, where the SSS supports general health assessments and facilitates collaboration with healthcare teams.
Enhanced monitoring and tracking
By tracking symptom intensity over time, the SSS helps healthcare professionals identify trends, detect changes, and evaluate treatment effectiveness. Regular use of the scale allows providers to objectively assess severe symptoms and adjust care plans promptly. The ability to discover the symptom severity ensures that interventions are timely and focused on the most pressing patient concerns, aiding in effective treatment.
Data-driven decision making
The SSS provides objective data through frequency and severity ratings, enabling evidence-based decisions. It aligns with health measurement scales aimed at improving patient care by prioritizing symptoms that significantly impact health-related quality of life. Additionally, the tool’s use of statistical analyses, such as factor analysis and data analysis with statistical significance, ensures that symptom severity scores are interpreted accurately, contributing to improved outcomes.
Tailored and holistic care
The SSS allows patients to document potential causes, triggers, and additional symptoms, adding valuable context to their experiences. For example, the Dutch AIMS2 scales and HFF subscales can be integrated to address specific functional impairments, such as hand and finger function in arthritis patients. This ensures that care plans are tailored to individual needs, promoting better health outcomes and satisfaction.
Commonly asked questions
The Symptom Severity Scale (SSS) is a concise tool for assessing and tracking symptom intensity and severity, commonly used in clinical practice. It provides healthcare professionals with a standardized way to measure symptom and functioning severity across various conditions, including carpal tunnel syndrome and chronic pain.
The SSS is easy to integrate into clinical workflows, offering a concise tool for tracking symptom intensity aiding. It captures the life outcomes and health status of patients by enabling them to rate their symptom severity in a structured format.
Symptom severity can be measured using a visual analog scale (VAS) or numerical rating scale, where patients rate their symptoms on a scale of 0 to 10, with 0 being no symptoms and 10 being the worst imaginable. Patients mark their perceived symptom intensity, which is then recorded and monitored over time to track changes. This simple, subjective method provides valuable data for evaluating treatment effectiveness and guiding clinical decisions.