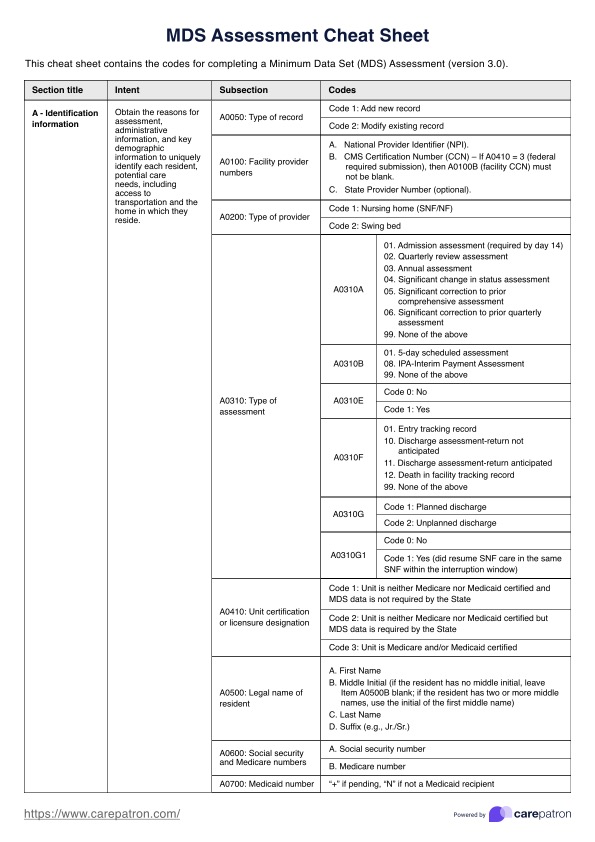
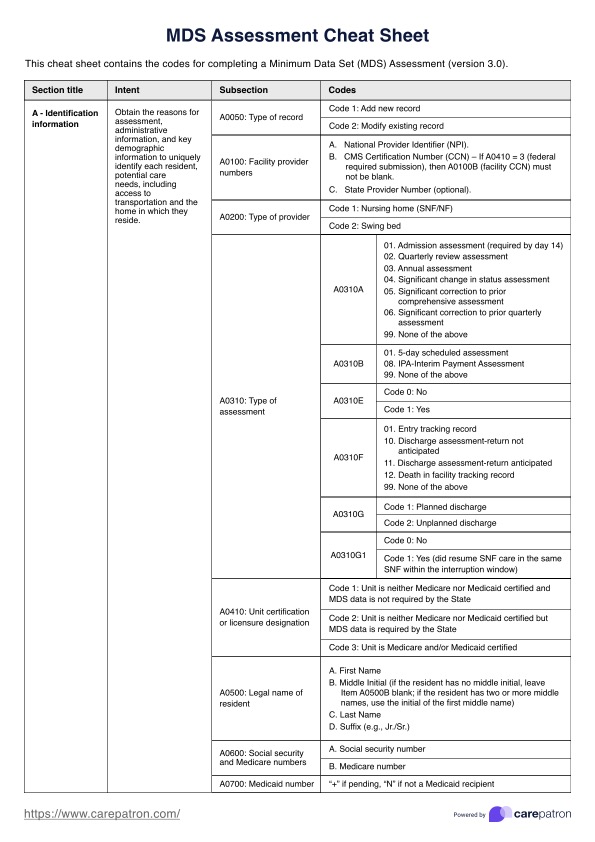
MDS Assessment Cheat Sheet
Access a free MDS Assessment Cheat Sheet, a quick reference guide for healthcare professionals coding mandatory MDS evaluations.


What is an MDS Assessment Cheat Sheet?
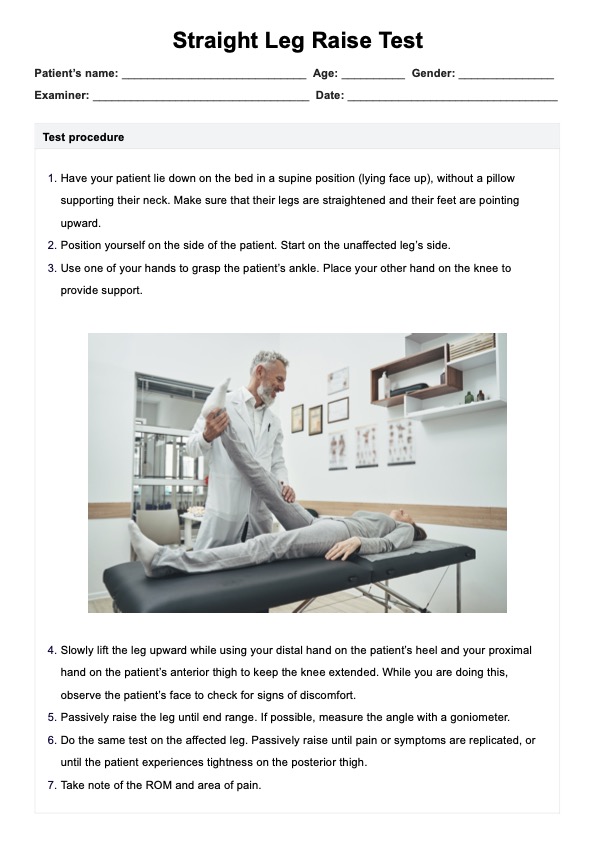
A minimum data set (MDS) assessment is a standardized evaluation used in elderly healthcare to record the functional ability and health of a nursing home resident. It records current health concerns and facilitates appropriate, individualized care. Federal law requires all residents of Medicare and Medicaid-certified facilities to undergo periodic MDS assessments.
An MDS Assessment Cheat Sheet serves as a quick reference tool to aid nursing home staff in accurately completing the assessment. This resource guides staff through the different sections of the evaluation, such as daily living activities, medication usage, oral hygiene, and specific diagnoses, focusing on the resident's condition within the prior seven days.
This comprehensive assessment plays a pivotal role in measuring the health status of residents and initiating comprehensive care plans. Regulatory standards require these assessments to be conducted at specific intervals, including when a resident first arrives, is discharged, or displays a significant change in condition.
A cheat sheet is a simple way to ensure this meticulous process is completed accurately, ensuring a reliable evaluation of the resident's health status. By conducting MDS assessments with precision, nursing home staff contribute to creating a comprehensive and personalized care record, aligning with regulatory standards and fostering optimal resident well-being.
MDS Assessment Cheat Sheet Template
MDS Assessment Cheat Sheet Example
How to use this MDS Assessment Cheat Sheet
Efficiently completing the MDS (Minimum Data Set) Assessment while maintaining accuracy requires a strategic and organized approach. This MDS Assessment Cheat Sheet has been designed as a quick reference tool for healthcare professionals who are coding an MDS assessment form. Here's how it works:
Step 1: Access the cheat sheet
Click the 'download' button on this page to access a printable PDF file of the MDS cheat sheet. Alternatively, click 'use template' to open the cheat sheet in the Carepatron app, where it can be annotated and saved.
Step 2: Review the intent for each section
For each section, read over the intent before beginning the assessment. This is to ensure a comprehensive understanding of what the codes are communicating.
Step 3: Begin completing the form
Systematically work through each section on the MDS assessment form. Some questions require written answers or numbers (e.g. resident's name or Medicaid number), while others will require healthcare providers to check the relevant box(es) or insert the appropriate code. For each subsection requiring a code, refer to the cheat sheet to determine which number to document to ensure accuracy.
Step 4: Seek clarification when needed
Note that this cheat sheet is a quick reference tool, designed to save time by providing a reminder of the code numbers for each section and subsection. Healthcare professionals should refer back to the current RAI manual (Centers for Medicare & Medicaid Services, 2024) for clarification on any sections they are less familiar with, to ensure codes are correct.
Step 5: Double-check responses
Once all sections have been completed, take a moment to review and double-check the responses against the cheat sheet before submitting the assessment. This extra step helps catch potential errors and ensures the accuracy of the information provided.
What are each of the MDS sections?
The documentation requirements for each MDS section must be completed accurately to ensure the assessment is standardized (Centers for Medicare & Medicaid Services, 2024). Here is an overview of some essential documentation requirements for standard MDS sections:
- Section A: Identification information - Resident's name, identification, and demographic details.
- Section B: Hearing, speech, and vision - Documentation related to hearing, speech, and vision impairments.
- Section C: Cognitive patterns - Assessments of cognitive status and abilities, including memory and decision-making.
- Section D: Mood and behavior - Documentation of resident's mood, behaviors, and psychosocial well-being.
- Section E: Preferences for customary routine and activities - Resident's preferences for daily routines and activities.
- Section F: Balance and mobility - Assessment of balance and mobility, including any mobility aids used.
- Section GG: Functional status - Documentation of activities of daily living (ADLs) performance.
- Section H: Bowel and bladder incontinence - Information related to bowel and bladder incontinence.
- Section I: Active diagnoses - Documentation of current active diagnoses and medical conditions.
- Section J: Health conditions - Comprehensive information on various health conditions affecting the resident.
- Section K: Swallowing/nutritional status - Documentation regarding the resident's swallowing and nutritional status.
- Section L: Oral/dental status - Assessment of oral and dental health.
- Section M: Skin conditions - Documentation of skin conditions, wounds, or pressure ulcers.
- Section N: Medications - Comprehensive list of current medications, including dosage and frequency.
- Section O: Special treatments, procedures, and programs - Document any specialized treatments or programs.
- Section P: Restraints - Information on any use of restraints and the associated care plan.
- Section Q: Participation in assessment and goal setting - Resident's involvement and preferences in the assessment and goal-setting process.
Understanding and adhering to specific forms and documentation requirements for each MDS section is crucial for accurate and comprehensive resident assessments in healthcare settings.
What are the consequences of incomplete or inaccurate MDS documentation?
Medicare and Medicaid healthcare facilities are subject to various regulations and standards that mandate accurate and complete MDS documentation. Failure to comply with these regulations can result in penalties, fines, or loss of accreditation.
MDS documentation can also affect Medicare and Medicaid reimbursement rates, meaning facilities may receive lower reimbursement if documentation does not accurately reflect the resident's condition and care needs.
Incomplete or inaccurate MDS (Minimum Data Set) documentation can also significantly affect quality of care. An incorrect reflection of the health status and needs of nursing home residents can result in suboptimal care planning, and hinders effective communication among healthcare professionals. This lack of information may lead to misunderstandings or gaps in the continuity of care, impacting residents' well-being.
Furthermore, inaccurate documentation may lead to legal challenges, especially if there are discrepancies in the provided care and the documented information. Legal actions could result in litigation, fines, or reputational damage to the facility.
References
Centers for Medicare & Medicaid Services. (2024). Long-Term care facility resident assessment instrument 3.0 user’s manual. Version 1.19 .1. https://www.cms.gov/files/document/finalmds-30-rai-manual-v1191october2024.pdf
Commonly asked questions
This MDS Assessment Cheat Sheet is a standardized assessment tool containing the codes for each section of the MDS assessment. It streamlines the data collection process while ensuring accurate completion of each section.
The type of MDS assessment refers to the reason or time at which it was conducted. Common types include admission, quarterly, annual, significant change, and discharge Assessments.
The standard look-back period for the MDS 3.0 is 7 days, unless otherwise stated. Only those occurrences during the look back period will be captured on the MDS.
Nursing staff in Medicare or Medicaid long term care facilities are responsible for completing MDS assessments. Some nursing homes will have an MDS coordinator whose sole responsibility is ensuring MDS assessments are conducted periodically and accurately.