Integrated Treatment Plan
Download Carepatron's free Integrated Treatment Plan PDF template to help you create effective treatment plans for patients.


What is integrated treatment for co-occurring disorders?
Integrated treatment for co-occurring disorders is a comprehensive approach that simultaneously addresses both mental health and substance use disorders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) (2024), this method is critical for effectively managing the complexities associated with dual diagnosis. It integrates services for mental health conditions and chronic pain like generalized anxiety disorder, attention deficit hyperactivity disorder (ADHD), post-traumatic stress disorder (, and panic disorder with treatment for substance abuse, ensuring that both sets of conditions are treated concurrently.
This approach uses a coordinated care model in which the same healthcare providers or teams address both psychiatric symptoms and substance-related issues together. This integrated method improves treatment consistency and enhances recovery outcomes (Kelly & Daley, 2013). A key aspect of this model is the use of evidence-based practices, such as cognitive behavioral therapy, which are customized to meet the specific needs of individuals with co-occurring psychiatric disorders and substance dependency.
Integrated treatment is highly relevant due to its holistic approach, which addresses not only depressive symptoms but also physical health and overall well-being. It follows a "no wrong door" policy, ensuring that anyone seeking help receives comprehensive screening and appropriate care, regardless of their initial concern. By reducing access barriers and prioritizing coordinated, continuous care, this approach aims to lower hospitalization rates, improve quality of life, and promote stable living conditions for individuals facing these complex challenges.
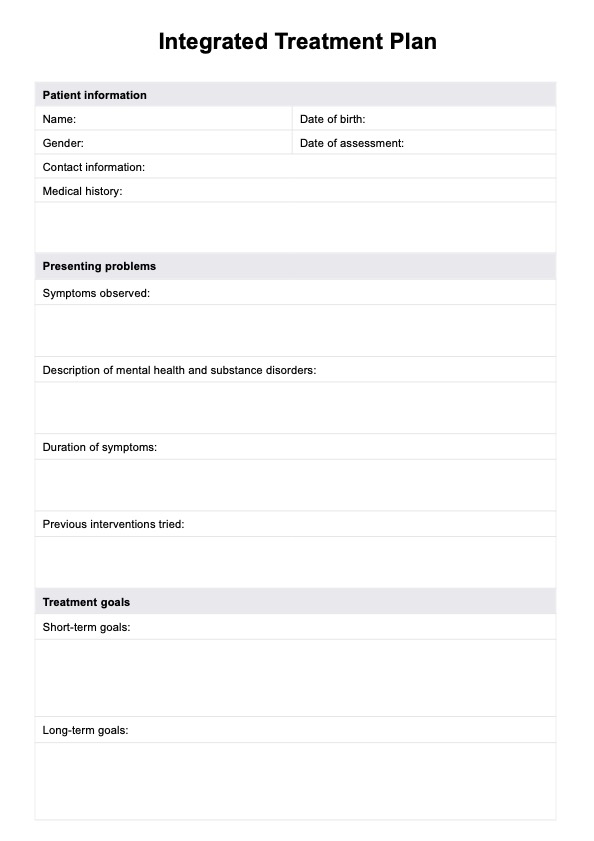
Integrated Treatment Plan Template
Integrated Treatment Plan Example
What is an Integrated Treatment Plan?
An Integrated Treatment Plan is a holistic approach designed to address the complex needs of individuals with co-occurring disorders, such as mental health challenges and substance use disorders. It ensures that physical and mental health concerns are treated simultaneously through a patient-centered and coordinated strategy. This dynamic plan is developed collaboratively with the patient, their family, and a multidisciplinary treatment team to tailor care to their unique circumstances and aspirations.
Integrated Treatment Plans focus on comprehensive care, combining interventions like substance abuse treatment, mental health support, and social assistance. The plan evolves, adapting to the patient’s progress and changing needs. It addresses multiple areas, including physical health, co-occurring mental health issues, social support systems, and relapse prevention strategies.
Carepatron offers a blank Integrated Treatment Plan template to streamline the development of these plans and support effective personalized care.
How to use our free Integrated Treatment Plan template work
Our free blank template simplifies creating effective treatment plans for your patients. Follow these steps to get started:
Step 1: Access the template
Click “Use template” to open and customize the Integrated Treatment Plan in Carepatron's app. The template includes fillable fields and patient-centered features, allowing you to modify it to fit each patient's specific health needs before printing or saving.
Step 2: Introduce the plan to the patient
Present the Integrated Treatment Plan to the patient, explaining its purpose in managing co-occurring disorders. Highlight how the plan coordinates substance abuse treatment, mental health support, and physical care goals, ensuring they understand its role in their long-term recovery.
Step 3: Discuss how the plan goes and goals
Collaborate with the patient to set realistic treatment goals, discussing their specific needs and how the plan addresses them. Ensure they feel involved in developing their care plan, promoting engagement and ownership of their health journey.
Step 4: Provide further patient education and next steps
Offer guidance on available resources, relapse prevention strategies, and lifestyle adjustments. Schedule follow-up sessions to review the patient's progress and adjust the Integrated Treatment Plan as needed to ensure sustained comprehensive care.
Benefits of using this Integrated Treatment Plan template
The Integrated Treatment Plan offers a streamlined and effective approach to managing co-occurring disorders, including mental health disorders like major depressive disorder and borderline personality disorder. By addressing both substance abuse and mental illness simultaneously, this tool ensures that the treatment team addresses all co-occurring disorders effectively, promoting simultaneous treatment outcomes. It supports the implementation of evidence-based practices, such as medication-assisted treatment and mental health treatment, within a cohesive framework.
This plan template also simplifies the treatment process by providing a comprehensive structure that allows you to deliver tailored care to patients with complex conditions. It enhances collaboration among healthcare providers, ensuring that co-occurring disorders are managed effectively and that patient progress is monitored consistently. By facilitating holistic care, the Integrated Treatment Plan helps improve life satisfaction and effective patient treatment while empowering professionals to deliver impactful and sustainable solutions, improving overall treatment efficacy and patient outcomes.
Types of integrated treatment
Integrated treatment programs address the complex needs of individuals with co-occurring disorders by combining approaches that treat both substance abuse disorders and mental disorders simultaneously.
Cognitive behavioral therapy (CBT)
CBT is a cornerstone of integrated treatment (Nakao et al., 2021), helping individuals with co-occurring disorders identify and change harmful thought patterns. It focuses on relapse prevention strategies and equips patients with tools to manage triggers associated with substance abuse disorder and co-occurring mental health conditions.
Medication treatment
Medication can be essential for treating co-occurring disorders, particularly when mental disorders like depression or anxiety require pharmacological support (Iqbal et al., 2019). Combining medication with substance abuse treatment ensures a balanced approach, reducing symptoms and supporting recovery.
Motivational interviewing
Motivational interviewing is a patient-centered method used to encourage individuals with co-occurring disorders to commit to change (Substance Abuse and Mental Health Services Administration, 2019). It fosters collaboration between the patient and the treatment team, building intrinsic motivation to address substance abuse and mental health challenges.
Contingency management
This evidence-based approach reinforces positive behavior by offering rewards for meeting treatment goals. It has proven effective in integrated treatment programs for reducing substance use and promoting adherence to mental health care plans.
Social interventions
Social interventions address the environmental and relational factors affecting individuals with co-occurring disorders. By providing community support, life skills training, and family therapy, these interventions complement substance abuse treatment and foster a supportive network for long-term recovery.
References
Iqbal, M. N., & colleagues. (2019). Treatment for substance use disorder with co-occurring mental illness. FOCUS, 17(2), 88–97. https://doi.org/10.1176/appi.focus.20180042
Kelly, T. M., & Daley, D. C. (2013). Integrated treatment of substance use and psychiatric disorders. Social Work in Public Health, 28(3–4), 388–406. https://doi.org/10.1080/19371918.2013.774673
Nakao, M., & colleagues. (2021). Cognitive–behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. BioPsychoSocial Medicine, 15(1), 1–4. https://doi.org/10.1186/s13030-021-00219-w
Substance Abuse and Mental Health Services Administration (SAMHSA). (2019). Motivational interviewing as a counseling style. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK571068/
Substance Abuse and Mental Health Services Administration. (2024). Managing life with co-occurring disorders. SAMHSA. https://www.samhsa.gov/mental-health/serious-mental-illness/co-occurring-disorders
Commonly asked questions
An Integrated Treatment Plan is a comprehensive, patient-centered approach that addresses both mental health and substance use disorders simultaneously. It ensures coordinated care by involving a multidisciplinary team to tailor interventions to the individual’s specific needs and goals. This dynamic plan evolves to reflect the patient’s progress and changing circumstances.
Effective integrated treatment includes evidence-based practices such as cognitive-behavioral therapy, medication management, and motivational interviewing. It emphasizes a holistic approach, addressing physical health, mental health, and social factors like housing and employment. Key elements also include continuous care, family involvement, and strategies for relapse prevention.
The integrated behavior treatment model is a unified approach designed to address co-occurring disorders by simultaneously treating substance use disorders and mental health symptoms. It integrates interventions to ensure consistency and minimize fragmented care, creating a more effective treatment experience. This model emphasizes patient-centered care, fostering collaboration, adaptability, and long-term recovery for individuals managing complex challenges.