Fasting Insulin Levels
Fasting Insulin Levels Chart - a vital tool for healthcare practitioners. Understand its clinical importance in managing insulin and optimizing patient care.


What is a Fasting Insulin Levels Chart?
Insulin, a hormone secreted by the pancreas's beta cells, helps regulate blood glucose levels. When you consume food, your digestive system breaks down carbohydrates into glucose, which enters your bloodstream. Elevated blood sugar levels trigger insulin release from the pancreas, facilitating the transfer of glucose from the blood into cells, predominantly muscle and fat tissue. It also directs glucose into the liver, storing it as glycogen for future energy needs.
The fasting insulin test assesses your insulin levels following a minimum 8-hour fast. A healthcare practitioner will draw a blood sample from a vein and send it to a lab for analysis. Other tests to evaluate blood sugar and insulin levels include fasting blood glucose, hemoglobin A1C (HbA1c), fructosamine, and c-peptide.
Fasting insulin is a critical yet sometimes underestimated assessment that can help identify insulin resistance. In this regard, the Fasting Insulin Levels Chart is an invaluable resource for monitoring.
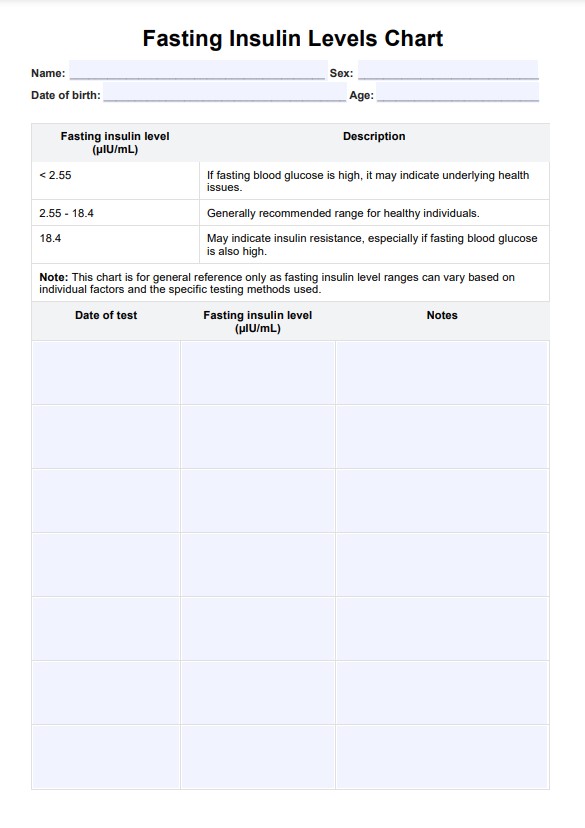
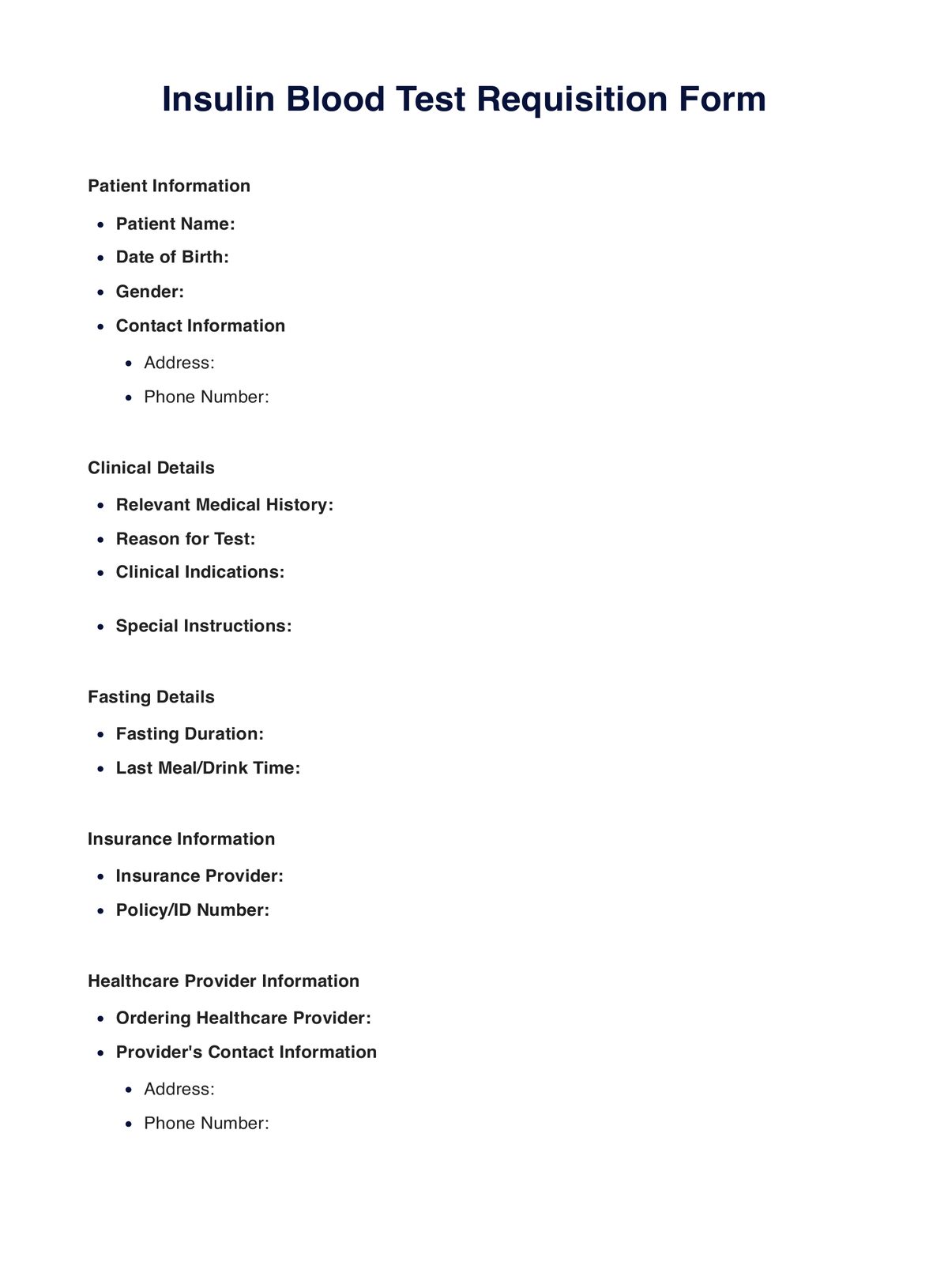
Fasting Insulin Levels Chart Template
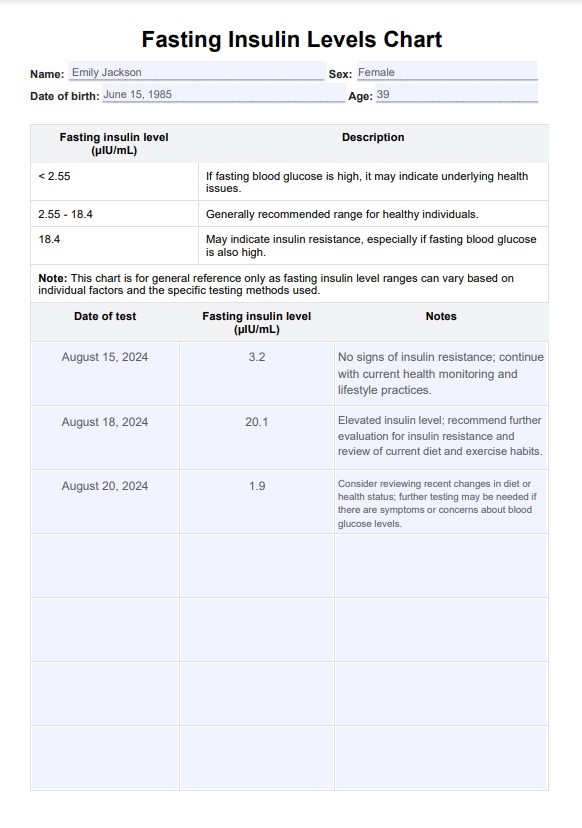
Fasting Insulin Levels Chart Example
Insulin resistance levels and management
Insulin resistance levels are vital to monitor since they indicate how the body's cells respond to low insulin alone, impacting overall metabolic and health conditions. It provides insights into how efficiently the body regulates glucose.
When individuals experience insulin resistance, cells in the body, such as fat tissue and skeletal muscle, do not respond normally to insulin and are less able to manage glucose levels. This results in an increase in blood glucose, which poses increased risk and factors for chronic conditions like high blood pressure, type 2 diabetes mellitus, and heart disease. Measuring serum insulin is also critical, as it relates to conditions such as polycystic ovary syndrome (PCOS) and type 2 diabetes.
Several risk factors exist. There is no single blood test for diagnosing insulin resistance, but various tests can assess insulin and average blood sugar levels and diagnose prediabetes or diabetes. The oral glucose tolerance test is another means of further assessment, showing how the body handles glucose after a meal and checking for conditions like gestational diabetes.
Early detection of insulin resistance allows timely interventions, such as lifestyle changes and medication, to manage and potentially reverse the condition. Proper care can prevent complications, improve overall health, and enhance the quality of life for those affected enough insulin alone. Lifestyle modifications such as regulating body weight, proper nutrition, and exercise can reverse insulin resistance.
Nutritional strategies for optimizing insulin sensitivity
This section could offer detailed advice on dietary approaches to improve insulin sensitivity, including:
- Low-glycemic index diets: Learn how consuming foods with a low glycemic index can help stabilize blood sugar and insulin levels.
- Role of macronutrients: Discussion on balancing carbohydrates, proteins, and fats in managing insulin levels.
- Specific foods and supplements: Recommendations for foods and supplements that have been shown to enhance insulin sensitivity, such as omega-3 fatty acids, soluble fiber, and certain vitamins and minerals.
How does the Fasting Insulin Levels Chart work?
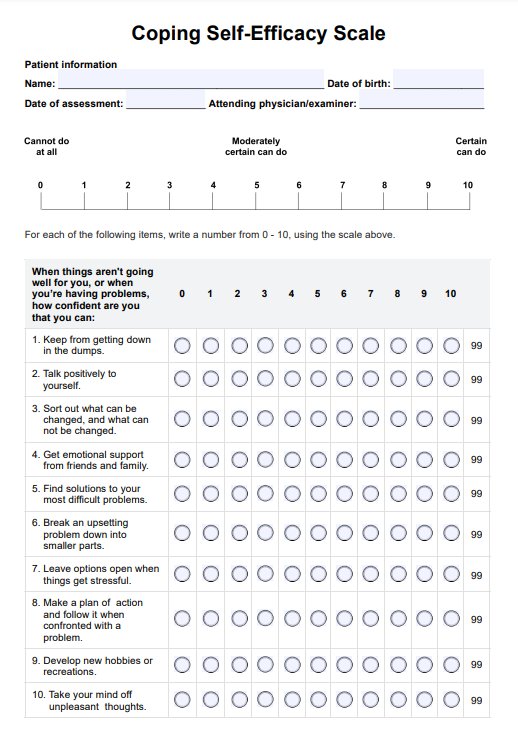
For healthcare practitioners, having access to a well-structured and comprehensive printable Fasting Insulin Levels Chart is essential. Here's how to use this fasting insulin test chart:
Obtain a template
Start by downloading this Fasting Insulin Levels Chart template for healthcare professionals from this page.
Use the provided interpretation table
The chart includes an interpretation table to help assess fasting insulin levels. Levels below 2.55 µIU/mL, especially with elevated fasting blood glucose, may indicate underlying health issues. A range of 2.55 to 18.4 µIU/mL is generally recommended for healthy individuals. Levels above 18.4 µIU/mL may suggest insulin resistance, particularly if fasting blood glucose is also high.
Have the patient log results
After the patient has fasted, conduct the insulin level test. Record the test date and the fasting insulin level (in µIU/mL). This data is vital for tracking insulin trends over multiple tests.
Make notes on lifestyle changes
After interpreting the results, document any recommended lifestyle changes or follow-up actions, such as dietary adjustments, increased physical activity, or further medical consultations. Tracking these recommendations over time helps monitor the impact of interventions and guide future patient care.
When should you use the Fasting Insulin Levels Chart?
The Fasting Insulin Levels Chart is necessary for various healthcare scenarios where precise monitoring of insulin levels and normal blood sugar levels is of utmost importance. Regular blood tests are crucial to monitor glucose levels and guide interventions for managing insulin resistance. It plays a pivotal role in diabetes management, facilitating the regular tracking of fasting insulin levels and blood sugar tests and enabling healthcare practitioners to make more effective adjustments to a patient's diabetes treatment plan.
This chart extends its value to individuals with metabolic disorders such as metabolic syndrome. It provides a structured approach to assessing insulin sensitivity and dynamics to optimize treatment strategies for cardiovascular disease.
For patients taking on weight management journeys and those seeking to improve their metabolic health and overcome insulin resistance, the Fasting Insulin Levels Chart is a valuable ally. It aids in evaluating insulin sensitivity and guiding the formulation of tailored lifestyle changes, like implementing a healthy diet. It also serves as an invaluable resource in routine health check-ups, enhancing the comprehensiveness of patient assessments.
Commonly asked questions
Insulin levels can fluctuate throughout the day based on food intake, physical activity, stress, and other factors. This is why fasting insulin levels are measured after an 8-12 hour fast to provide a consistent baseline for assessing normal blood sugar levels.
In addition to fasting insulin, tests for high blood sugar, such as fasting blood glucose, hemoglobin A1C (HbA1c), fructosamine, and c-peptide, are commonly used to evaluate both high blood glucose, sugar control, and insulin function.
Lifestyle factors such as diet, physical activity, stress management, and sleep quality significantly influence fasting insulin levels. A diet high in refined sugars and carbohydrates can increase insulin levels, while regular exercise and a balanced diet help maintain healthy plasma glucose levels and normal blood sugar level.












-template.jpg)