Gillet Test
Learn about the Gillet Test for assessing sacroiliac joint dysfunction, including step-by-step procedures, interpretation, and more. Free PDF download.


What is sacroiliac joint dysfunction?
Sacroiliac joint dysfunction refers to improper movement of the joints at the bottom of the spine that connect the sacrum to the pelvis. This condition can cause significant lower back and leg pain, often mimicking other conditions such as herniated discs or hip problems. Accurate diagnosis is essential, as the sacroiliac joint is responsible for transmitting the weight and forces of the upper body to the lower limbs.
Sacroiliac joint dysfunction can arise from various causes, including trauma, arthritis, pregnancy, and biomechanical issues such as leg length discrepancy or scoliosis. Common symptoms include localized pain in the lower back, buttocks, and thighs, sometimes extending down to the legs. The pain is often exacerbated by activities that stress the sacroiliac joint, such as standing up from a seated position, climbing stairs, or running.
Healthcare professionals use a combination of clinical tests to diagnose sacroiliac joint dysfunction. Pain provocation tests, such as the thigh thrust and palpation tests, are commonly used to assess the presence and severity of sacroiliac joint pain. A positive test result in these assessments can help confirm the diagnosis. Other tests of the sacroiliac joint include the Gillet Test, which evaluates the mobility and function of the joint, and various imaging studies that can further aid in identifying the underlying cause of the dysfunction.
How to diagnose sacroiliac joint dysfunction
Diagnosing sacroiliac joint dysfunction requires a comprehensive approach, incorporating various clinical tests to identify the source of buttock and lower back pain accurately. Among the most commonly used tests of the sacroiliac joint are pain provocation tests, such as the thigh thrust test, which involve applying controlled pressure to specific areas to elicit pain responses.
Palpation and palpatory clinical tests are also essential, as they help assess tenderness and pain in the sacroiliac region. One widely used palpation test is the Stork Test, also known as the Gillet Test, which evaluates sacroiliac joint mobility by observing the movement of the posterior superior iliac spines during single-leg stance.
However, note that no single test can definitively diagnose sacroiliac joint dysfunction; therefore, a combination of tests is often used. Typically, a diagnosis is considered more reliable if at least three out of four tests of sacroiliac joint yield positive results. These tests include pain provocation tests, palpatory clinical tests, and functional assessments like the Gillet Test. In cases with inconclusive test results, imaging studies may rule out other conditions.
Physical therapy plays a crucial role in diagnosing and treating sacroiliac joint dysfunction, helping improve joint mobility and alleviate pain. However, it is essential to distinguish between symptomatic and asymptomatic patients, as some individuals may exhibit positive test results without experiencing any pain or dysfunction.
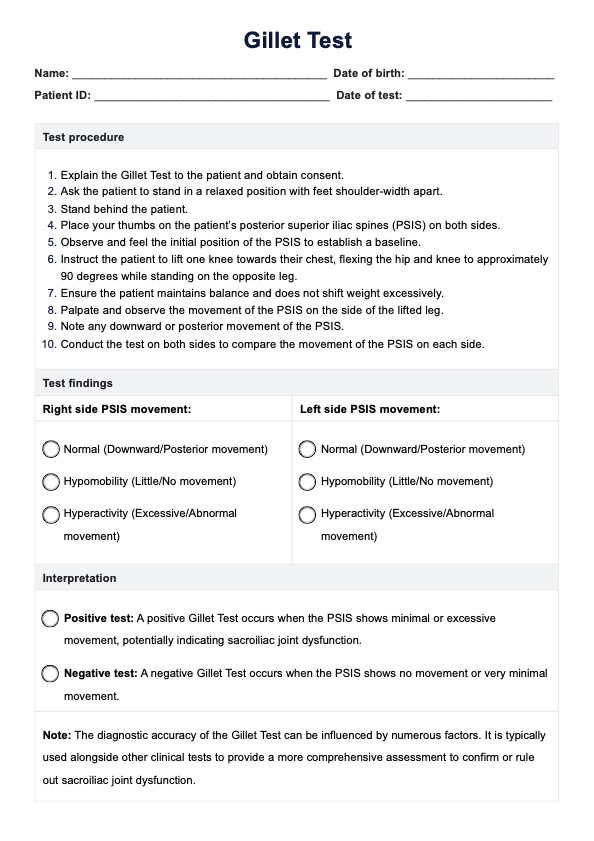
Gillet Test Template
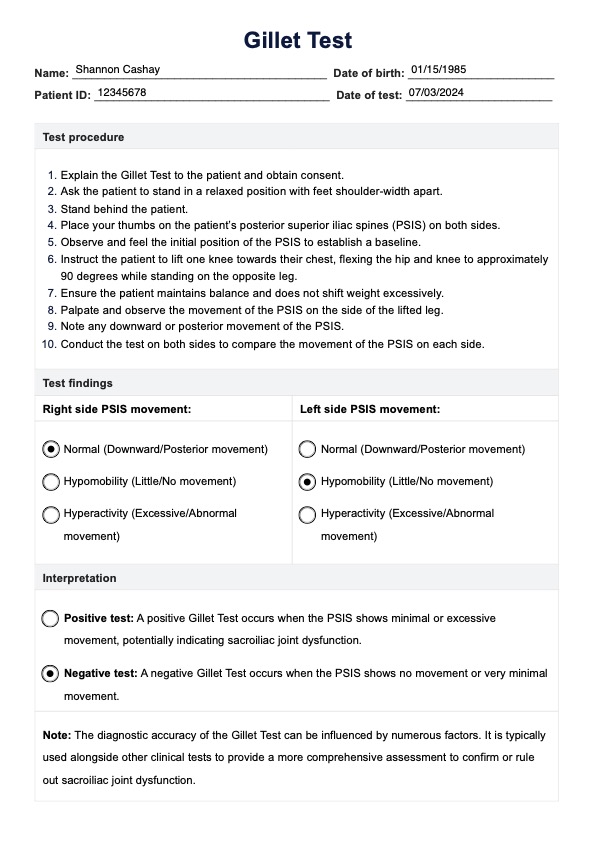
Gillet Test Example
What is the Gillet Test?
The Gillet Test, also known as the Stork Test, is a clinical assessment used by physical therapists and pain physicians to evaluate the mobility and function of the sacroiliac joint. During the test, the examiner palpates the posterior superior iliac spines (PSIS) while the patient lifts one knee towards their chest, simulating a stork-like stance. This motion palpation helps the examiner observe the movement of the PSIS and assess sacroiliac motion.
A positive Gillet or Stork Test is where the PSIS moves little to no or excessively, which may indicate sacroiliac joint dysfunction. However, the diagnostic validity of the Gillet Test can be influenced by various factors, and it is often used in conjunction with other clinical tests for a more comprehensive assessment.
Despite its utility, the Gillet Test is not without limitations. For instance, asymptomatic patients may sometimes exhibit positive test results, highlighting the need to interpret findings carefully. Additionally, while the test can provide valuable insights into sacroiliac motion, it does not offer conclusive predictive values. Therefore, combining the Gillet Test with other assessments, such as the compression test and other palpatory tests, enhances its diagnostic accuracy.
Exercise therapy may be recommended based on the test outcomes to improve sacroiliac joint function and alleviate pain, making the Gillet Test an integral part of the diagnostic and therapeutic process for sacroiliac joint dysfunction.
How to perform the Gillet Test
The Gillet Test is a simple yet effective way to assess sacroiliac joint mobility and function. It involves observing the motion of the posterior superior iliac spines (PSIS) while the patient performs a specific leg movement.
Step 1: Preparation
Begin by explaining the procedure to the patient and obtaining their consent. Ask the patient to stand in a relaxed position with their feet shoulder-width apart.
Step 2: Positioning the examiner
Stand directly behind the patient and place your thumbs on the patient’s PSIS on both sides. This positioning allows you to palpate intrapelvic motion effectively.
Step 3: Baseline observation
Observe and feel the initial position of the PSIS to establish a baseline. This step is crucial for identifying any changes in the position during the test.
Step 4: Patient movement
Instruct the patient to lift one knee towards their chest, flexing the hip and knee to approximately 90 degrees, while standing on the opposite leg. Ensure the movement is slow and controlled.
Step 5: Palpation and observation
Palpate the PSIS on the tested side as the patient lifts their knee. Observe the movement of the PSIS, noting any downward or posterior motion, or lack thereof.
Step 6: Repeat for both sides
Repeat the test on the opposite side to compare the PSIS movement bilaterally. Abnormal movement on one side compared to the other may indicate sacroiliac joint dysfunction.
Step 7: Interpretation
Analyze the findings from both sides. Normal movement is characterized by the PSIS moving downward or posteriorly on the tested side. Lack of movement or abnormal movement suggests potential dysfunction in the sacroiliac joint.
By following these steps, healthcare professionals can effectively use the Gillet Test as part of their broader assessment of sacroiliac joint function, comparing results bilaterally to identify any discrepancies.
Commonly asked questions
The Gillet Test, also known as the Stork Test, is used to assess the mobility and function of the sacroiliac (SI) joint. It helps identify potential dysfunctions by observing the movement of the posterior superior iliac spines (PSIS) during specific leg movements.
The Gillet Test involves the patient standing while the examiner palpates the PSIS. The patient lifts one knee towards the chest, and the examiner observes the movement of the PSIS on the tested side. Normal movement indicates a functioning SI joint, while abnormal movement suggests dysfunction.
If the PSIS on the tested side moves downward or posteriorly, it indicates normal SI joint function. Little to no movement or excessive motion suggests sacroiliac joint dysfunction, which can contribute to lower back and buttock pain. The test results should be considered alongside other clinical assessments for an accurate diagnosis.