Fall Risk Assessment
Identify patients who may be at risk of a fall and implement interventions to prevent falls before they happen, with our simple Fall Risk Assessment, based on the Peninsula Health FRAT.


What is a Fall Risk Assessment?
Fall risk assessment is a crucial process to evaluate an individual's susceptibility to falling, particularly prevalent among the elderly population. It systematically examines various factors contributing to the likelihood of a person experiencing a fall, with the ultimate goal of implementing preventive measures to mitigate this risk.
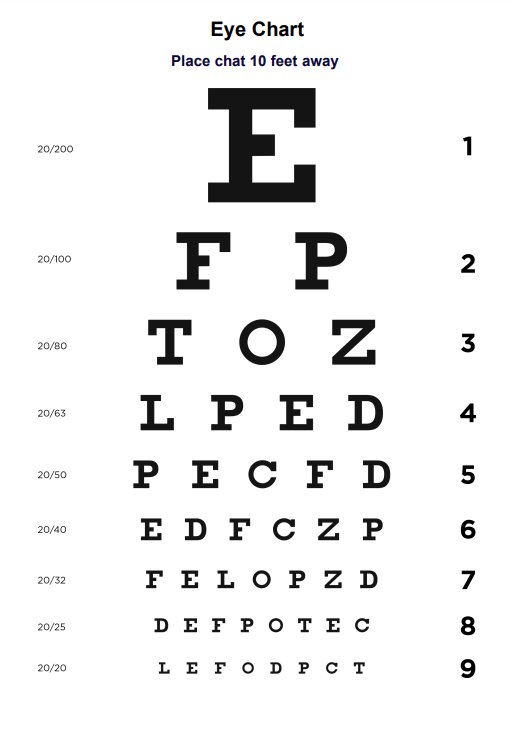
The assessment typically utilizes a combination of fall risk evaluation tools and checks to identify potential risk factors. These may include previous falls, balance impairment, mobility limitations, medication usage, visual impairment, cognitive decline, and environmental hazards. By comprehensively evaluating these factors, healthcare professionals can stratify individuals into different risk categories ranging from low to high risk.
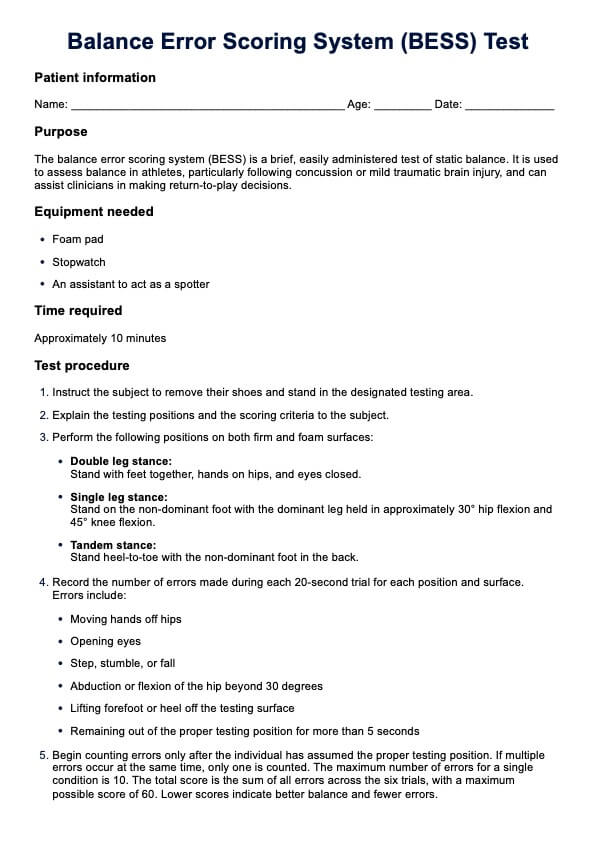
For community-dwelling older adults, fall risk screening often begins with simple questions about any history of falls or near falls. Further assessment may involve a physical examination, including balance assessment, gait analysis, muscle strength evaluation, and assessment of sensory function. Additionally, using standardized risk assessment tools, such as the Timed Up and Go test or the Berg Balance Scale, aids in objectively quantifying an individual's fall risk.
Identifying those at high risk of falls is crucial as they are more susceptible to serious injury, which can significantly impact their quality of life. Therefore, interventions to prevent falls must be tailored to address the specific needs of each individual. These may include exercise programs to improve strength and balance, home modifications to reduce environmental hazards, medication management to minimize side effects that affect balance, and education on fall prevention strategies.
Physical therapists play a pivotal role in evaluating patients' risk for falls and implementing appropriate interventions. Through comprehensive assessments and personalized interventions, they aim to reduce the incidence of falls and promote safety and independence in daily activities. By stopping elderly accidents before they happen, fall risk assessment and prevention contribute significantly to improving the overall well-being of older adults and reducing healthcare costs associated with fall-related injuries.
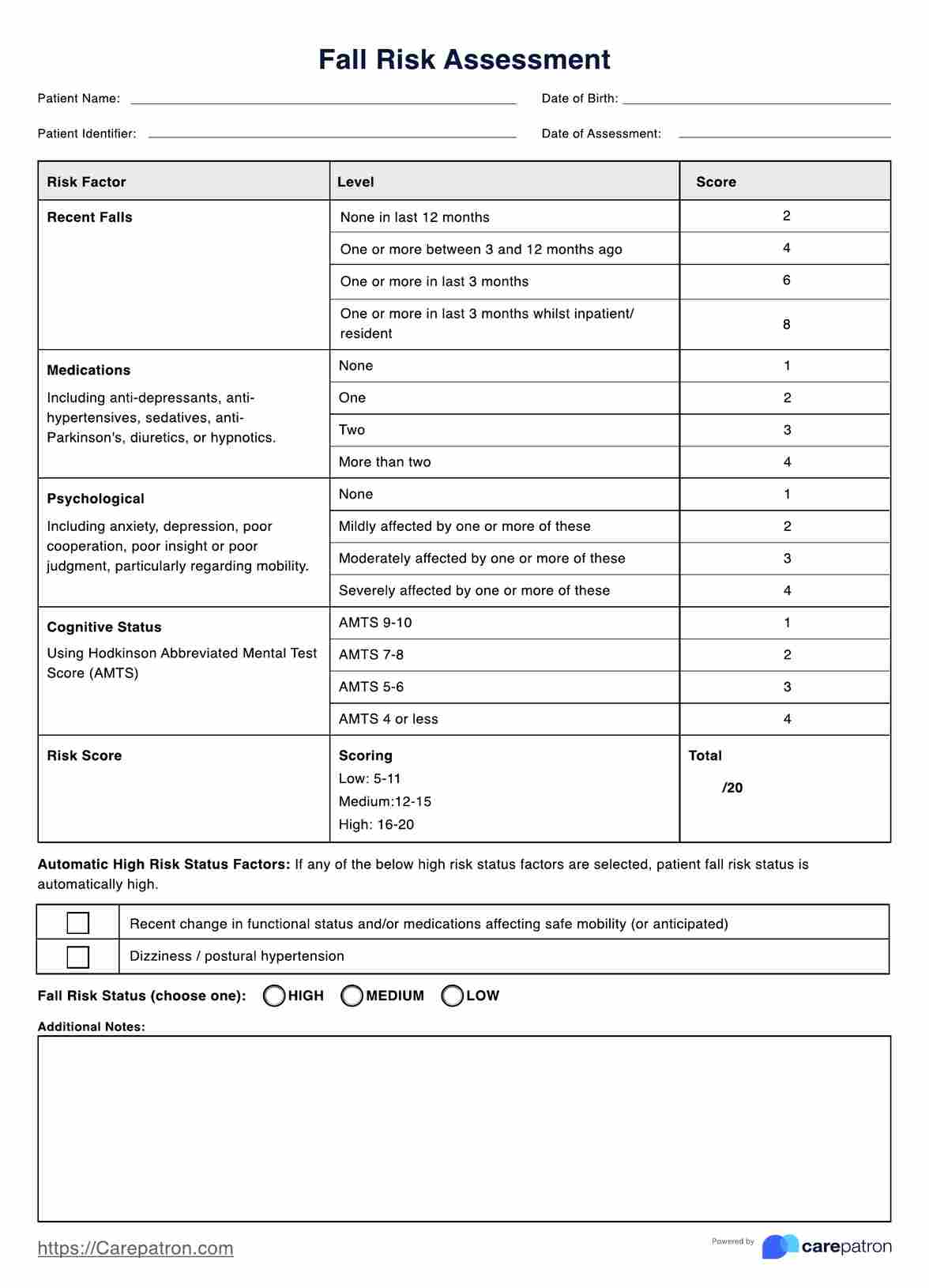
Fall Risk Assessment Template
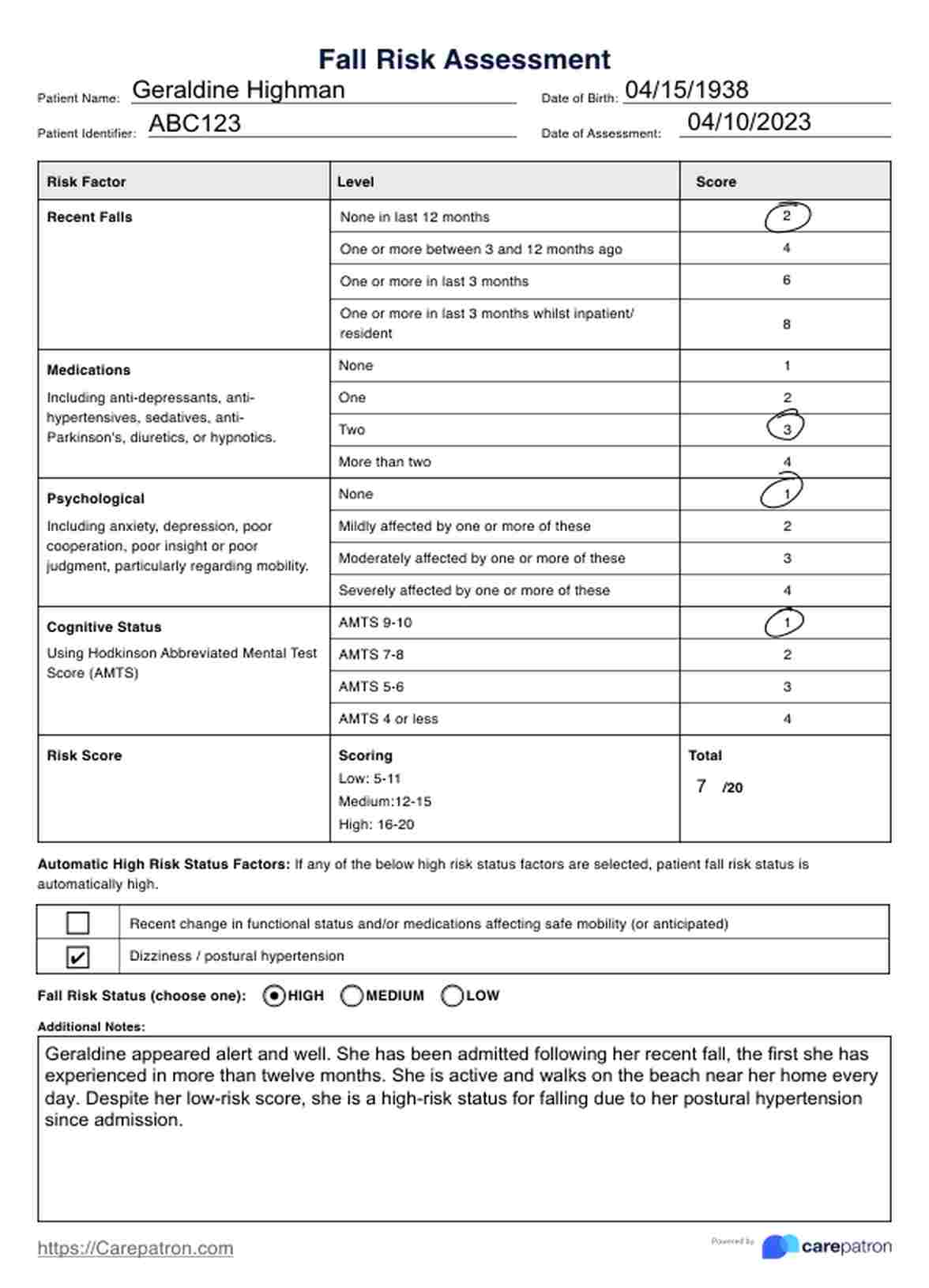
Fall Risk Assessment Example
How to use this Fall Risk Assessment
This simple Fall Risk Assessment is based on the first part of the full Fall Risk Assessment Tool (FRAT) developed by Peninsula Health in 1999. This assessment is split into different risk factors that can contribute to an increased likelihood of falling. Follow the step-by-step guide below to gain confidence in administering this invaluable assessment.
Step 1: Gather information
Before administering the fall risk assessment form, gather relevant information about the individual's medical history, current medications, recent falls, mobility status, cognitive function, and psychological well-being. This information can be obtained through interviews with the individual, their caregivers, and a review of their medical records.
Step 2: Conduct a quick assessment
Begin by asking the individual about their history of falls, including the frequency and circumstances of any recent falls. Inquire about any mobility problems they may experience, such as unsteady or difficulty walking. Assess their visual function by asking if they have had an eye exam recently.
Step 3: Review medications
Conduct a thorough review of the individual's medications, paying particular attention to those known to increase the risk of falls, such as sedatives or medications that lower blood pressure. Determine if they are taking multiple medications or if there have been recent changes in their medication regimen.
Step 4: Assess home environment
Evaluate the individual's home environment for potential hazards that could increase the risk of falls, such as poor lighting, loose rugs, or lack of grab bars in the bathroom. Discuss any modifications or adaptations that may be needed to improve home safety.
Step 5: Administer the Fall Risk Assessment form
Guide the individual through the fall risk assessment form, explaining each question and recording their responses accurately. Ensure that the individual understands the purpose of the assessment and feels comfortable providing honest answers.
Step 6: Analyze the results
Calculate the total risk score based on the responses provided in the assessment form. Determine the individual's risk category (low, medium, or high) based on the total score and the presence of automatic high-risk status factors.
Step 7: Develop a personalized care plan
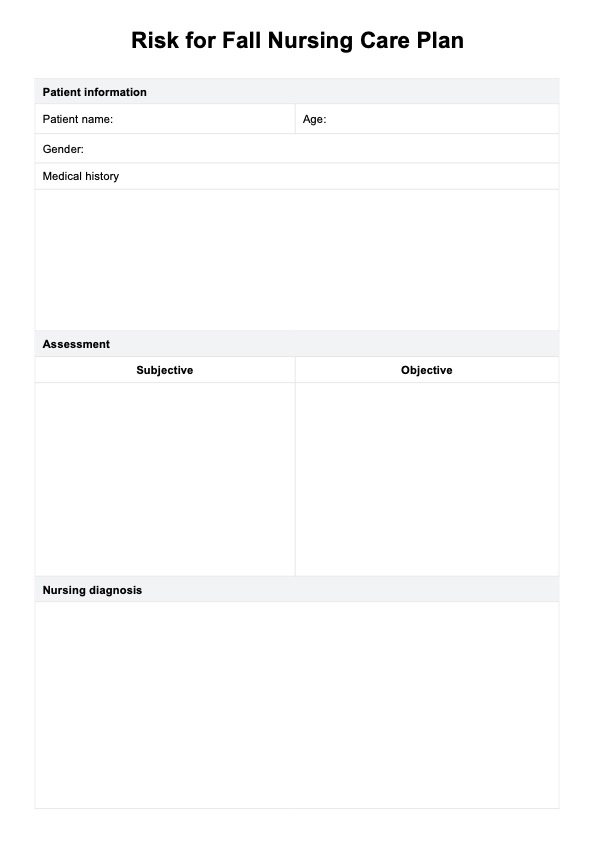
Based on the individual's risk level and identified risk factors for falls, collaborate with a multidisciplinary team, including physicians, occupational therapists, and other healthcare professionals, to develop a personalized care plan. This plan may include exercise programs to improve strength and balance, medication adjustments, home modifications, and referrals to other specialists as needed.
Step 8: Follow-up and reassessment
Regularly monitor the individual's progress and reassess their risk of falls as needed. Modify the care plan based on changes in their health status or home environment. Provide ongoing education and support to promote safety and reduce the risk of falls in their daily living activities.
To further enhance your practice, check out our risk assessment form and care plan templates.
When would you typically use this Fall Risk Assessment?
The Fall Risk Assessment Assessment is a valuable resource that healthcare providers utilize in various settings to evaluate an individual's risk of falls and implement preventive measures accordingly. It is particularly appropriate in the following scenarios:
- Primary Care Settings
- During routine medical appointments, healthcare providers can administer the fall risk assessment to elderly patients or those with a history of falls. This helps in the early identification of risk factors and the implementation of preventive strategies.
- After a Head Injury
- Following a head injury or concussion, assessing the patient's risk of falls becomes crucial. The fall risk assessment aids in identifying factors such as balance impairments or cognitive deficits that may increase the risk of further injury.
- Occupational Therapy Sessions
- Occupational therapists often use the fall risk assessment to evaluate older adults or individuals with mobility limitations comprehensively. This guides the development of tailored interventions to improve balance and prevent falls.
- Physical Therapy Sessions
- Physical therapists incorporate the fall risk assessment into their assessments of rehabilitation patients, especially those recovering from injuries or surgeries that affect mobility. It informs the design of balance training programs and home exercise plans.
- Halfway Through Treatment
- In long-term medical treatment or rehabilitation, conducting periodic fall risk assessments approximately halfway through the treatment course allows healthcare providers to monitor patient risk factors and adjust interventions accordingly.
- Before Discharge from Care
- Before discharging patients from medical care or rehabilitation, healthcare providers can conduct a final fall risk assessment to ensure that appropriate measures have been taken to prevent falls and reduce the risk of serious injury.
By integrating the fall risk assessment into various healthcare settings and patient care pathways, healthcare providers can effectively identify intrinsic and extrinsic factors contributing to the risk of falls. This proactive approach facilitates early intervention, tailored balance training, and implementation of safety measures to prevent falls and promote the well-being of older adults and individuals with mobility limitations.
.png)
Who can use this printable Fall Risk Assessment?
The printable Fall Risk Assessment is a versatile tool that can be utilized by a wide range of healthcare practitioners caring for individuals at risk of falls. Some relevant practitioners who can effectively use this form include:
- Primary Care Physicians
- Primary care physicians play a pivotal role in assessing and managing the health of older adults. They can use the Fall Risk Assessment to systematically evaluate their patients' risk factors for falls during routine medical visits and initiate appropriate interventions to prevent falls.
- Physical Therapists
- Physical therapists specialize in restoring mobility and function in individuals with physical impairments. They can use the Fall Risk Assessment as part of their initial evaluation to identify balance deficits and other factors contributing to the risk of falls. This guides the development of personalized exercise programs to improve strength, balance, and gait.
- Occupational Therapists
- Occupational therapists focus on promoting independence in daily activities for individuals with physical or cognitive limitations. They can incorporate the Fall Risk Assessment into their assessments to identify environmental hazards and recommend home modifications or assistive devices to enhance safety and prevent falls.
- Geriatricians
- Geriatricians specialize in the care of older adults and are well-positioned to assess and manage the complex health needs of this population. They can use the Fall Risk Assessment as part of comprehensive geriatric assessments to identify modifiable fall risk factors and develop multidisciplinary care plans to address them.
- Nurse Practitioners
- Nurse practitioners often provide primary care services and are skilled in conducting health assessments and implementing preventive measures. They can use the Fall Risk Assessment during patient visits to identify individuals at increased risk of falls and coordinate referrals to other healthcare professionals for further evaluation and management.
- Home Health Nurses
- Home health nurses care for individuals in their homes, where fall risks may be more prevalent. They can use the Fall Risk Assessment to conduct home safety evaluations and educate patients and their caregivers about strategies to prevent falls and promote safety in the home environment.
Benefits of free Fall Risk Assessment
1. Early identification of risk factors
Conducting a free fall risk assessment allows for the early identification of risk factors contributing to falls, enabling healthcare providers to intervene proactively.
2. Tailored interventions
By identifying specific risk factors through the assessment, healthcare professionals can develop personalized interventions targeted at addressing patients' individual needs, thereby reducing the risk of falls.
3. Prevention of fall-related injuries
Implementing preventive measures based on the assessment results can significantly reduce fall-related injuries, promoting patient safety and well-being.
4. Cost savings
Free fall risk assessments facilitate early intervention and prevention strategies, ultimately leading to cost savings by reducing hospital admissions, emergency department visits, and healthcare expenditures associated with fall-related injuries.
5. Improved quality of life
Individuals can maintain their independence, mobility, and quality of life by reducing the risk of falls and fall-related injuries, enhancing their overall well-being and functional status.
6. Enhanced patient-centered care
Utilizing free fall risk assessments promotes patient-centered care by involving patients in the assessment process, addressing their individual concerns, and empowering them to participate in fall prevention strategies tailored to their actively.
Commonly asked questions
Fall Risk Assessment is particularly important for older adults, individuals with mobility impairments, those with a history of falls, and patients recovering from injuries or surgeries that affect mobility.
Common risk factors assessed in the Fall Risk Assessment include previous falls, balance impairment, medication usage (sedatives or antihypertensives), cognitive impairment, visual deficits, and environmental hazards.
Fall Risk Assessment is typically conducted using standardized assessment tools, questionnaires, and physical examinations. Healthcare professionals may also review medical records, conduct medication reviews, and assess the individual's home environment for potential fall hazards.