Ear Infection Test
Explore our comprehensive guide on Ear Infection Tests designed for healthcare professionals to effectively diagnose and manage ear infections.


What is an ear infection?
An ear infection, medically known as otitis media, is an inflammation of the middle ear, typically caused by bacteria or viruses. This condition is most common in children but can occur at any age. Ear infections can be classified into various types, including acute otitis media (AOM), which presents with rapid symptoms and middle ear inflammation, and otitis media with effusion (OME), where fluid remains in the middle ear without bacterial or viral infection symptoms. Another type is external otitis, or swimmer's ear, affecting the outer ear canal. Ear infections can be particularly concerning because they may lead to temporary hearing loss, impacting speech and language development in children.
These infections often result from another illness like a cold, flu, or allergy that causes congestion and swelling of the nasal passages, throat, and eustachian tubes. The eustachian tubes, small passages that connect the middle ear to the back of the throat, help equalize ear pressure and drain normal ear secretions. When these tubes become swollen or blocked, fluid can build up in the middle ear, creating a breeding ground for bacteria or viruses, leading to infection.
In some cases, especially in children who experience frequent ear infections or fluid build-up, ear tubes may be recommended. These tiny tubes are surgically inserted into the eardrum to allow air to enter the middle ear and prevent fluid accumulation, thereby reducing the risk of further infections and aiding in treating hearing loss associated with otitis media.
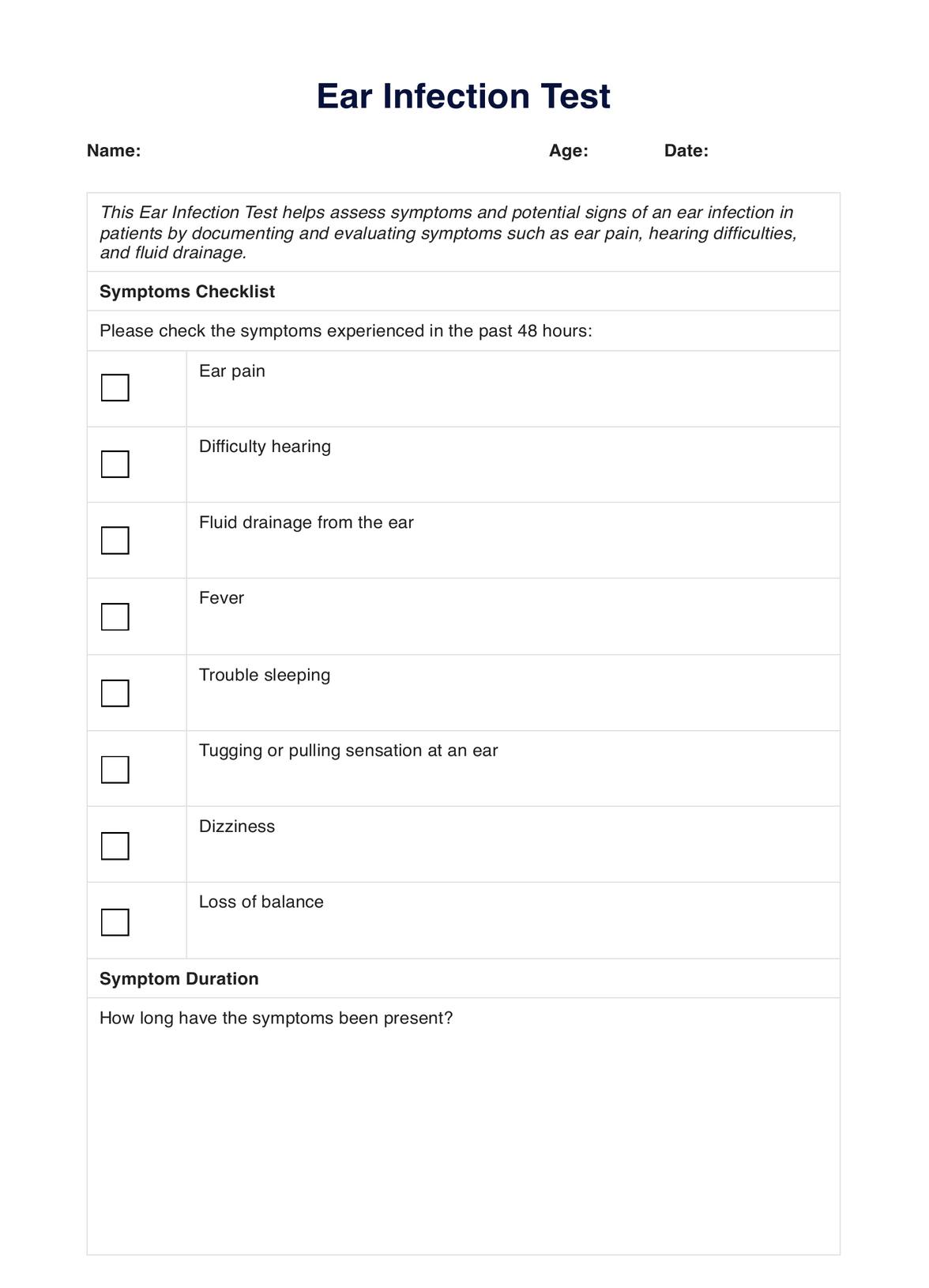
Ear Infection Test Template
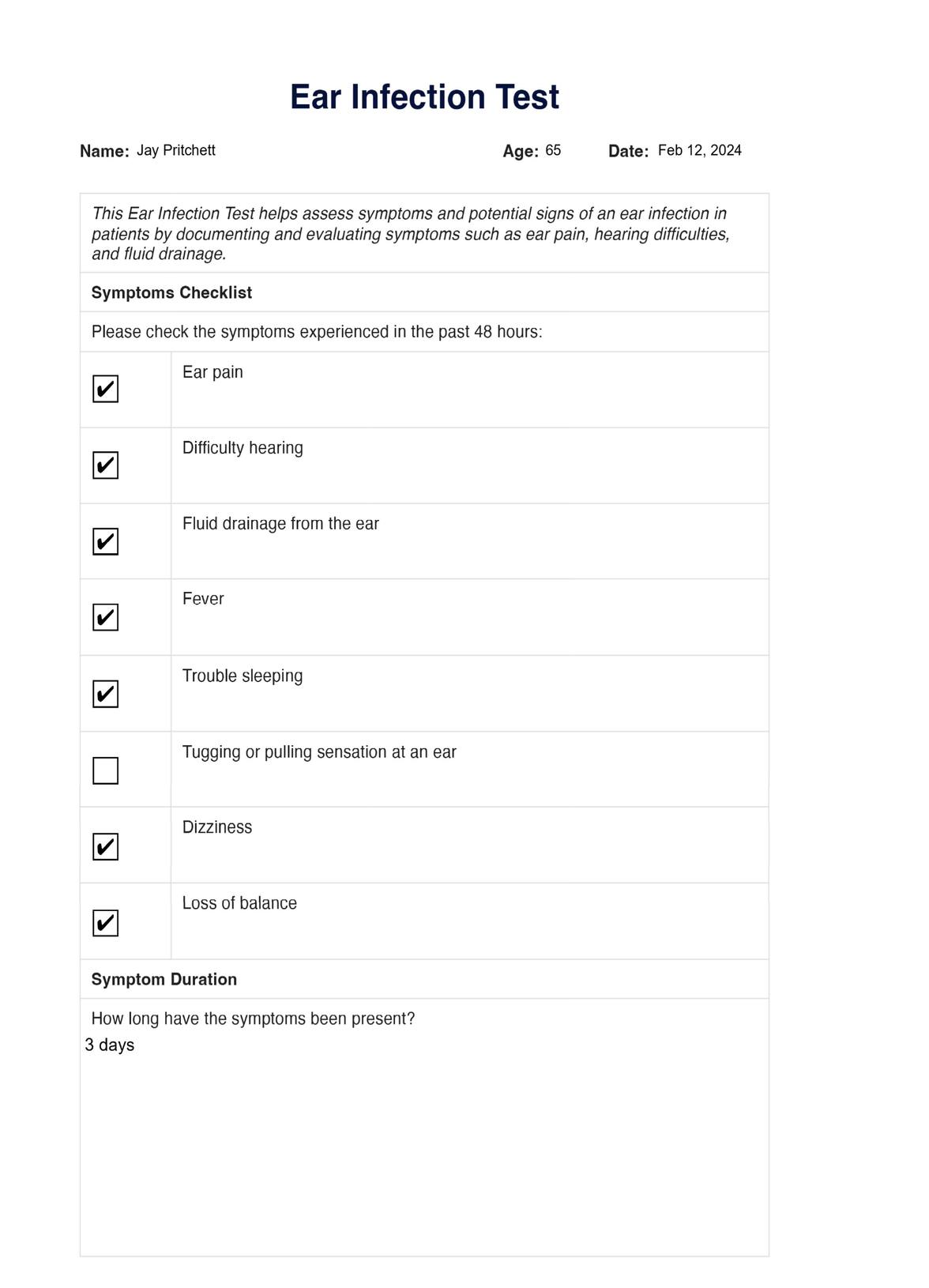
Ear Infection Test Example
What are the signs and symptoms of an ear infection?
Ear infections can manifest through various signs and symptoms, which can differ in intensity from one individual to another. Recognizing these symptoms is crucial for timely diagnosis and treatment. Here are some common signs and symptoms associated with ear infections:
- Ear pain: Ear pain, or otalgia, affecting one or both ears, is the most common symptom of an ear infection. It can range from mild discomfort to severe pain and may worsen when lying down due to pressure changes in the middle ear.
- Difficulty hearing: Fluid build-up in the middle ear can cause temporary hearing loss or muffled hearing, making it challenging to understand spoken words, especially in noisy environments.
- Fluid drainage from the ear: Sometimes, an ear infection can lead to the drainage of fluid from the ear canal, which might be clear, yellow, or bloody. This symptom often indicates a ruptured eardrum.
- Fever: Especially in children, an ear infection might be accompanied by a fever, reflecting the body's response to the infection.
- Trouble sleeping: The discomfort and pain caused by an ear infection can make it difficult for individuals, particularly children, to sleep through the night. This may also result in irritability.
- Tugging or pulling sensation at a child's ear: Young children, who may not be able to verbalize their discomfort, might tug or pull at their ears in response to the pain.
- Dizziness: If the infection affects the inner ear, it can lead to dizziness or problems with balance, as the inner ear is responsible for equilibrium.
- Loss of balance: Similar to dizziness, a loss of balance can occur if the infection extends to the inner ear structures that regulate balance.
These symptoms can indicate the presence and severity of an ear infection. Healthcare professionals and caregivers must be vigilant for these signs, especially in children who cannot communicate their discomfort effectively. Early recognition and treatment can prevent the progression of the infection and reduce the risk of complications.
What are the causes of ear infections?
Understanding the causes of ear infections is crucial for their prevention and treatment. Here are the primary factors that can lead to the development of an ear infection:
- Bacterial or Viral Infections: The most common cause of ear infections, especially middle ear infections (acute otitis media), results from bacterial or viral infections. These can follow other illnesses like colds, the flu, or upper respiratory infection, as pathogens travel from the nose and throat to the middle ear.
- Eustachian Tube Dysfunction: The Eustachian tubes connect the middle ear to the back of the throat and can become blocked or swollen. This can lead to fluid accumulation in the middle ear, creating an environment conducive to infection.
- Enlarged Adenoids: Particularly in children, enlarged adenoids near the openings of Eustachian tubes can block these tubes, leading to repeated ear infection episodes.
- Allergies: Allergic reactions that cause inflammation and swelling in the Eustachian tubes can lead to fluid buildup in the middle ear, increasing the risk of infection.
- Environmental Factors: Exposure to tobacco smoke, air pollution, and frequent colds can heighten the risk of developing ear infections by impacting the upper respiratory system and Eustachian tube functionality.
- Poor Immune Function: Those with weakened immune systems due to illness, age, or medical treatments, are more susceptible to infections, including ear infections.
Addressing these causes can help healthcare professionals guide their patients in reducing the risk of ear infections or managing existing conditions more effectively. Implementing preventive measures, such as avoiding exposure to smoke, controlling allergies, and practicing good hygiene, is also vital in minimizing the incidence of ear infections.
How are ear infections diagnosed?
Diagnosing an ear infection typically involves a thorough examination by a healthcare professional. Here's how doctors usually diagnose an ear infection:
- Visual inspection: The primary method for diagnosing an ear infection is a visual examination of the ear using an otoscope, a device equipped with a light and magnifier that allows the doctor to see the eardrum and the ear canal. Through this examination, the doctor can check for signs of inflammation, fluid behind the eardrum, and damage to the eardrum, which are indicative of an ear infection.
- Pneumatic otoscope examination: This special otoscope blows a puff of air into the ear to test eardrum movement. A healthy eardrum will move back and forth with the puff of air, whereas an eardrum with fluid buildup behind it will have limited movement.
- Tympanometry: This test involves using a device that seals the ear canal and adjusts air pressure within it. The device measures how the eardrum responds to changes in pressure, which can help detect issues like fluid in the middle ear.
- Hearing tests: In some cases, especially if there are concerns about hearing loss, the doctor may conduct hearing tests. These tests can help determine the impact of the ear infection on hearing and assess the function of the middle ear and eardrum.
- Tympanocentesis: In severe or persistent cases, the doctor might perform tympanocentesis, where a small needle pierces the eardrum and extracts fluid from the middle ear. This fluid can then be tested for bacteria or viruses, helping to guide more specific treatment.
By utilizing these diagnostic methods, healthcare professionals can accurately identify ear infections and their type, whether it's an outer ear infection (otitis externa), middle ear infection (acute otitis media), or otitis media with effusion. Accurate diagnosis is crucial for determining the most effective treatment plan, including using antibiotics, ear tubes, or other treatments to address the infection and prevent complications.
How does this Ear Infection Test work?
Using the Ear Infection Test involves a streamlined process to identify symptoms indicating an ear infection efficiently:
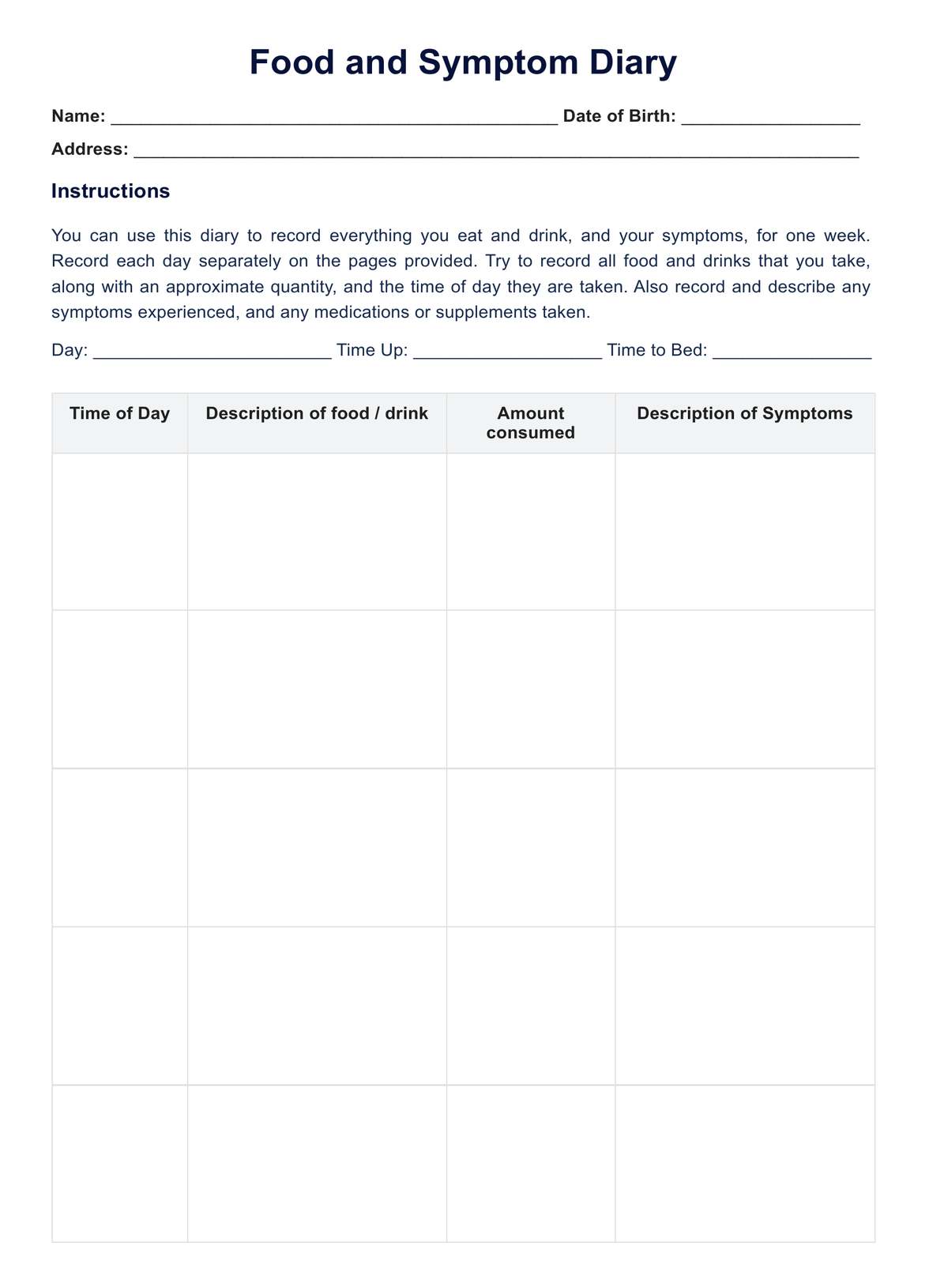
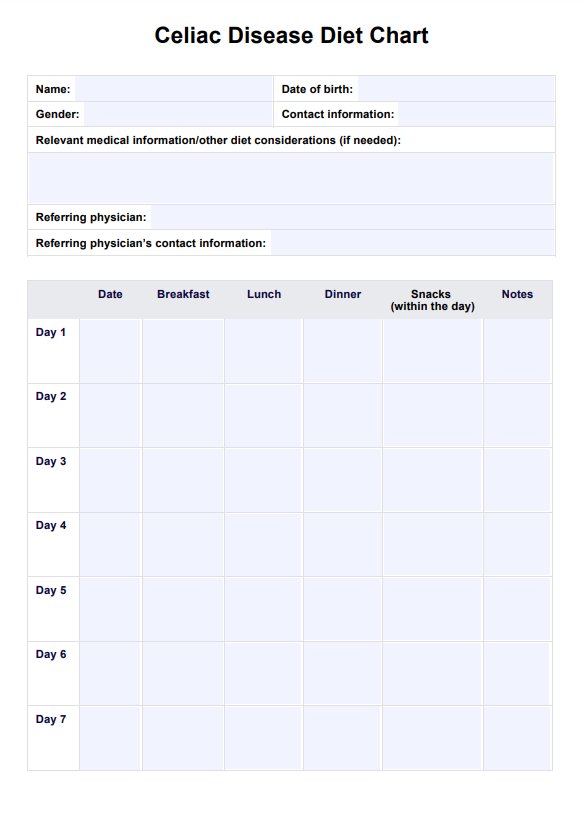
Step 1: Access the template
Healthcare professionals begin by accessing the Ear Infection Test Template through Carepatron. This standardized template facilitates symptom assessment for ear infections.
Step 2: Explain the template and complete the symptom checklist
Before completing the checklist, healthcare professionals explain the purpose of each section to the patient, ensuring they understand how to document their symptoms accurately. After this explanation, patients or healthcare professionals fill in patient details (name, age, date), check off symptoms experienced in the past 48 hours, and note the duration of these symptoms.
Step 3: Document previous occurrences and additional comments
This step involves noting any previous ear infections to identify recurring issues and allows for the inclusion of extra symptoms or concerns not covered by the checklist. It offers a complete picture of the patient's ear health history and any additional factors that might influence diagnosis and treatment.
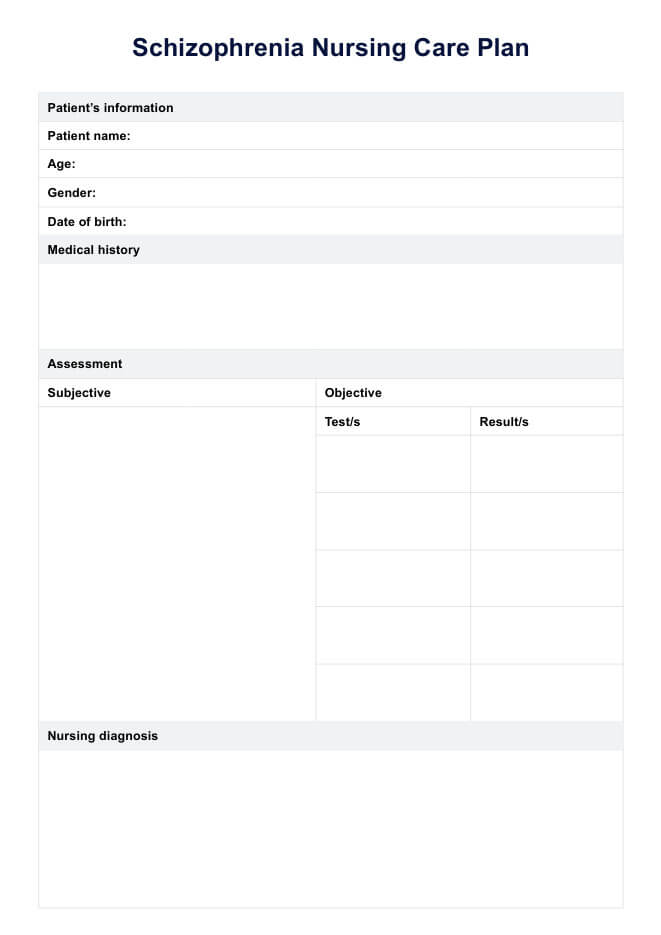
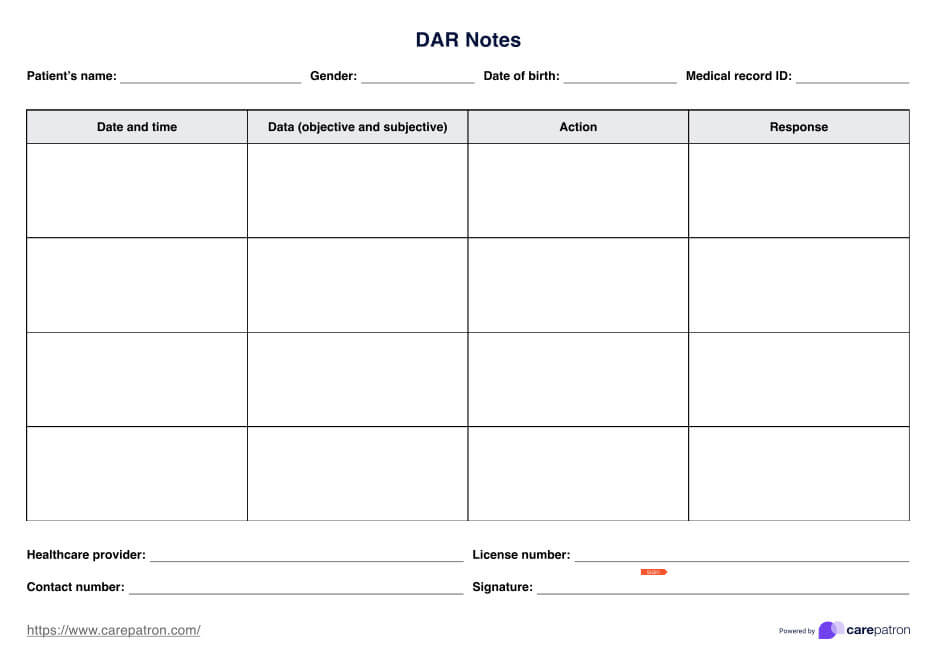
Step 4: Healthcare professional’s analysis and recommendations
The healthcare professional reviews the completed checklist, additional comments, and their observations from any other tests conducted. Based on this information, they can make diagnostic conclusions and recommend further steps, such as additional testing or immediate treatment options.
By consolidating these steps, healthcare professionals can efficiently use the Ear Infection Test to guide the initial assessment of symptoms suggestive of an ear infection. This approach ensures a thorough and organized evaluation, aiding in the accurate diagnosis and management of ear infections.
How are ear infections treated?
Treating ear infections typically involves a combination of methods tailored to the infection's type, severity, and the patient's overall health. Here's an overview of common treatments:
- Medication: Antibiotics are often prescribed for bacterial ear infections, especially in severe cases or those that do not resolve on their own. Pain relievers like acetaminophen or ibuprofen can alleviate pain and reduce fever.
- Ear drops: For infections affecting the outer ear canal (otitis externa), antifungal or antibiotic ear drops may be recommended to treat the infection directly.
- Warm compresses: Applying a warm compress to the affected ear can help relieve pain and discomfort associated with ear infections.
- Fluiddrainage: A healthcare provider may need to drain the fluid when the fluid buildup is significant. This is often done through a minor procedure where a small ear tube is inserted into the eardrum to allow fluid to drain and prevent future buildup.
- Observation: In mild cases, especially those likely caused by a virus, healthcare providers may recommend a wait-and-see approach, as many ear infections resolve on their own without antibiotics. This involves monitoring the infection for a few days to see if it resolves independently without antibiotics.
- Preventive measures: For recurrent ear infections, preventive strategies may include avoiding known triggers, practicing good ear hygiene, and, in some cases, receiving vaccinations that protect against certain infections contributing to ear problems.
- Surgery: In chronic cases, when infections cause significant complications, or following neck surgery, surgical intervention may be necessary to improve ear drainage or repair damage.
Early and appropriate treatment and preventive measures to prevent ear infections can help avoid complications and promote a quicker recovery. Early and appropriate treatment can help prevent complications and promote a quicker recovery.
Commonly asked questions
Yes, you can observe symptoms like ear pain, trouble hearing, or fluid drainage at home, but a healthcare professional should confirm an ear infection diagnosis.
Symptoms such as persistent ear pain, difficulty hearing, fever, and fluid leaking from the ear may indicate an ear infection.
Conditions like temporomandibular joint (TMJ) disorders, dental issues, or throat infections can sometimes mimic ear infection symptoms due to overlapping nerve pathways.