Cranial Nerve Nursing Assessment
Explore our comprehensive nursing guide to cranial nerve assessment – essential insights, procedures, and applications for holistic patient care.


What is a Cranial Nerve Nursing Assessment?
A Cranial Nerve Nursing Assessment is a comprehensive evaluation conducted by healthcare professionals to assess the function and integrity of the nervous system and twelve cranial nerves. These nerves, originating directly from the brain, play a crucial role in various sensory and motor functions within the head and neck region. The assessment aims to identify any abnormalities or dysfunctions that may indicate neurological issues, helping guide diagnosis and appropriate interventions.
The cranial nerves are numbered and named based on their location and function, ranging from the olfactory nerve (I) responsible for the smell to the hypoglossal nerve (XII) controlling tongue movements. Each nerve has a specific role, such as controlling eye movements, facial expressions, and senses like taste and hearing.
During a Cranial Nerve Nursing Assessment, nurses employ a systematic and thorough approach to examine each cranial nerve. This involves assessing sensory functions, motor functions, and reflexes associated with each nerve. For instance, the nurse may evaluate the patient's ability to smell different odors, assess their ability to hear and interpret speech, and observe their facial expressions for signs of asymmetry or weakness.
The assessment also includes examinations like assessing pupillary responses to light, extraocular eye movements, and the patient's ability to follow visual stimuli. Testing the patient's ability to taste, move the tongue, and perform coordinated movements, such as swallowing, is also a critical part of the evaluation. The nurse observes for any signs of abnormalities in facial sensation, such as numbness or tingling, and checks the strength and coordination of the muscles associated with chewing and facial expressions.
A Cranial Nerve Nursing Assessment is particularly valuable in a variety of healthcare settings, including neurology, critical care, and general medical-surgical units. It aids in the early detection of neurological issues, which can be essential for prompt intervention and management. This assessment requires observational skills, patient interaction, and knowledge of the anatomy and functions of the cranial nerves. Any deviations from normal findings may prompt further diagnostic investigations and collaboration with other healthcare professionals to ensure a comprehensive understanding of the patient's neurological status.
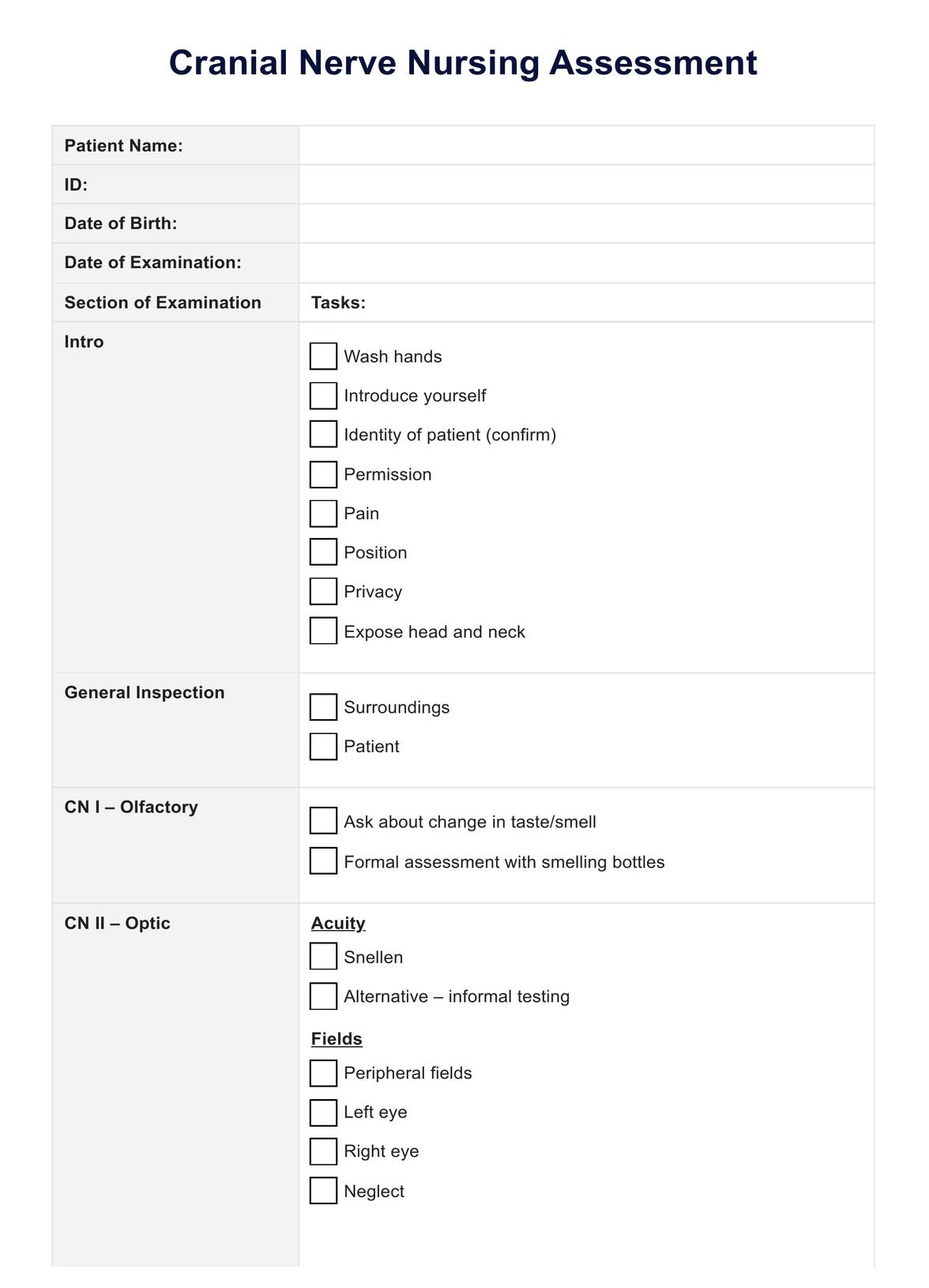
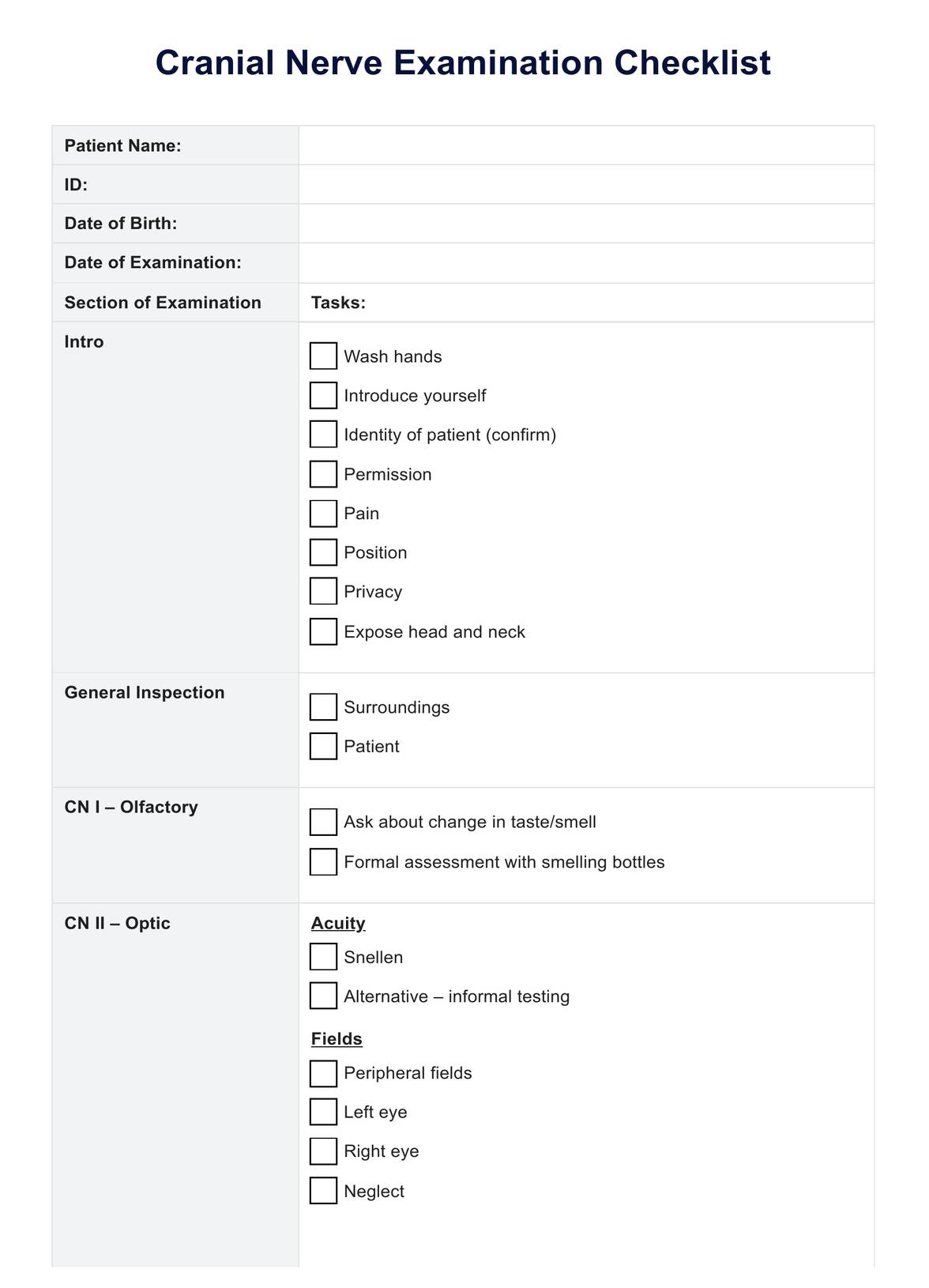
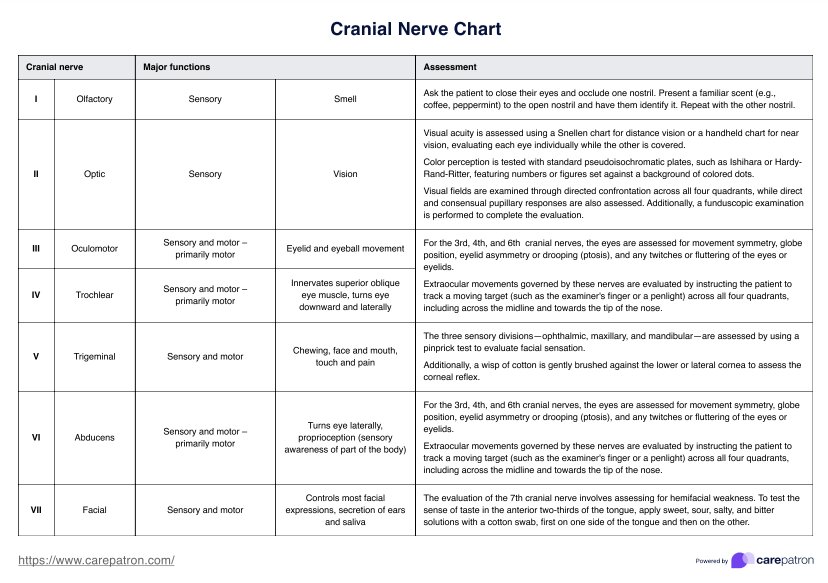
Cranial Nerve Nursing Assessment Template
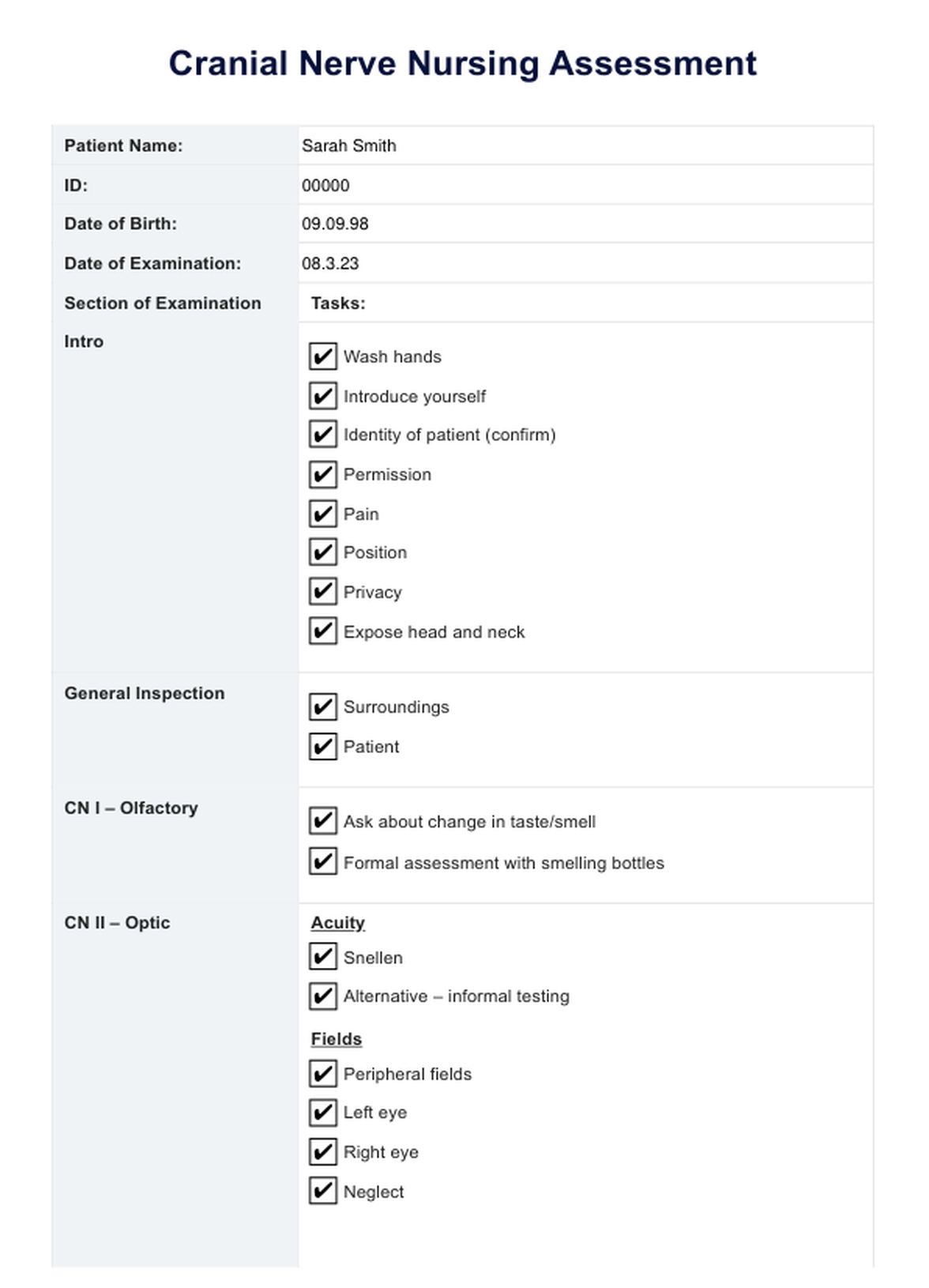
Cranial Nerve Nursing Assessment Example
What does this assessment cover?
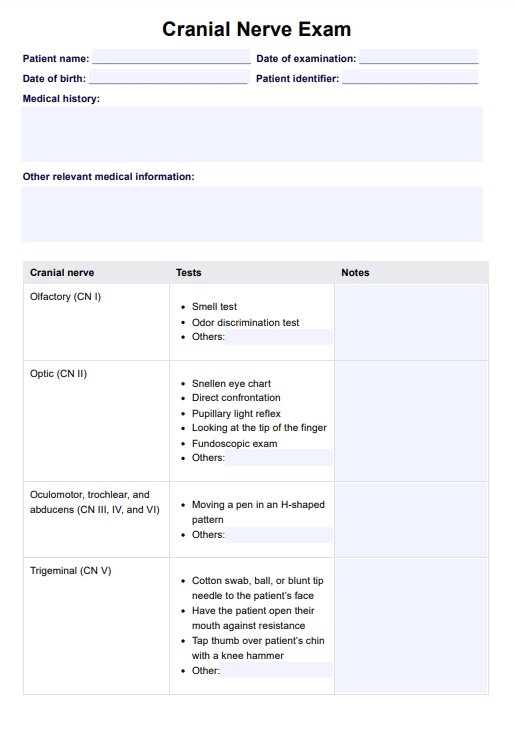
The cranial nerve nursing assessment is a methodical assessment that individually evaluates the function of each cranial nerve. Typically conducted in a hospital setting with readily available equipment (Reese et al., 2023), this examination covers various methods for assessing each nerve's functionality.
Let's briefly explore the functions assessed for each cranial nerve in this examination.
Olfactory nerve (CN I):
Associated with smell, olfactory nerve tests involve questioning changes in taste or smell and more formal assessments using scent bottles.
Optic nerve (CN II):
Assessed through tests of visual acuity, fields, and reflexes, with informal testing including reading tasks and formal testing involving charts like the Snellen eye chart.
Oculomotor nerve (CN III), trochlear nerve (CN IV), abducens nerve (CN VI):
These nerves, governing eye movement, are assessed to evaluate their functioning.
Trigeminal nerve (V):
Comprising ophthalmic, maxillary, and mandibular divisions, the trigeminal nerve is tested through cotton wool tests and facial muscle movements.
Facial nerve (CN VII):
Associated with facial expression muscles, assessment involves asking patients to make specific facial expressions and evaluating muscle strength.
Vestibulocochlear nerve (auditory) (CN VIII):
Responsible for hearing and balance, it can be tested through a whispered voice test or formally through Rinne's or Weber's tests.
Glossopharyngeal nerve (CN IX):
Innervating the tongue and pharynx, it's involved in functions like swallowing, the gag reflex, saliva production, and speech.
Vagus nerve (CN X):
Extensively associated with structures from the pharynx to the abdomen, it can manifest symptoms such as a hoarse voice or uvula asymmetry with palsy.
Spinal accessory nerve (CN XI):
Associated with sternocleidomastoid and trapezius muscles, focusing on these muscles is typical in its assessment due to its proximity to the vagus nerve.
Hypoglossal nerve (CN XII):
Innervating tongue muscles and palsy may result in tongue asymmetry or muscle wasting. The examination covers these aspects comprehensively.
How does a cranial nerve assessment work?
Cranial nerve assessment is commonly incorporated into comprehensive examinations, such as the Nurse Neurological Assessment and the HEENT Assessment, encompassing the head and neck examination. Within these extensive evaluations, professionals perform various tasks, including specific tests like the PERRLA Eye Exam and Weber and Rinne hearing tests.
Given the multifaceted nature of neurological examinations, having checklists or similar resources becomes essential for professionals to track completed tasks and pending assessments. This is where the cranial nerve assessment template proves invaluable. Detailing each cranial nerve, its vocabulary, functions, and the required assessment procedures, the chart serves as a reference tool.
For instance, in evaluating the cranial nerves, the template aids professionals in systematically examining each nerve. Taking the Olfactory Nerve as an example, responsible for the sense of smell, the chart guides the examiner to conduct a smelling test with various substances like coffee, cloves, and peppermint. The comprehensive information provided by the cranial nerve nursing template allows professionals to easily refresh their memory on assessment procedures when needed, promoting efficiency and accuracy in examinations.
Interpreting the results of the cranial nerve assessments
Interpreting the results of cranial nerve assessments involves evaluating the findings from each specific test associated with individual cranial nerves. Here's a general guide on interpreting results:
Normal vs. abnormal findings:
- Understand the expected or normal responses for each cranial nerve test.
- Identify any deviations from the norm, as these may indicate abnormalities or dysfunction.
Bilateral comparison:
- Compare findings bilaterally, as some cranial nerves have paired structures (e.g., optic nerves, facial nerves).
- Note any asymmetry or differences between the right and left sides.
Quantitative and qualitative assessment:
- For certain tests, such as visual acuity or taste sensation, quantitative measures may be obtained (e.g., 20/20 vision).
- Other assessments, like facial expressions or eye movements, may involve qualitative observations (e.g., symmetry of facial movements).
Reflexes and Responses:
- Assess reflexes associated with specific cranial nerves, such as pupillary responses (cranial nerves II and III).
- Observe patient responses to sensory stimuli, like taste or smell, associated with specific cranial nerves.
Documentation:
- Document the findings, including any abnormalities, deviations, or patient responses.
- Record quantitative measurements and note qualitative observations for a comprehensive record.
Clinical Correlation:
- Relate the cranial nerve assessment findings to the patient's overall clinical presentation.
- Consider other neurological or medical factors that may influence cranial nerve function.
Diagnostic considerations:
- Abnormalities in specific cranial nerve assessments may suggest certain neurological or systemic disorders.
- Collaborate with other healthcare professionals or specialists to further investigate and confirm diagnoses.
Patient history:
- Consider the patient's medical history, as pre-existing conditions, medications, or recent trauma may influence cranial nerve function.
Follow-Up assessment:
- If abnormalities are identified, schedule follow-up assessments to monitor changes over time.
- Adjust the assessment plan based on the patient's progress or response to interventions.
Consultation and collaboration:
- Consult with neurologists or other specialists for complex cases.
- Collaborate with the healthcare team to ensure a comprehensive understanding of the patient's condition.
Remember that interpreting cranial nerve assessments requires a combination of knowledge, clinical judgment, and consideration of the patient's unique characteristics. If you are not a healthcare professional, it's crucial to seek guidance from qualified healthcare providers for accurate interpretation and appropriate action.
Next steps
Following a cranial nerve assessment, the next steps involve interpreting the findings and determining appropriate actions based on the results. Here is a general guideline for the next steps:
Interpretation of findings
- Analyze the results of each cranial nerve test, comparing them to expected norms.
- Identify any abnormalities, asymmetries, or deviations from the expected responses.
Documentation
- Document the assessment findings, noting any observed abnormalities or noteworthy responses.
- Include relevant details such as quantitative measurements, qualitative observations, and patient responses.
Clinical correlation
- Relate the cranial nerve assessment results to the patient's overall clinical presentation.
- Consider how the findings may align with or provide insights into the patient's symptoms or medical history.
Differential diagnosis
- Develop a preliminary differential diagnosis based on the cranial nerve assessment results.
- Consider potential neurological, ophthalmic, or systemic conditions associated with identified abnormalities.
Further diagnostic testing
- Determine if additional diagnostic tests are necessary to confirm or further investigate suspected conditions.
- Imaging studies, such as MRI or CT scans, may be ordered to assess the structural integrity of cranial nerves or related structures.
Consultation with specialists
- If necessary, consult with specialists such as neurologists, ophthalmologists, or otolaryngologists to obtain expert opinions and insights.
- Collaborate with the healthcare team to ensure a multidisciplinary approach to patient care.
Treatment planning
- Develop a treatment plan based on the identified issues.
- Treatment may involve medical interventions, therapeutic strategies, or surgical procedures depending on the underlying cause.
Patient Education
- Educate the patient about the assessment findings, the suspected condition, and the proposed treatment plan.
- Provide information on prognosis, potential interventions, and any lifestyle modifications if applicable.
Follow-Up assessments
- Schedule follow-up assessments to monitor changes in cranial nerve function and the patient's overall condition.
- Adjust the treatment plan as needed based on the patient's response to interventions.
Reassessment
- Periodically reassess cranial nerve function to track improvements or detect any recurrence of abnormalities.
- Modify the care plan as necessary to address ongoing or new concerns.
Documentation of progress
- Continuously document the patient's progress, including improvements or any complications.
- Maintain clear and updated records to facilitate communication among healthcare providers.
Always remember that the specific next steps may vary depending on the context, the patient's overall health, and the healthcare setting. Healthcare professionals should exercise clinical judgment and follow established protocols to ensure comprehensive and patient-centered care. If you are not a healthcare professional, it's crucial to ask the patient or to seek guidance from qualified healthcare providers for accurate interpretation and appropriate action.
Research and evidence
Cranial nerve examinations are anchored in extensive research and evolving knowledge of neuroanatomy and physiology. The intricate network of twelve pairs of cranial nerves, emerging directly from the brain, governs distinct sensory and motor functions.
Numerous research studies have unveiled the specific roles of each cranial nerve, offering insights into their pathways, functions, and potential abnormalities. Advanced imaging modalities, such as Magnetic Resonance Imaging (MRI), have allowed researchers to visualize the complex structures associated with cranial nerves, deepening our understanding of their anatomical relationships.
These investigations have refined examination techniques and established correlations between specific cranial nerve abnormalities and various neurological disorders. This evidence-based approach ensures that cranial nerve examinations go beyond routine procedures, rooted in a robust scientific foundation. This foundation enables healthcare professionals to detect abnormalities, make precise diagnoses, and implement appropriate interventions.
Despite their historical significance, medical imaging techniques have somewhat taken precedence over cranial nerve examinations in recent years (Damodaran et al., 2014). The diagnostic specificity of the cranial nerve exam is challenged by the potential for multiple diagnoses leading to impairment in one or more cranial nerves' functions (Taylor et al., 2021). However, standardizing the cranial nerve exam procedure can mitigate this limitation, ensuring the most reliable results from the examination.
Why is this nerve assessment useful for nurses?
The cranial nerve assessment is highly useful for nurses for several reasons, primarily contributing to their ability to provide comprehensive and patient-centered care. Here are key reasons why the cranial nerve assessment is beneficial for nurses:
Early detection of neurological issues
By conducting a cranial nerve assessment, nurses can identify early signs of neurological dysfunction or abnormalities. Early detection allows for prompt intervention and may prevent the progression of neurological conditions.
Holistic patient assessment
The cranial nerve assessment is a crucial component of a holistic nursing assessment. It provides insights into the patient's neurological status, complementing other assessments related to physical, psychosocial, and environmental factors.
Informed clinical decision-making
Nurses use cranial nerve assessment findings to make informed clinical decisions. Abnormalities may prompt further diagnostic testing, consultation with specialists, or adjustments to the patient's care plan.
Monitoring patient recovery
For patients with neurological conditions or those recovering from surgeries or injuries affecting the cranial nerves, regular assessments help nurses monitor changes in neurological function over time. This supports ongoing care planning and adaptation of interventions.
Communication with the healthcare team
Clear documentation of cranial nerve assessment findings facilitates effective communication among healthcare professionals. Nurses can convey important information to physicians, neurologists, and other team members, fostering collaboration in patient care.
Tailoring patient-centered care
Understanding cranial nerve function allows nurses to tailor care plans to the patient's specific needs. For instance, modifications in feeding strategies may be implemented for patients with impaired swallowing (cranial nerves IX and X).
Enhanced patient education
Nurses can educate patients about the results of the cranial nerve assessment, helping them understand their condition, potential symptoms, and the rationale behind recommended interventions. This empowers patients to actively participate in their care.
Prevention of complications
In certain situations, cranial nerve dysfunction may pose risks for complications, such as aspiration due to impaired swallowing. Nurses can implement preventive measures and closely monitor patients at risk to mitigate potential issues.
Assessment of neurological emergencies
In emergencies, such as head injuries or strokes, rapid cranial nerve assessments by nurses contribute to the initial assessment of neurological status. This information is crucial for determining the urgency and nature of interventions.
Compliance with standards of care
Including cranial nerve assessment as part of routine nursing practice aligns with standards of care and best practices. It ensures that nurses are conducting thorough assessments and addressing neurological aspects of patient well-being.
Adaptation of care for special populations
For vulnerable populations such as pediatric or elderly patients, nurses can adapt the cranial nerve assessment to account for age-related variations and tailor care accordingly.
References
Damodaran O, Rizk E, Rodriguez J, Lee G. (2014) Cranial nerve assessment: a concise guide to clinical examination. Clin Anat. 27(1):25-30.
Reese V, M Das J, Al Khalili Y. Cranial Nerve Testing. [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Taylor A, Mourad F, Kerry R, Hutting N. (2021) A guide to cranial nerve testing for musculoskeletal clinicians. J Man Manip Ther. 29(6):376-389. doi: 10.1080/10669817.2021.1937813.
Commonly asked questions
A cranial nerve nursing assessment is crucial for evaluating the neurological function of the twelve cranial nerves. It helps nurses identify early signs of dysfunction, make informed clinical decisions, and tailor patient-centered care plans.
The assessment involves a systematic examination of each cranial nerve, assessing sensory and motor functions. Techniques include testing vision, hearing, facial movements, and evaluating reflexes. The goal is to identify abnormalities or deviations from expected responses.
A cranial nerve nursing assessment is essential in various clinical scenarios, including patients with head injuries, neurological disorders, or those undergoing surgeries affecting the cranial nerves. It is also valuable in assessing conditions such as strokes, facial paralysis, and sensory impairments.