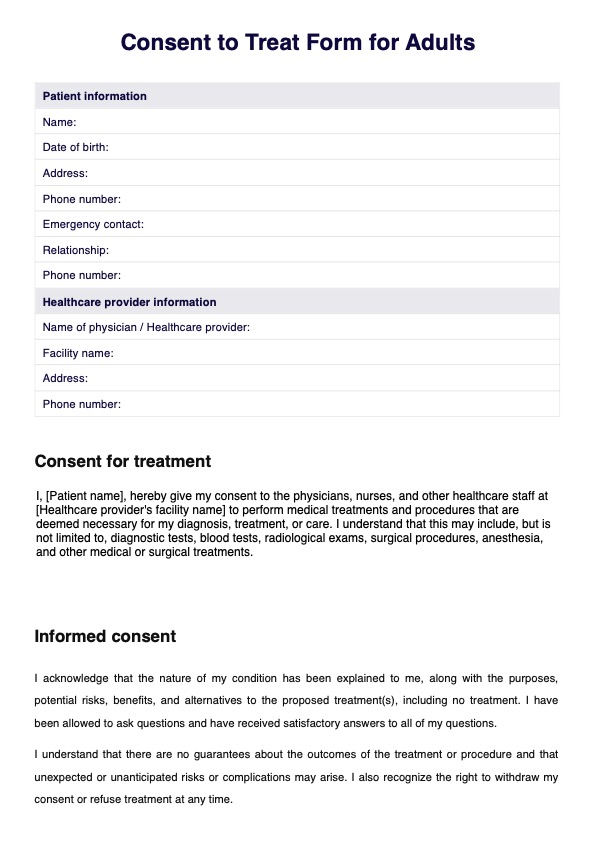
To write a simple consent form, start by clearly stating its purpose and the specific treatment or procedure it covers. Include sections for patient information (name, date of birth, contact details), a detailed explanation of the treatment (including its risks and benefits), the patient's right to refuse treatment, and a signature line for the patient and witness (if applicable).
Ensure the language is straightforward and understandable to non-medical readers.