The test assesses chronic fatigue syndrome (CFS) by identifying primary symptoms of profound fatigue and secondary symptoms, such as muscle pain, memory problems, headaches, unrefreshing sleep, or insomnia.
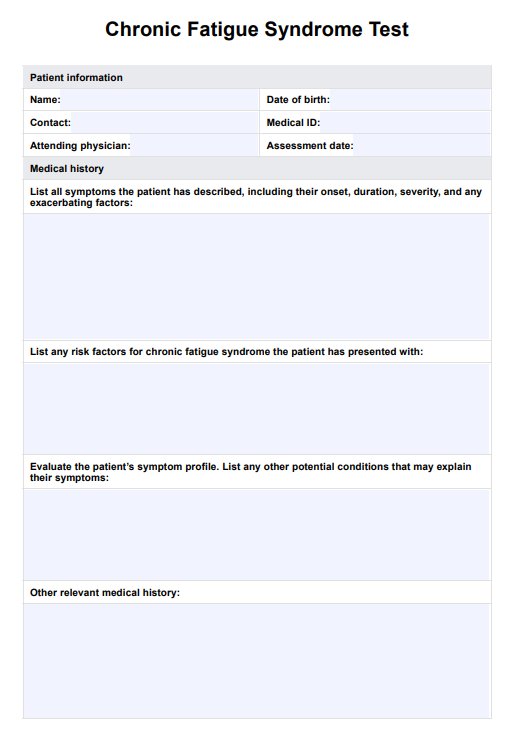
Chronic Fatigue Syndrome Test
Download a free Chronic Fatigue Syndrome Test template, a tool specifically designed to facilitate the process of diagnosing clients with chronic fatigue syndrome (ME/CFS)
Chronic Fatigue Syndrome Test Template
Commonly asked questions
No, there is no single test for CFS. This resource serves as a valuable tool for recognizing patterns and symptoms associated with CFS, aiding in the absence of a specific diagnostic test.
Flu-like symptoms such as low-grade fever, chills, sore throat, swollen lymph nodes, and general malaise, may also be experienced. Some people with CFS experience orthostatic intolerance upon standing or sitting upright (e.g. dizziness, lightheadedness, a rapid heart rate). Gastrointestinal symptoms, such as irritable bowel syndrome (IBS), abdominal pain, and nausea, can also occur.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











