Pelvic Floor Exam
Explore our pelvic floor exam guide for a comprehensive overview, including preparation, procedure insights, and understanding results. Your pelvic health matters!


What is a Pelvic Floor Exam?
A pelvic floor exam is a medical procedure designed to assess the health and function of the pelvic floor muscles, ligaments, and other connective tissue in both men and women. The pelvic floor is a complex network of muscles that support the pelvic organs, including the bladder, uterus, and rectum. This exam is typically performed by a healthcare provider, such as a gynecologist or urologist, and is crucial for diagnosing and treating various pelvic floor disorders.
The patient is usually asked to lie on an examination table with their legs supported in stirrups during the exam. The healthcare provider begins by conducting a thorough external examination of the genital and pelvic regions, checking for abnormalities, swelling, or signs of discomfort. Following the external assessment, an internal examination is often performed, involving the insertion of a gloved and lubricated finger into the vagina or rectum, depending on the specific concerns being addressed.
The internal examination allows the healthcare provider to evaluate the pelvic floor muscles' strength, tone, and flexibility. They may also assess for any tenderness, pain, or unusual sensations indicating dysfunction. For men, the pelvic exam may involve a rectal examination to determine the condition of the pelvic floor muscles and the prostate gland.
In some instances, additional tools or instruments may be used during an internal pelvic exam, such as a speculum, for better visualization of the vaginal canal. The healthcare provider may gently apply pressure to different areas of the pelvic floor to identify any weaknesses or areas of concern. Throughout the exam, clear communication between the healthcare provider and the patient is essential, ensuring that the patient feels comfortable and informed about each process step.
Pelvic floor exams are crucial for diagnosing conditions such as pelvic organ prolapse, urinary incontinence, and pelvic pain disorders. The information gathered from the exam helps guide treatment plans, which may include pelvic floor physical therapy, lifestyle modifications, or surgical interventions.
Regular pelvic floor exams are essential for women during routine gynecological check-ups and for individuals experiencing symptoms like pelvic pain, bladder dysfunction, or sexual dysfunction. The pelvic floor exam is vital in promoting pelvic health and addressing issues that may impact a person's quality of life.
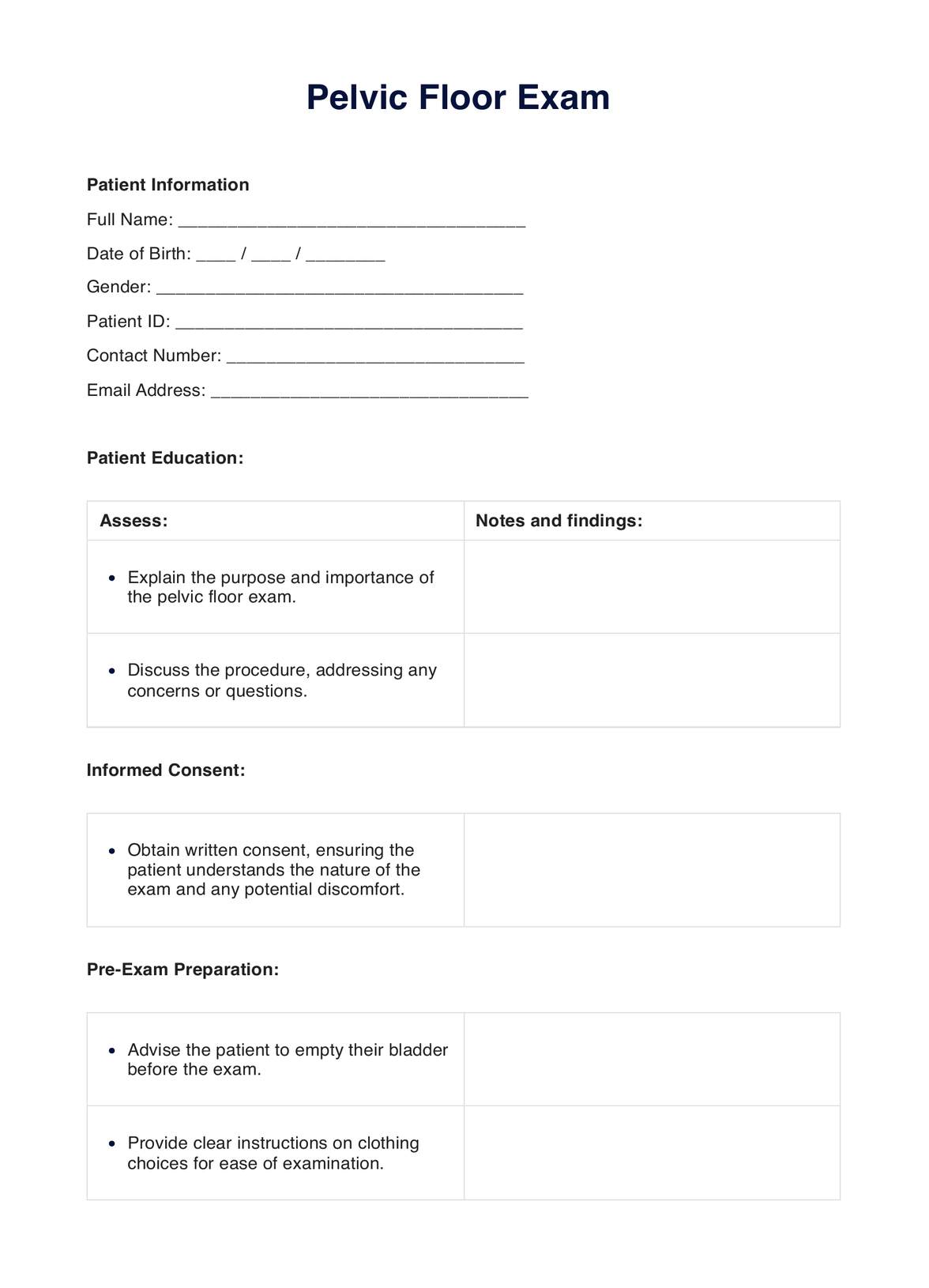
Pelvic Floor Exam Template
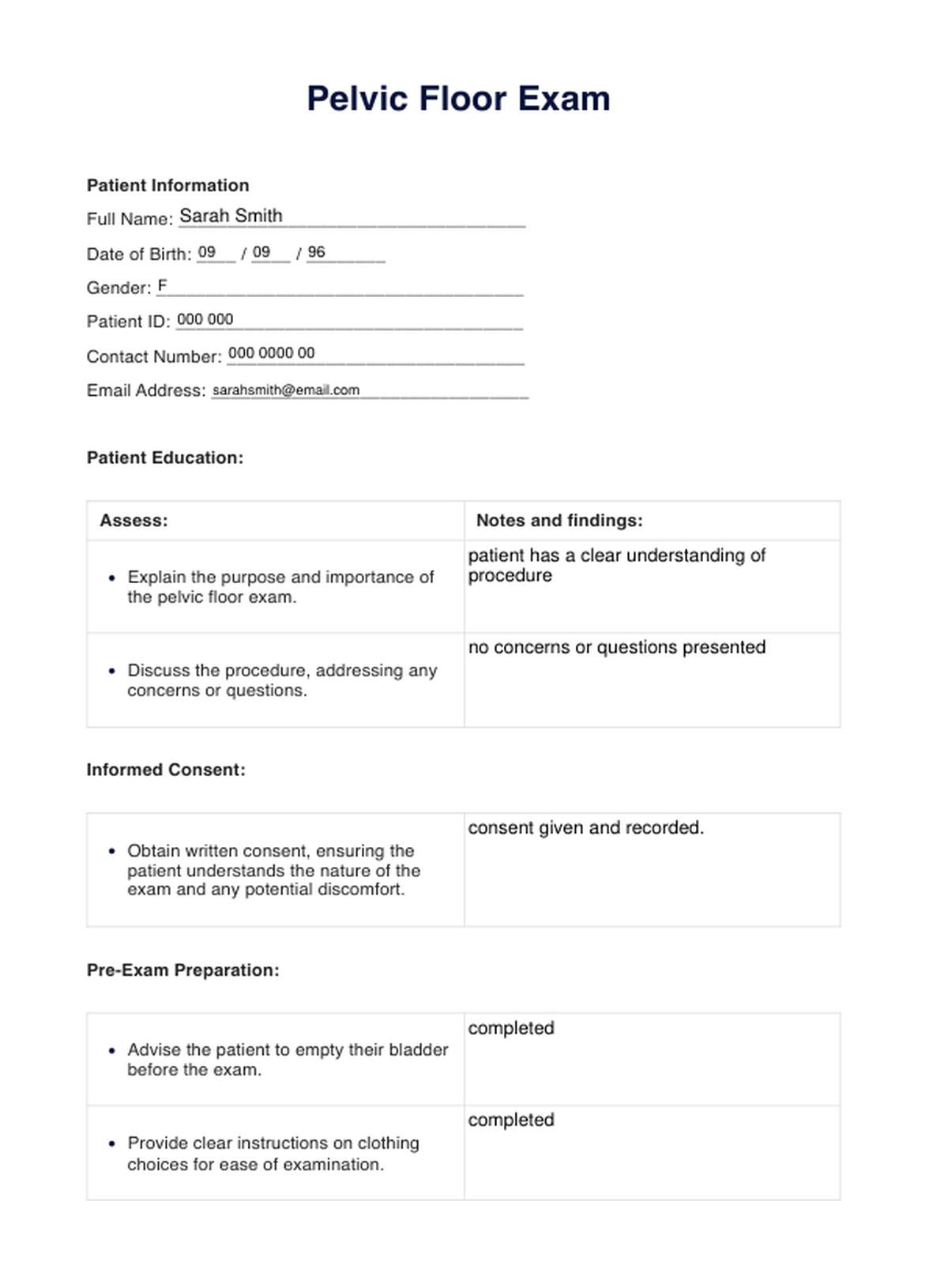
Pelvic Floor Exam Example
Brief introduction to the function of the pelvis
The pelvis is a bony structure located at the base of the spine, connecting the spine to the lower limbs. Comprising the sacrum, coccyx, and two hip bones (ilium, ischium, and pubis), the pelvis is a central support for the body's weight and is crucial in various physiological functions. Its primary functions include providing support and stability for the spine, transmitting the upper body's weight to the lower limbs, and accommodating and protecting the pelvic organs, such as the bladder, reproductive organs, and rectum.
Additionally, the pelvis is essential for mobility, as a point of attachment for muscles and ligaments that contribute to posture, walking, and overall movement. Its structure and function are integral to activities ranging from standing and sitting to childbirth, making the pelvis a key component of the body's structural and functional framework.
How does a Pelvic Floor Exam work?
During a pelvic floor exam, a healthcare provider assesses the health and functionality of the pelvic floor muscles and associated structures. The procedure is typically conducted in a medical office or clinic, involving external and internal components of routine pelvic exams.
External examination
The patient usually begins lying on an examination table with their legs supported in stirrups. The healthcare provider starts with an external examination, inspecting the genital and pelvic regions for any visible abnormalities, swelling, or signs of discomfort. They may also evaluate the overall pelvic structure and alignment.
Internal examination
Following the external assessment, the healthcare provider performs an internal examination. This involves the insertion of a lubricated, gloved finger into the vagina for women or the rectum for men. The choice of insertion point depends on the specific concerns being addressed. The internal exam allows the healthcare provider to assess the pelvic floor muscles' strength, tone, and flexibility.
Muscle tone and strength assessment
During the internal examination, the healthcare provider may assess the pelvic floor muscles by asking the patient to perform specific actions, such as contracting and relaxing the muscles. This helps evaluate muscle tone, strength, and coordination. Any tenderness, pain, or abnormalities detected during this process can provide important diagnostic information.
Additional tools or instruments
In some cases, additional tools or instruments may be used, such as a speculum for better visualization of the vaginal canal or a rectal examination for men to assess the condition of the pelvic floor muscles and the prostate gland.
Communication and comfort
Clear communication between the healthcare provider and the patient is crucial throughout the exam. The patient should feel informed about each process step, and the healthcare provider should address any concerns or questions. Maintaining a comfortable and respectful environment is essential to ensure the patient's well-being during the examination.
Interpreting the results of the exam
Interpreting the results of a pelvic floor exam involves assessing the findings to understand the health and function of the pelvic floor muscles and related structures. The healthcare provider considers various aspects to determine if there are any abnormalities or conditions that require attention. Here are key elements in interpreting the results:
Muscle tone and strength
The healthcare provider evaluates the tone and strength of the pelvic floor muscles. Normal muscle tone is essential for supporting pelvic organs and maintaining continence. Weakness or excessive tension in these muscles may be indicative of issues such as pelvic floor dysfunction, which can contribute to conditions like urinary incontinence or pelvic pain.
Coordination and reflexes
Coordination and reflexes of the pelvic floor muscles are assessed during the examination. Proper coordination ensures effective pelvic floor muscle function. Dysfunctional reflexes or poor coordination may be associated with problems like urinary or fecal incontinence.
Tenderness or pain
The healthcare provider notes any tenderness or pain experienced by the patient during the exam. Pain or discomfort may indicate underlying issues like muscle spasms, inflammation, or pelvic floor disorders. Identifying the source of pain is crucial for developing an appropriate treatment plan.
Visualization of structures
If additional tools or instruments were used, the healthcare provider assesses the visualization of pelvic structures. This may include checking for any abnormalities in the vaginal canal or rectum that could contribute to pelvic health concerns.
Patient feedback
The patient's feedback and communication during the exam provide valuable information. Any symptoms, concerns, or discomfort reported by the patient contribute to the overall assessment. Open communication is essential to comprehensively understand the patient's pelvic health.
Integration with medical history
Results are often integrated with the patient's medical history and any presenting symptoms. This comprehensive approach helps identify potential causes and contributing factors to pelvic floor issues.
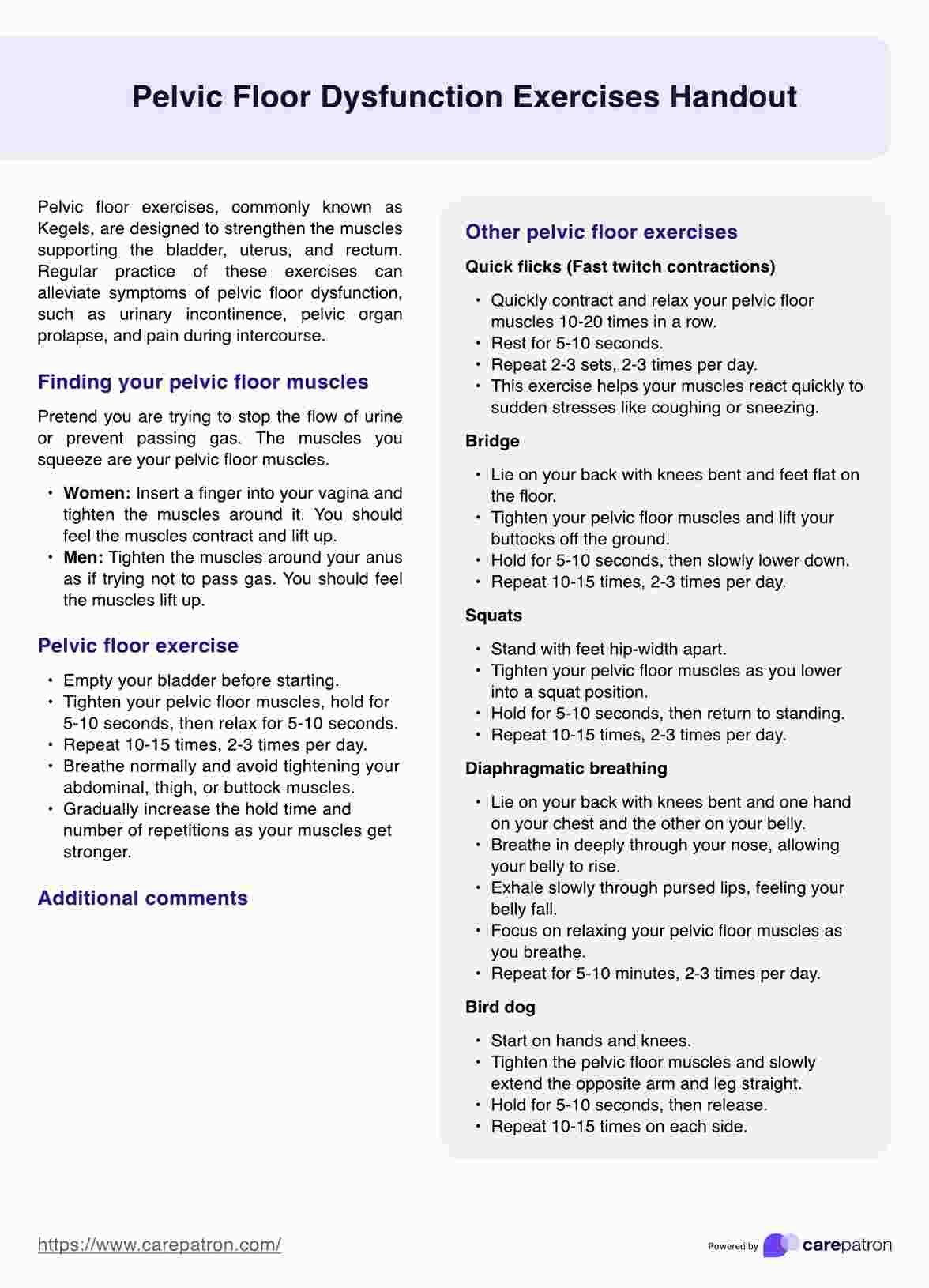
Pelvic floor dysfunction treatment plan
- Pelvic floor physical therapy: Pelvic floor physical therapy is a cornerstone of PFD treatment. A specialized physical therapist works with the patient to address muscle imbalances, weakness, or tension in the pelvic floor. Therapeutic exercises, biofeedback, and manual techniques are often employed to improve muscle function and coordination.
- Biofeedback: Biofeedback involves using sensors to provide visual or auditory feedback about muscle activity. This helps patients become more aware of and control their pelvic floor muscles. Biofeedback can be used in conjunction with pelvic floor exercises to enhance effectiveness.
- Behavioral and lifestyle modifications: Lifestyle changes may include dietary adjustments to manage bowel habits, such as addressing constipation or diarrhea. Behavioral modifications may involve optimizing fluid intake, establishing regular bathroom habits, and avoiding straining during bowel movements.
- Bladder and bowel training: For those experiencing urinary or fecal incontinence, bladder and bowel training techniques may be implemented. This includes scheduled bathroom breaks, timed voiding, and techniques to strengthen sphincter muscles.
- Medications: In some cases, medications may be prescribed to manage symptoms associated with pelvic floor dysfunction. For example, medications for overactive bladder or constipation may be recommended based on the specific symptoms present.
- Relaxation techniques: Techniques such as deep breathing, relaxation exercises, and mindfulness can help manage muscle tension and stress, contributing to the overall improvement of pelvic floor function.
- Electrical stimulation: Electrical stimulation involves the use of low-level electrical currents to stimulate pelvic floor muscles. This can be done with pelvic floor exercises to enhance muscle strength and coordination.
- Surgery: In cases where conservative treatments are ineffective, surgery may be considered. Surgical options vary depending on the specific pelvic floor disorder and may include procedures to repair pelvic organ prolapse, address muscle abnormalities, or treat urinary or fecal incontinence.
- Counseling and psychotherapy: Emotional factors can contribute to pelvic floor dysfunction. Counseling or psychotherapy may be beneficial for addressing stress, anxiety, or trauma that could be impacting pelvic floor health.
- Education and support: Providing education about pelvic floor health, proper body mechanics, and strategies for symptom management is crucial. Support groups or counseling can also be valuable in offering emotional support and sharing experiences with others facing similar challenges.
Commonly asked questions
A pelvic floor exam is a medical procedure that assesses the health and function of the pelvic floor muscles and associated structures. It is performed to diagnose and address conditions such as pelvic organ prolapse, urinary incontinence, and pelvic pain disorders.
While some patients may experience mild discomfort, a pelvic floor exam is generally not painful. Clear communication with the healthcare provider is essential, and they can adjust their approach to ensure the patient's comfort during the examination.
The frequency of pelvic floor exams varies based on individual health needs and risk factors. For women, regular pelvic exams are often part of routine gynecological check-ups. Individuals experiencing pelvic health symptoms or conditions may require more frequent assessments, as determined by their healthcare provider.