Necrotizing Fasciitis Diagnosis Guidelines Handout
Learn all about necrotizing fasciitis diagnosis with our comprehensive guidelines handout and example. Get Carepatron's free PDF download now!


What is necrotizing fasciitis?
Necrotizing fasciitis, often referred to as a "flesh-eating" disease, is a severe and rapidly progressing bacterial infection that targets the body's soft tissues. This necrotizing soft tissue infection spreads swiftly, causing widespread tissue damage and, if left untreated, can lead to life-threatening complications.
The infection typically starts in the deeper layers of the skin, such as the fascia, subcutaneous tissue, and muscle, and can quickly spread along the fascial planes. It is primarily caused by certain strains of bacteria, most commonly Streptococcus pyogenes (group A streptococcus) and Staphylococcus aureus. However, other bacteria can also contribute to its development.
Necrotizing Fasciitis presents with severe pain, swelling, redness, and fever at the infected site. As the infection progresses, the affected skin may become discolored and develop blisters filled with fluid. Without prompt medical intervention, necrotizing fasciitis can rapidly lead to tissue death and systemic infection.
Treatment typically involves aggressive antibiotic therapy, surgical debridement to remove infected tissue, and in some cases, hyperbaric oxygen therapy to promote tissue healing. Despite advances in medical care, necrotizing fasciitis remains a medical emergency, and prompt diagnosis and treatment are essential to improve outcomes and reduce the risk of mortality associated with this severe necrotizing infection.
Causes of Necrotizing Fasciitis
Necrotizing Fasciitis can develop due to various factors, primarily bacterial infections that invade the body's soft tissues. Below are the main causes:
- Bacterial infections, including Streptococcus pyogenes (group A streptococcus) and Staphylococcus aureus.
- Bacteria enter through breaks in the skin, such as cuts, wounds, surgical incisions, or insect bites.
- Complications from other infections, such as cellulitis or surgical site infections.
- A weakened immune system can increase susceptibility to bacterial infections.
- Certain underlying health conditions, such as diabetes, obesity, or peripheral vascular disease, compromise blood flow and tissue healing.
- Intravenous drug use, which can introduce bacteria directly into the bloodstream, increasing the risk of soft tissue infections.
These factors can contribute to the development of necrotizing fasciitis, leading to rapid tissue destruction and potentially life-threatening complications if not promptly treated.
Symptoms of Necrotizing Fasciitis
Necrotizing Fasciitis manifests with distinct symptoms that indicate the severity and rapid progression of the infection. Recognizing these symptoms is crucial for prompt medical intervention. Common symptoms include:
- Severe pain at the site of infection, often disproportionate to the visible wound or injury.
- Swelling, redness, and warmth around the affected area.
- Fever and chills, indicating systemic infection.
- Rapid progression of symptoms within hours, including skin discoloration, blistering, or necrosis (tissue death).
- Presence of gas bubbles under the skin, known as crepitus.
- Malaise and fatigue, accompanying systemic inflammation and infection.
These symptoms may vary depending on the location and extent of the infection. However, the rapid onset and severe nature of symptoms are characteristic of necrotizing fasciitis and necessitate immediate medical attention for diagnosis and treatment.
Treatment for Necrotizing Fasciitis
Prompt and aggressive treatment is essential to manage necrotizing fasciitis effectively and prevent serious complications. Treatment typically involves a combination of medical interventions aimed at controlling the infection, removing necrotic tissue, and supporting tissue healing. Below are the key components of treatment:
- Antibiotic therapy: Administering broad-spectrum antibiotics intravenously to target the causative bacteria and prevent further spread of infection.
- Surgical debridement: Surgically removing necrotic tissue and infected material to halt the progression of the infection and promote wound healing.
- Hyperbaric oxygen therapy: Some cases may benefit from hyperbaric oxygen therapy, which involves breathing pure oxygen in a pressurized chamber to enhance tissue oxygenation and promote healing.
- Supportive care: Providing supportive care to manage pain, fever, and other symptoms associated with the infection. This may include intravenous fluids, pain medications, and monitoring for complications.
- Wound care: Proper wound care and dressing changes to keep the affected area clean, prevent secondary infections, and promote healing.
- Monitoring and follow-up: Close monitoring of the patient's condition, including vital signs, laboratory tests, and imaging studies, to assess treatment response and detect any complications early.
Treatment for necrotizing fasciitis often requires collaboration among various healthcare professionals, including infectious disease specialists, surgeons, and wound care specialists.
Necrotizing Fasciitis Diagnosis Guidelines Handout Template
Necrotizing Fasciitis Diagnosis Guidelines Handout Example
How do healthcare practitioners diagnose necrotizing fasciitis?
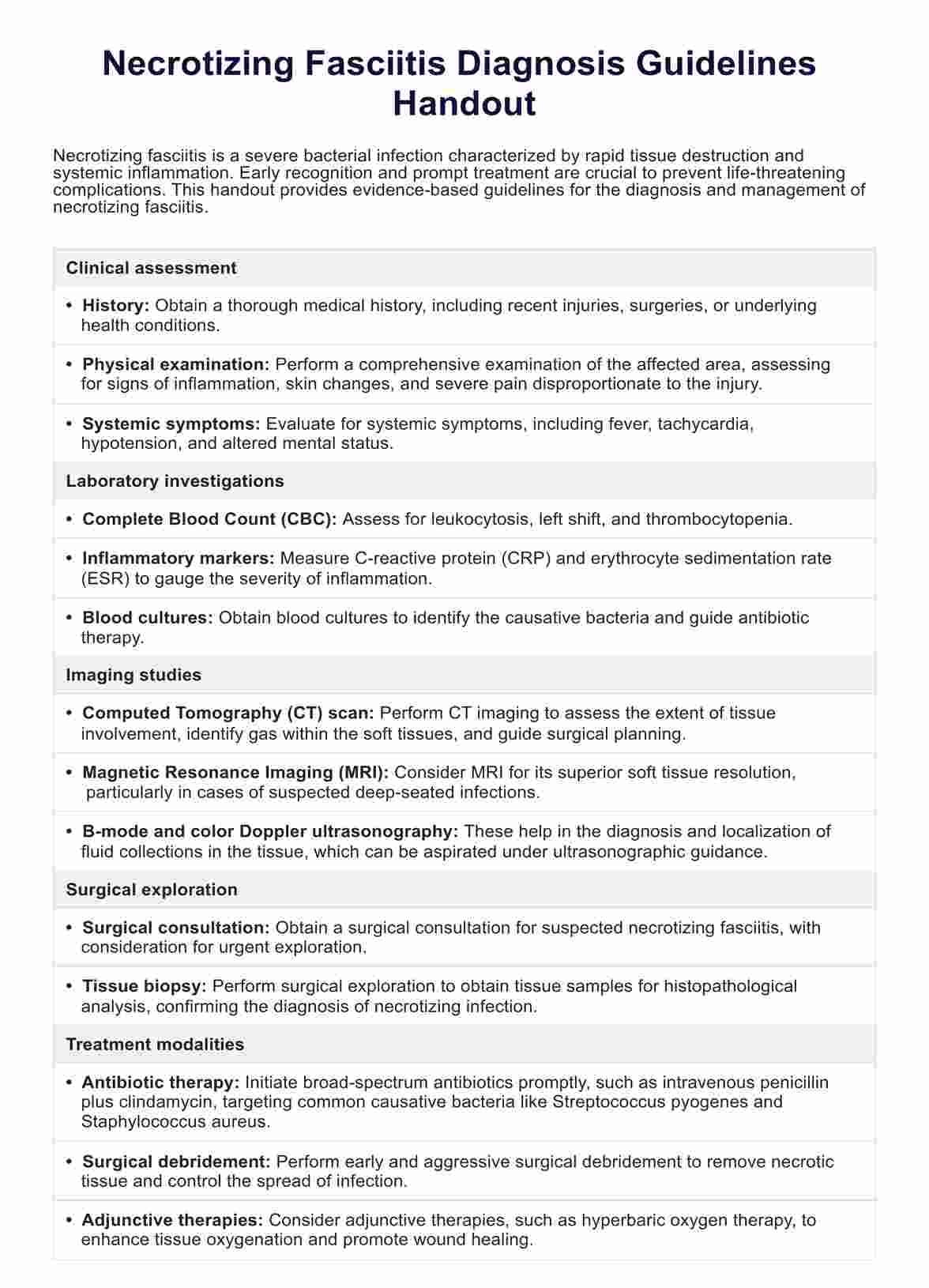
Diagnosing necrotizing fasciitis requires a comprehensive approach that involves clinical evaluation, imaging studies, laboratory tests, and, in some cases, surgical exploration. Below are the steps healthcare practitioners may follow to diagnose this condition:
Step 1: Clinical assessment
Healthcare practitioners begin by conducting a thorough physical examination of the patient, focusing on the affected area. They assess for common signs of necrotizing fasciitis, such as severe pain, swelling, redness, and skin changes. The presence of systemic symptoms like fever and malaise may also raise suspicion for the infection.
Step #2: Laboratory investigations
Laboratory tests are essential for confirming the diagnosis of necrotizing fasciitis. Blood tests, including complete blood count (CBC), inflammatory markers (such as C-reactive protein and erythrocyte sedimentation rate), and blood cultures, help identify signs of infection and determine the causative bacteria.
Step #3: Imaging studies
Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), play a crucial role in assessing the extent of tissue involvement and identifying areas of necrosis. These imaging modalities help healthcare practitioners visualize deep tissue structures and detect characteristic signs of necrotizing fasciitis, such as gas within the soft tissues.
Step 4: Surgical exploration
In cases where the diagnosis remains uncertain or urgent intervention is required, surgical exploration of the affected area may be necessary. Surgeons perform an incision and exploration to directly visualize the involved tissues, assess the extent of necrosis, and obtain tissue samples for further analysis.
Step 5: Tissue biopsy
A tissue biopsy may be performed during surgical exploration or as a separate procedure to confirm the presence of necrotizing fasciitis. Tissue samples are collected from the affected area and examined microscopically to identify characteristic histological features of necrotizing infection, such as necrosis of the fascia and surrounding tissues.
You can use the Clinical Evaluation Template to assess and document patient progress thoroughly. This template helps ensure a comprehensive understanding of each patient's condition, facilitating better diagnosis and treatment planning.
What is a Necrotizing Fasciitis Diagnosis Guidelines Handout?
A Necrotizing Fasciitis Diagnosis Guidelines Handout is a comprehensive document designed to provide healthcare practitioners with essential information and guidance for the diagnosis and management of necrotizing a soft tissue infection, specifically necrotizing fasciitis. This handout outlines evidence-based recommendations and best practices for identifying and treating this severe bacterial infection, which can lead to life-threatening complications if not promptly diagnosed and managed.
The guidelines cover various aspects of necrotizing fasciitis diagnosis, including clinical assessment, laboratory investigations, imaging studies, and surgical interventions. They emphasize the importance of early recognition of necrotizing infections and prompt initiation of appropriate treatment to prevent disease progression and improve patient outcomes.
In addition to diagnostic strategies, the handout may also include information on treatment modalities, such as antibiotic therapy, surgical debridement, and adjunctive therapies like hyperbaric oxygen therapy. It highlights the significance of a multidisciplinary approach involving infectious disease specialists, surgeons, and wound care experts in the management of severe soft tissue infections.
How to use our diagnosis guidelines handout template?
Necrotizing Fasciitis Diagnosis Guidelines Handout template is designed to assist medical practitioners in efficiently navigating the diagnostic process for necrotizing soft tissue infections, particularly necrotizing fasciitis caused by bacteria such as Streptococcus pyogenes.
Step 1: Familiarize yourself with the content
Start by reviewing the content of the handout template thoroughly. Familiarize yourself with the diagnostic criteria, recommended investigations, and treatment algorithms provided. Understanding the guidelines will help you utilize the handout effectively in clinical practice.
Step 2: Use as a reference tool
Utilize the handout template as a quick reference tool during patient evaluations. When assessing individuals with suspected severe necrotizing fasciitis or subcutaneous tissue infections, refer to the handout to ensure adherence to evidence-based diagnostic protocols and treatment recommendations.
Step 3: Customize for individual cases
Tailor the information provided in the handout template to suit the specific needs of each patient. Consider factors such as the patient's medical history, clinical presentation, and risk factors for necrotizing soft tissue infections when applying the diagnostic guidelines in practice.
Step 4: Educate patients and colleagues
Share the handout template with colleagues to promote consistent diagnostic approaches and enhance patient care. Additionally, use the information from the handout to educate patients and their families about the signs and symptoms of severe necrotizing fasciitis, emphasizing the importance of seeking medical attention promptly.
Step 5: Update regularly
Stay updated on advances in the field of infectious diseases and soft tissue infections. Periodically review and update the handout template to incorporate any new evidence-based practices or changes in diagnostic algorithms for necrotizing fasciitis.
Benefits of using this handout
Using our Necrotizing Fasciitis Diagnosis Guidelines Handout offers several advantages for healthcare practitioners in managing patients with necrotizing soft tissue infections, including streptococcal necrotizing fasciitis:
Accurate diagnosis
The handout provides a structured approach to evaluating patients with suspected necrotizing fasciitis, ensuring accurate diagnosis based on presenting symptoms, clinical assessment, and laboratory findings. This facilitates timely initiation of appropriate treatment, reducing the risk of complications and mortality associated with the condition.
Comprehensive guidance
Our handout offers comprehensive guidance on the diagnostic process, covering clinical assessment, laboratory investigations, imaging studies, and treatment modalities. It serves as a valuable reference tool, helping healthcare practitioners navigate the complexities of managing severe necrotizing soft tissue infections caused by streptococcal bacteria.
Early recognition of symptoms
By familiarizing themselves with the early symptoms and signs of necrotizing fasciitis outlined in the handout, healthcare practitioners can promptly identify patients at risk of developing severe complications. Early recognition allows for timely intervention and may prevent the progression of the infection to life-threatening stages.
Multidisciplinary collaboration
The handout promotes multidisciplinary collaboration among healthcare professionals involved in the care of patients with necrotizing fasciitis, including infectious disease specialists, plastic surgeons, and wound care experts. This collaborative approach ensures comprehensive management and optimal outcomes for patients affected by this flesh-eating bacterial infection.
Enhanced patient education
Healthcare practitioners can use the handout to educate patients and their families about the signs and symptoms of necrotizing fasciitis, emphasizing the importance of seeking medical attention promptly. Patient education plays a crucial role in facilitating early diagnosis and intervention, ultimately improving patient outcomes and reducing morbidity associated with the condition.
Commonly asked questions
Necrotising fasciitis is diagnosed through clinical assessment, laboratory tests, imaging studies, and, in some cases, surgical exploration to confirm tissue necrosis and identify causative bacteria.
The odds of surviving necrotizing fasciitis depend on various factors, including the promptness of treatment initiation, the extent of tissue involvement, and the presence of underlying health conditions. Mortality rates can range from 20% to 80%.
If left untreated, necrotizing fasciitis can rapidly progress, causing extensive tissue destruction, systemic infection, septic shock, and death. Early intervention is crucial to prevent life-threatening complications.