Medical Prior Authorization Form
Learn the importance of prior authorization for your patients. Download a free Medical Prior Authorization Form to simply insurance requests.


Understanding medical prior authorization
Medical prior authorization is a process wherein healthcare providers must submit a request to a patient's insurance company before performing certain procedures, administering specific medications, or sending patients to specialists outside of the primary care network.
This crucial step ensures that the requested service or medication is covered under the patient's health plan and is deemed medically necessary. Often, detailed information about the patient's condition and the rationale for the suggested treatment or medication must be provided, making the accuracy and thoroughness of the submitted documentation paramount.
Prior authorizations help manage costs and ensure patients receive appropriate care coverage, though they can also place additional administrative burdens on the healthcare provider and pharmacy within the network.
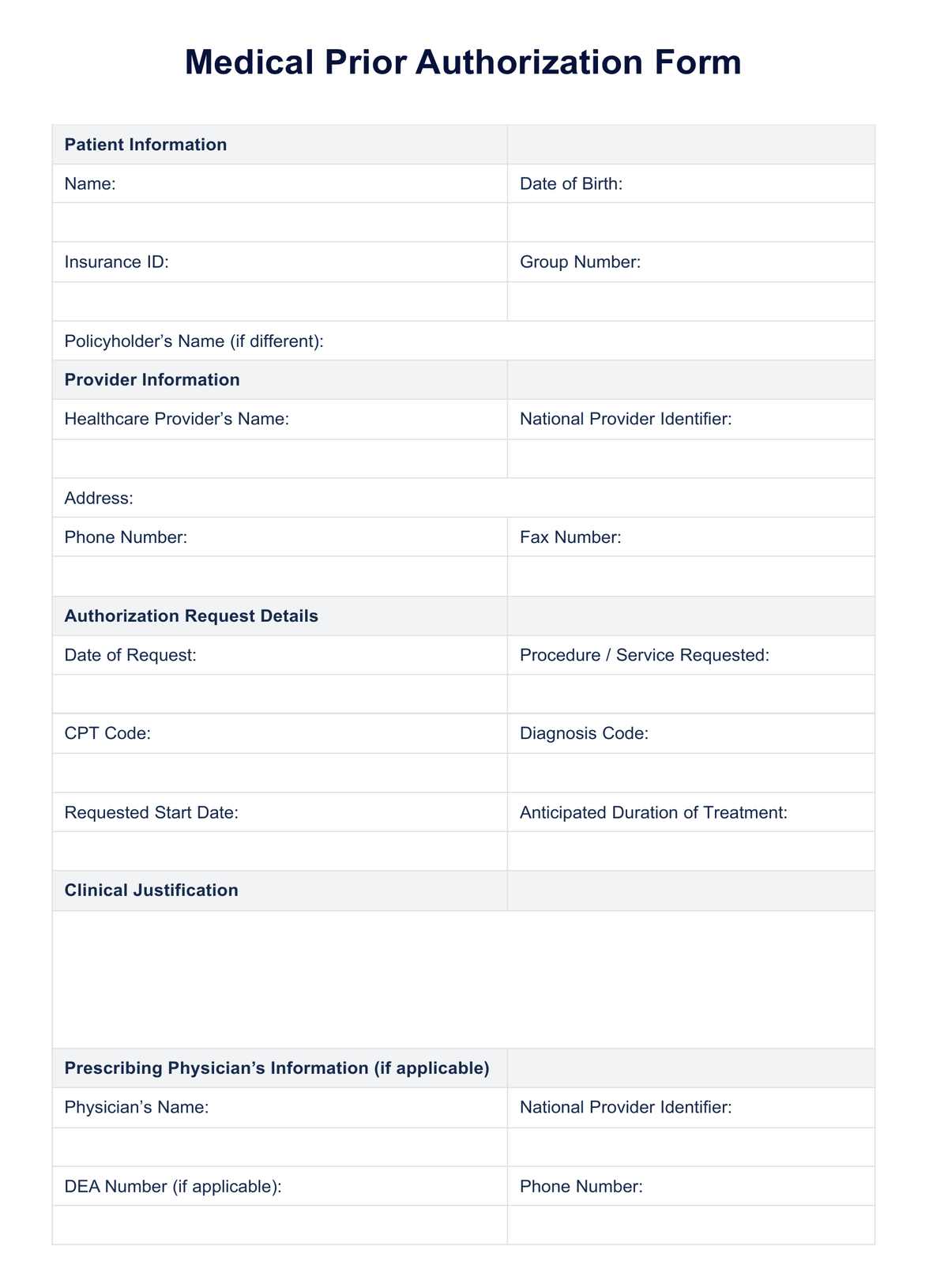
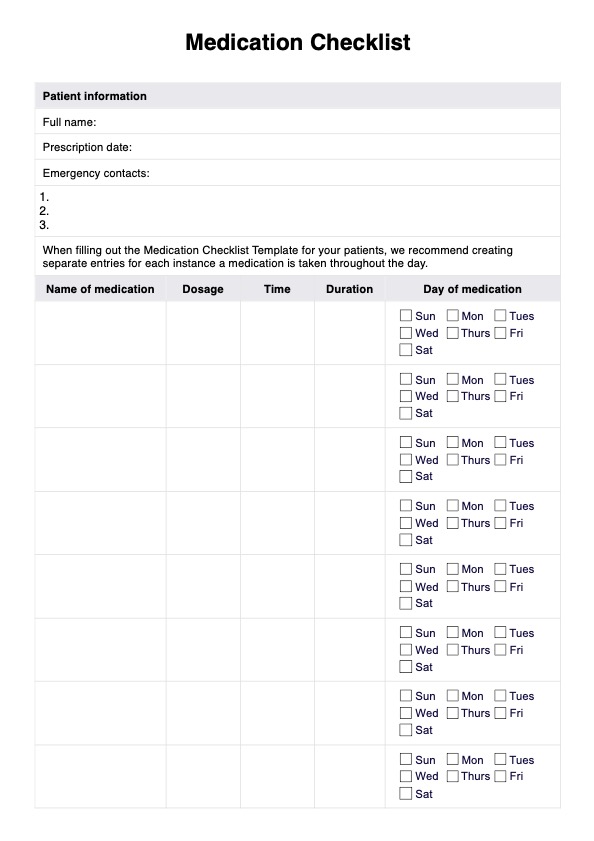
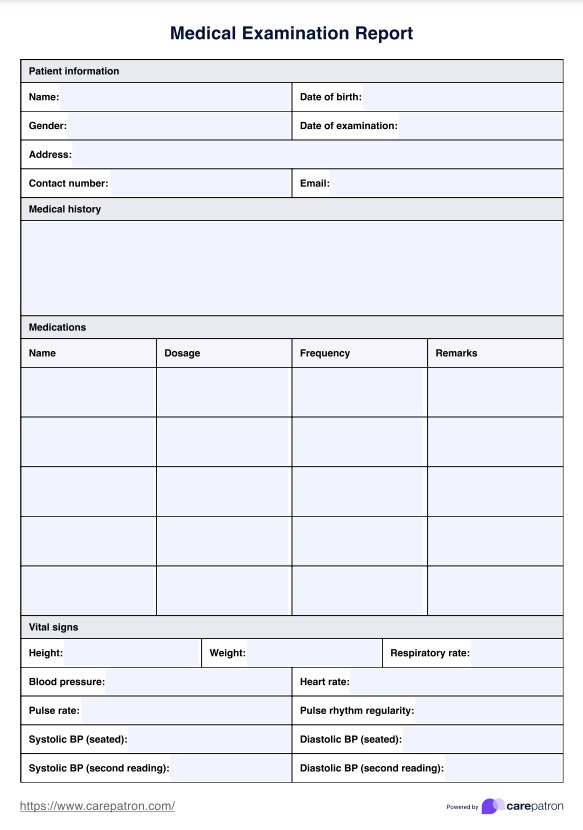
Medical Prior Authorization Form Template
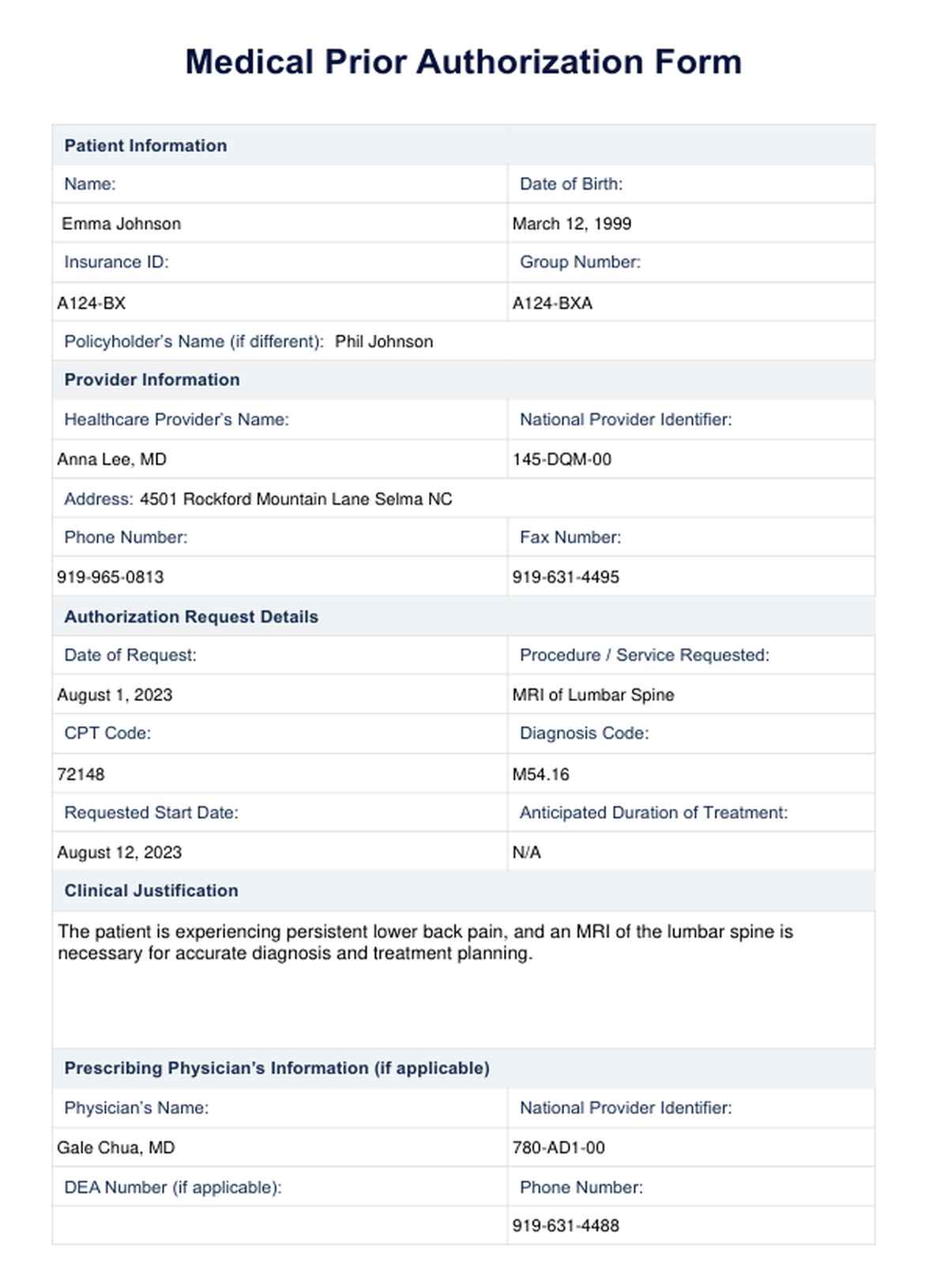
Medical Prior Authorization Form Example
Types of services requiring prior authorizations
The specific services and medications that require prior authorization can vary greatly depending on the patient's insurance plan. Some common examples include:
Surgeries (both elective and non-elective procedures)
These medical procedures could vary significantly, starting from routine tasks like mole removal to intricate surgeries such as joint replacements, which require specialized expertise and meticulous care.
Specialized medications and treatments
Certain expensive or high-risk medications, such as chemotherapy drugs or biological agents for autoimmune disorders, may require prior authorization. Moreover, some treatments, including physical therapy and home health services, may also need this step.
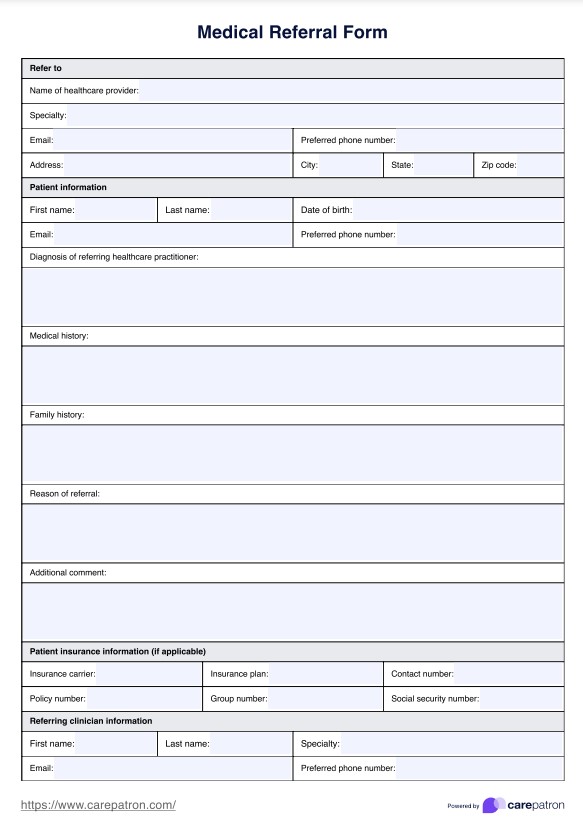
Out-of-network referrals
If a patient needs to see a specialist outside of the primary care network or receive treatment at an out-of-network facility, the healthcare provider must obtain prior authorization from the insurance company. This ensures that the patient's health plan covers the costs associated with these services.
Home healthcare services
In some cases, patients may require skilled nursing care or other medical services at home. The patient's insurance plan may cover these services, but prior authorization is typically required to ensure that they meet the criteria for coverage.
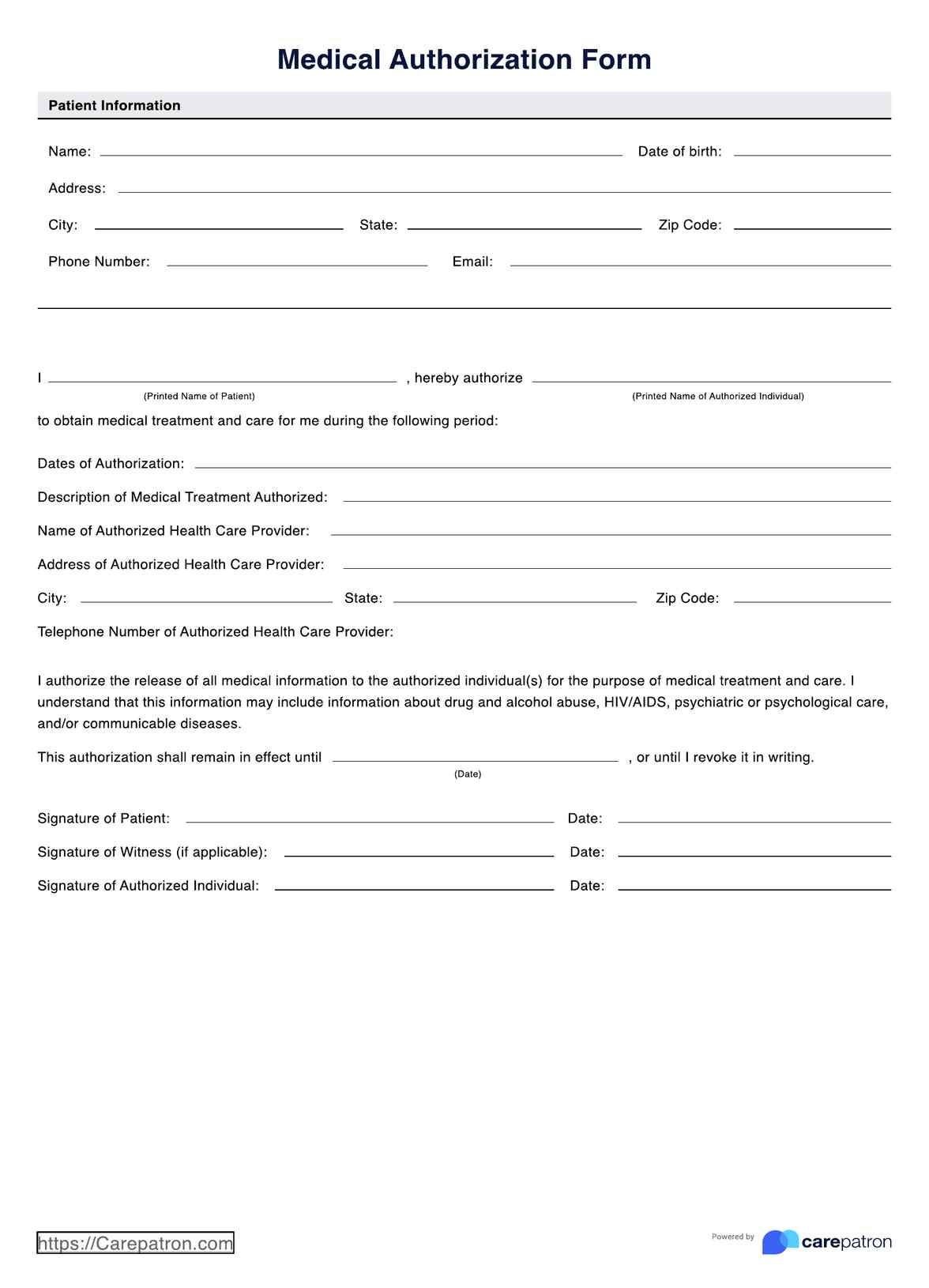
What is a Medical Prior Authorization Form?
Healthcare professionals use a Medical Prior Authorization Form to request a prior authorization from an insurance company. This form typically includes information such as the patient's personal details, relevant medical history, and specific treatment or medication being requested. It may also require additional supporting documents, such as lab results or imaging scans, to provide further justification for the requested service.
This form serves as a communication tool between healthcare providers and insurance companies, ensuring that all necessary information is provided in a standardized format for review. It also helps to streamline the process for both parties and reduces the chances of errors or missing information.
How to use our free Medical Prior Authorization Form template
Carepatron has created a free prior authorization form to ensure your patients get medical insurance coverage for necessary treatments or medications. To use our template, follow these steps:
Step 1: Access the form
Get a copy of the Medical Prior Authorization Form using the link on this page. It's also available via the Carepatron app or our templates library.
Step 2: Use the print or digital copy
Pick the form type that works best for you - print or digital copy. You can edit and fill out both versions electronically.
Step 3: Fill in the details
Complete the form with all necessary information, including patient details, provider information, and treatment/medication details.
Step 4: Attach supporting documents
Attach any relevant documents such as lab results or imaging scans to provide further justification for your request.
Step 5: Submit to insurance company
Submit the completed form and supporting documents to the appropriate insurance company for review. Ensure that all information is accurate and legible to avoid any delays in the approval process.
When is prior authorization needed?
Prior authorization is often required for certain treatments or medications that insurance companies may deem not medically necessary. This process helps ensure that patients receive the most appropriate and cost-effective care while also protecting insurance companies from unnecessary expenses.
Some common reasons for prior authorization include:
- Prescription drugs that are not on an insurance company's preferred drug list
- High-cost procedures or treatments
- Experimental or investigational treatments
- Certain medical equipment or devices
- Out-of-network providers or facilities
- Specific chronic conditions that require ongoing treatment
It's important to check with your insurance company beforehand to determine if prior authorization is needed for a particular treatment or medication.
Benefits of our free Medical Prior Authorization Form
Our printable Medical Prior Authorization Form template can help streamline the process of obtaining prior authorization for treatments or medications. Here are some of its other benefits:
Fully digital and customizable
Our form is available in a printable PDF format that can be easily filled out electronically or printed for handwritten completion. It can also be customized to include your practice's logo and contact information, making it look more professional and official.
Comprehensive and organized
You can record all the necessary patient and provider information in one place, including diagnosis codes, treatment details, and insurance information. This makes it easier for insurance companies to process the request quickly and efficiently.
Easy to use
Our form is designed to be user-friendly and easy to understand, with clear fields and instructions. This can save you time and frustration when filling it out, especially if you need multiple authorizations for different treatments or medications.
Commonly asked questions
A medical prior authorization is an approval process required by insurance companies before they will cover certain healthcare services or treatments. This helps ensure that the prescribed treatment is necessary and appropriate for the patient's condition.
Insurance companies require prior authorizations to control costs and prevent unnecessary or inappropriate healthcare services from being covered.
Common services that require prior authorization include surgeries, certain medications, diagnostic tests, and medical equipment such as wheelchairs or CPAP machines. Additionally, insurance companies may also require prior authorization for out-of-network providers or specialized treatments.
Yes, you can modify the Medical Prior Authorization Form for your practice. Carepatron's software allows you to customize forms and templates based on the specific needs of your practice. This feature helps save time and streamline the authorization process for both patients and providers.