SOAP Notes for Therapy Template
SOAP notes are the best way for therapists to capture clients' mental health. With this template, you can effectively streamline notes and achieve higher clinical outcomes.


What are SOAP Notes for Therapy Template?
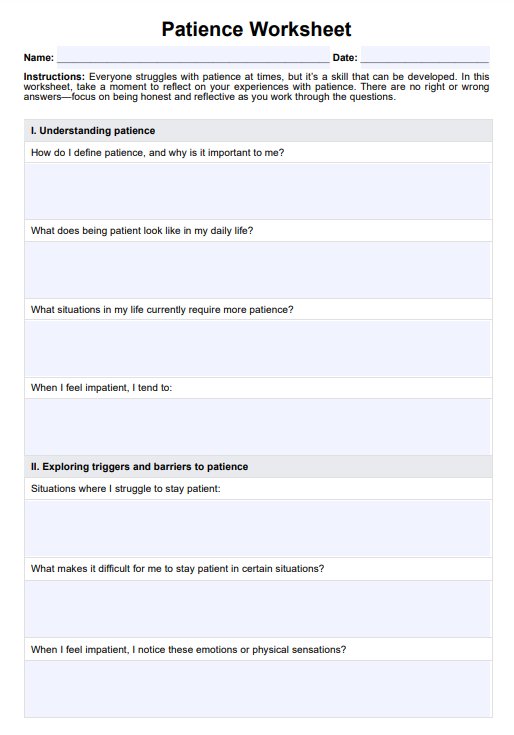
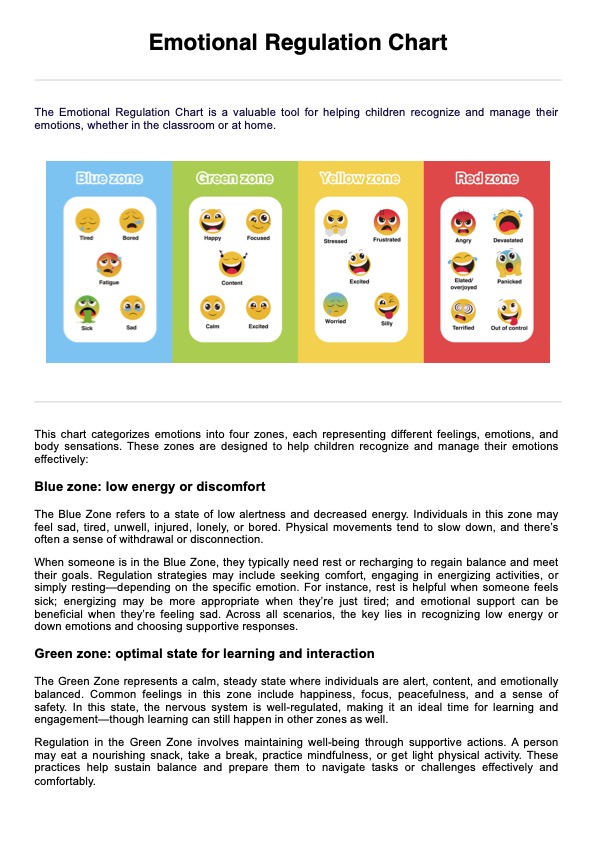
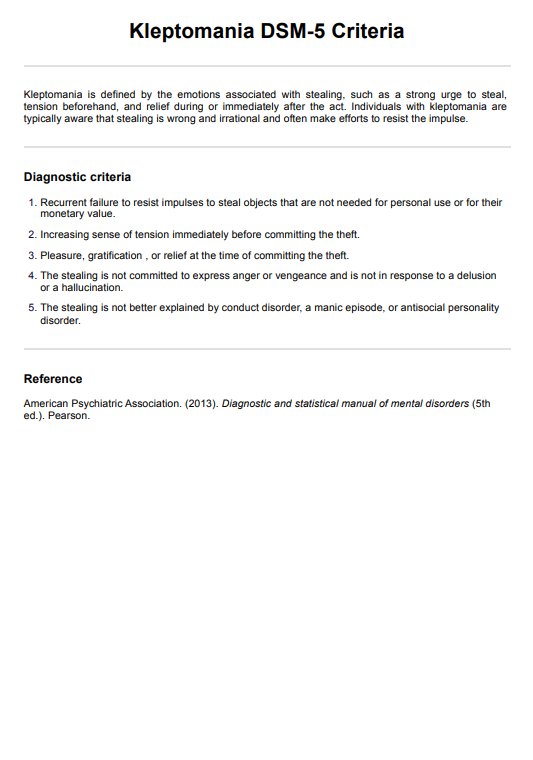
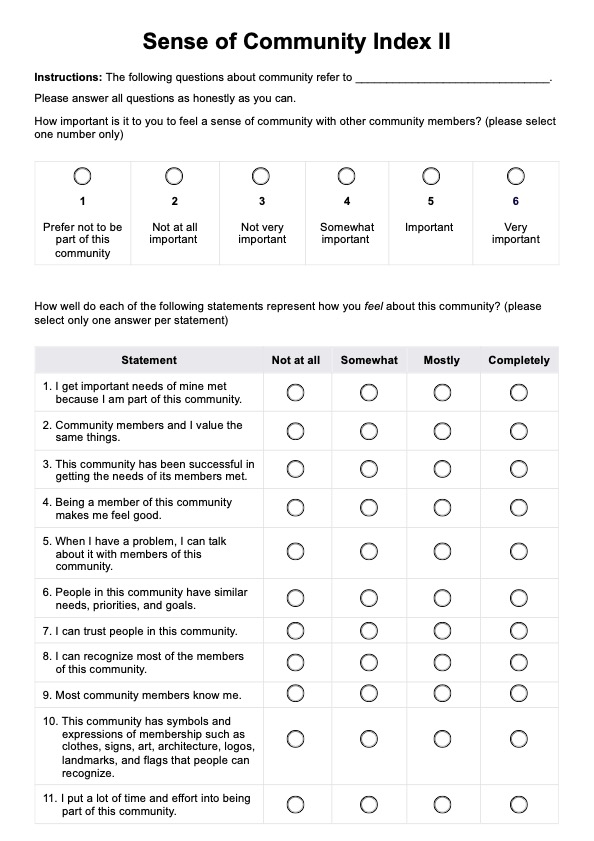
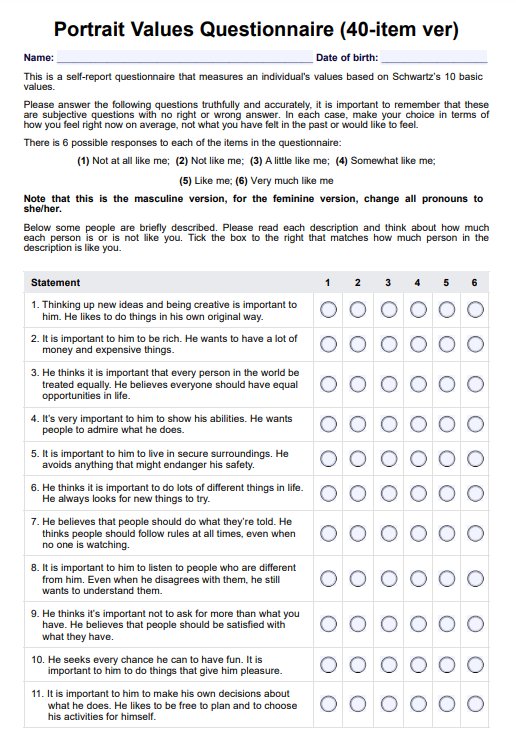
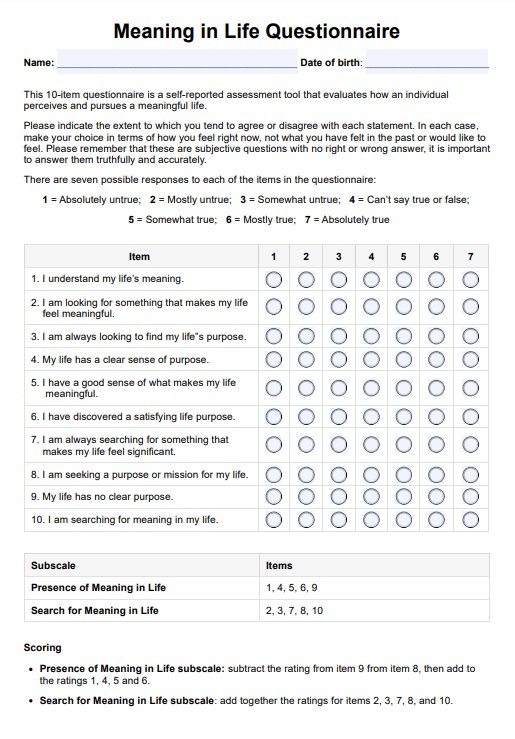
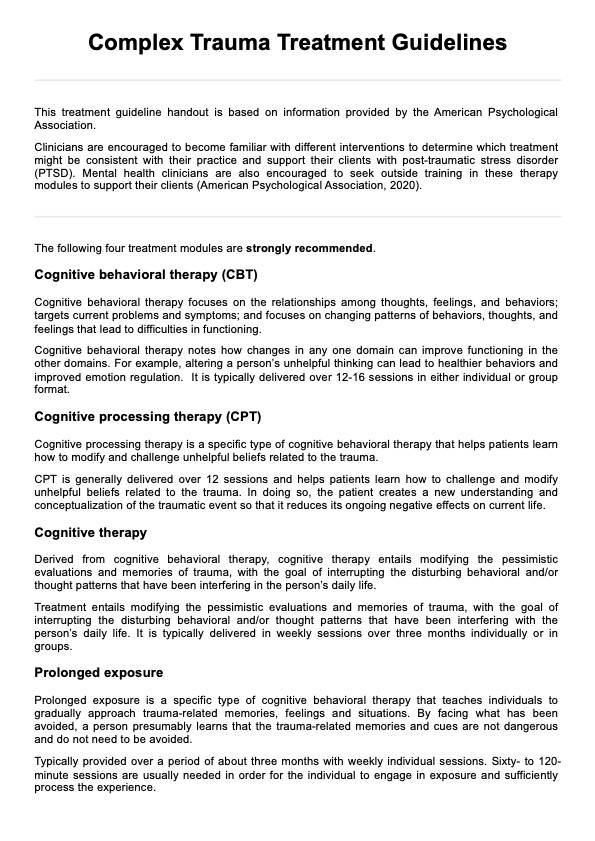
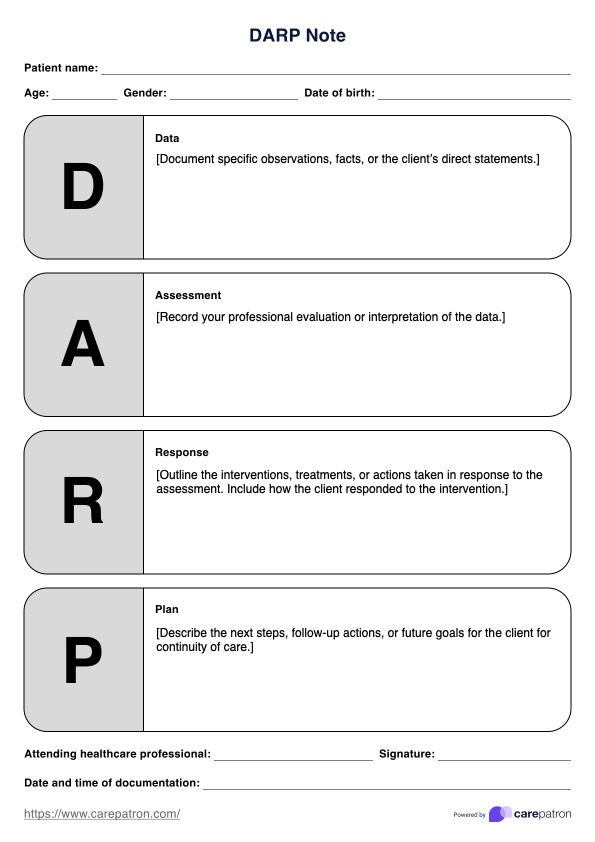
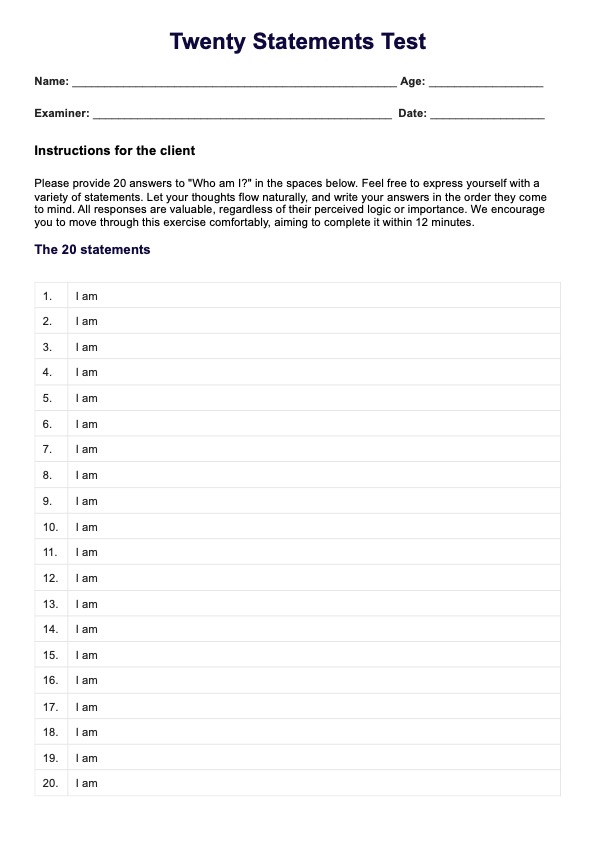
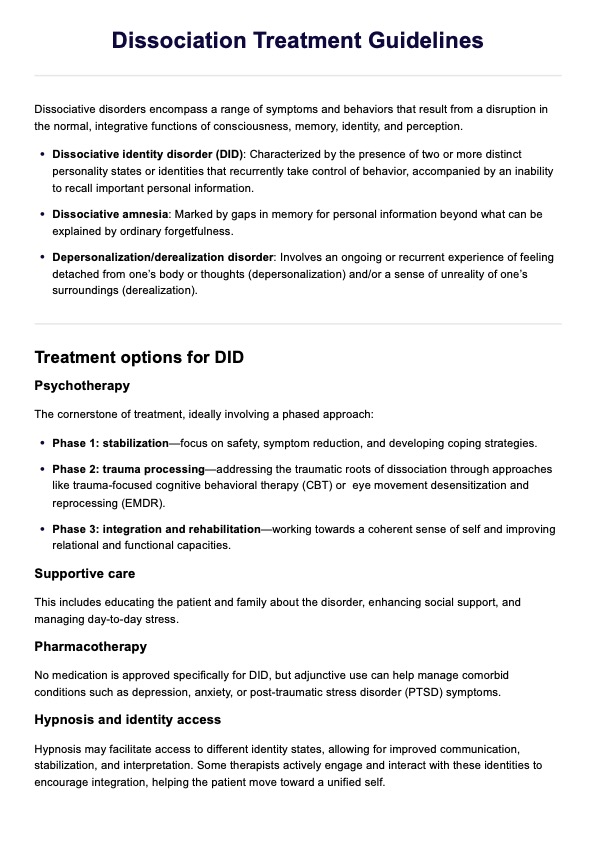
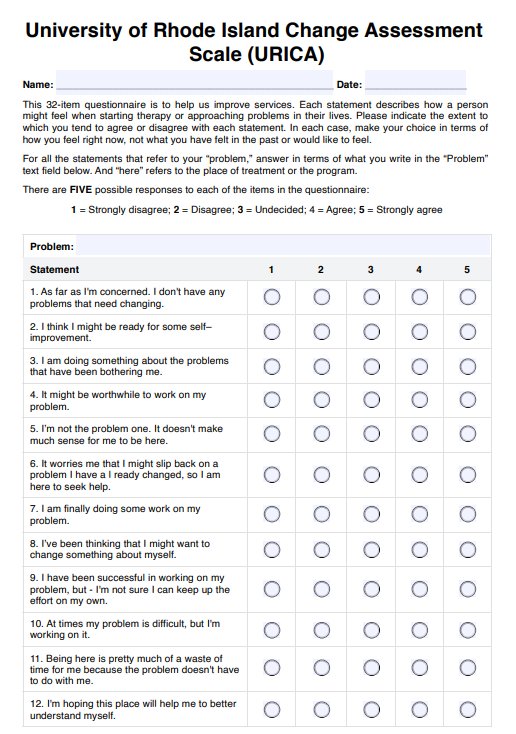
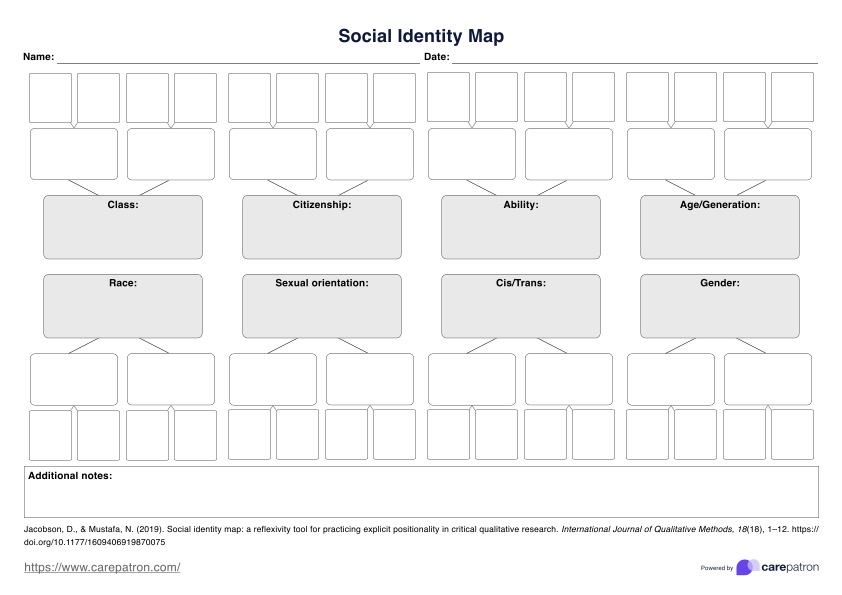
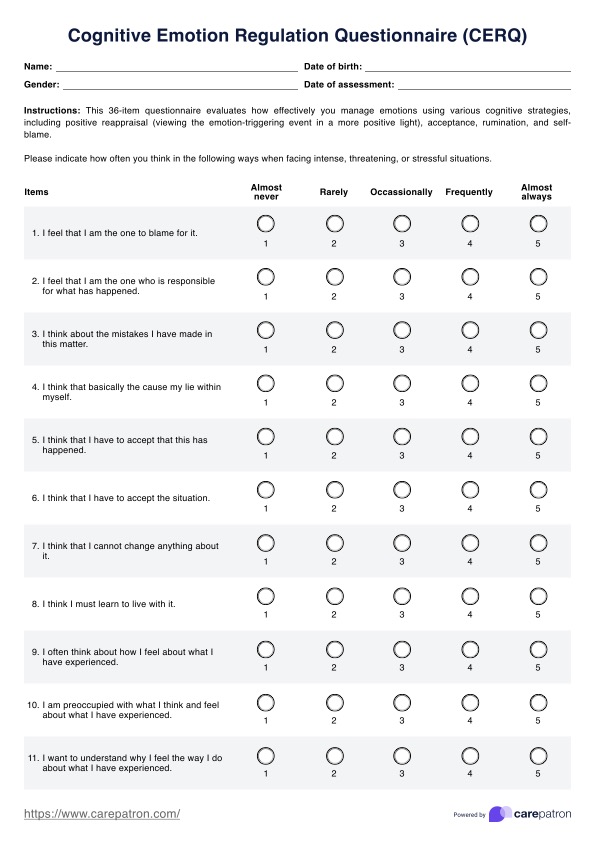
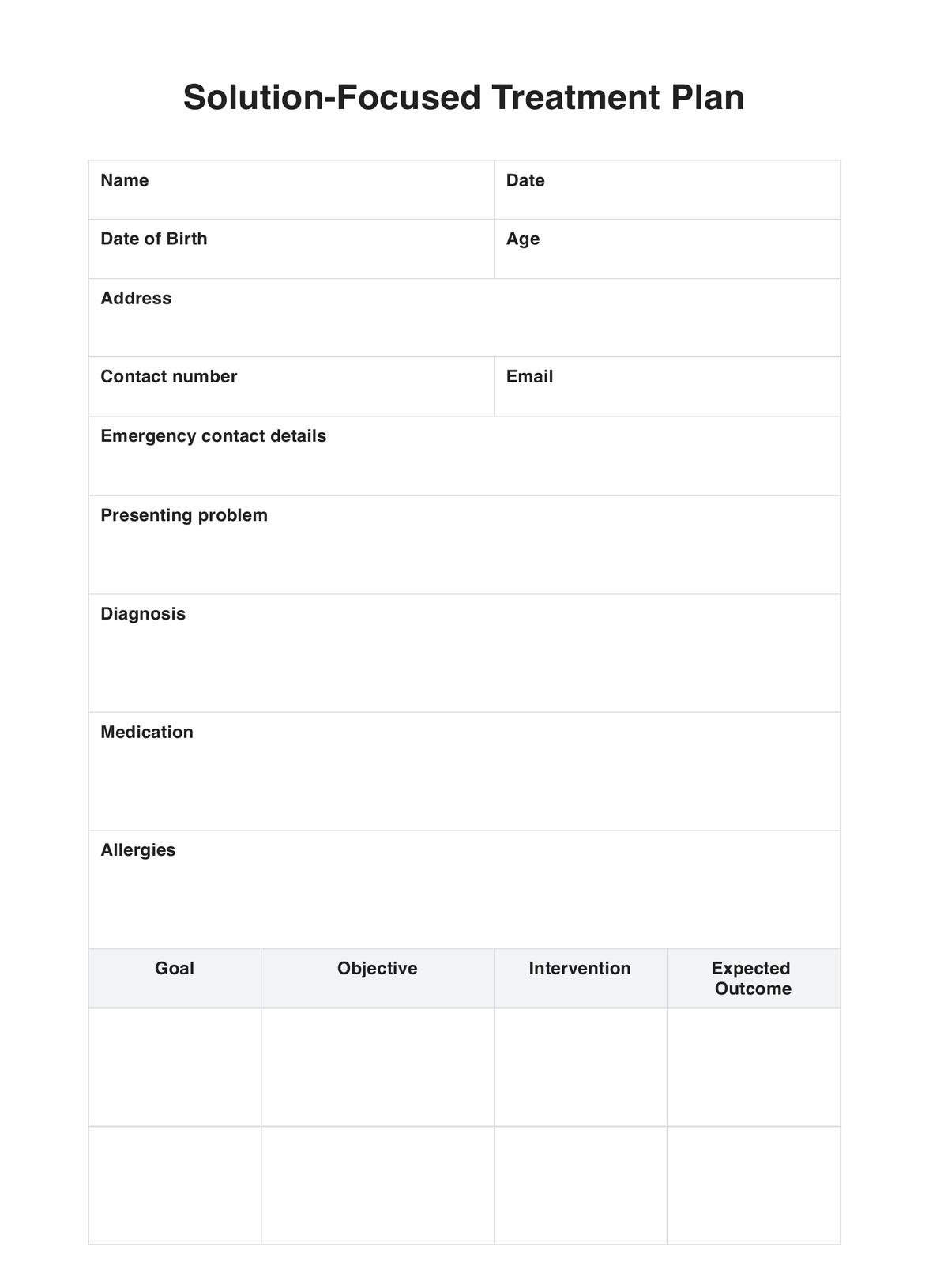
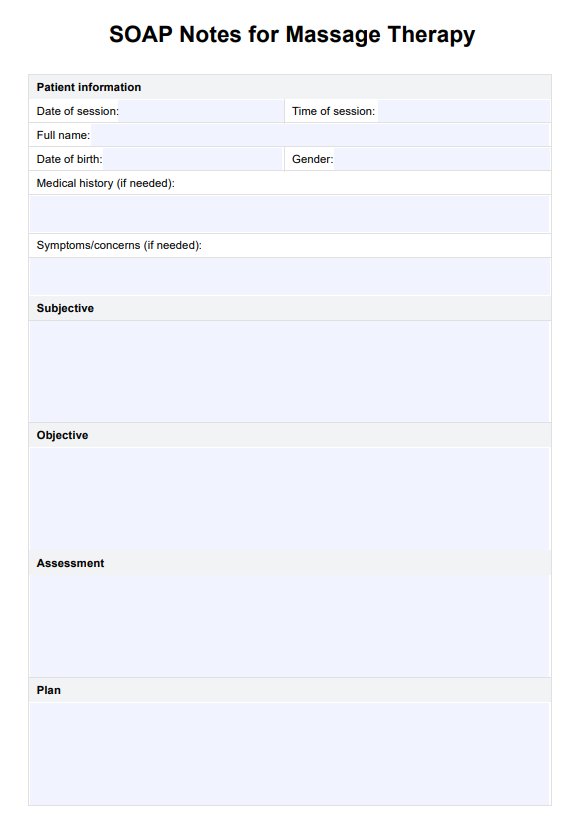
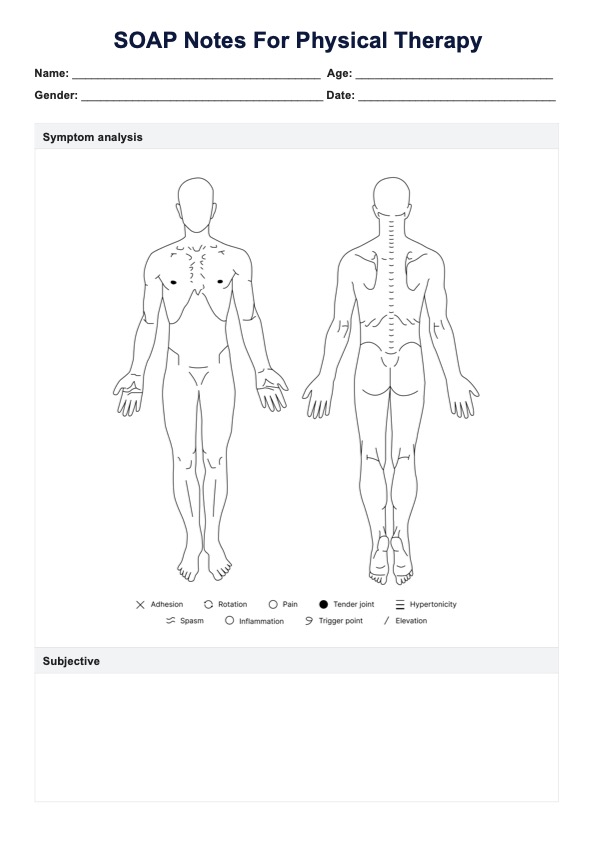
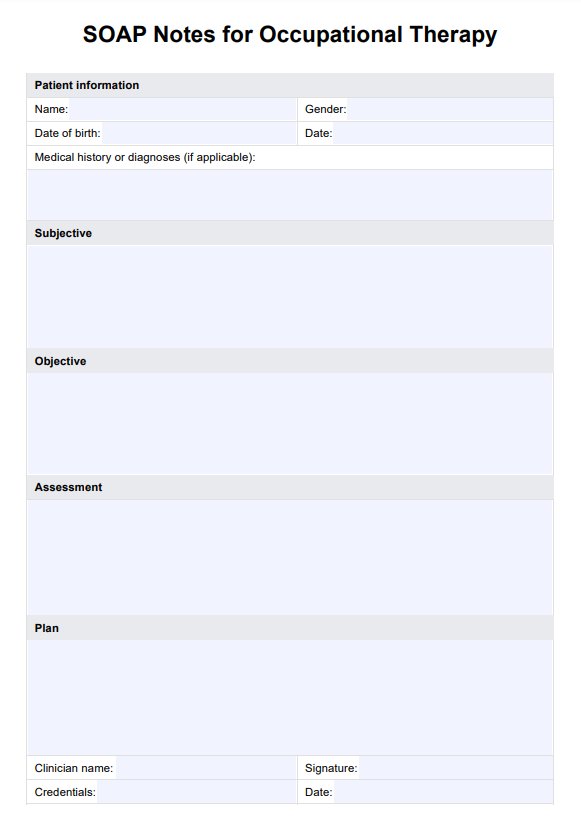
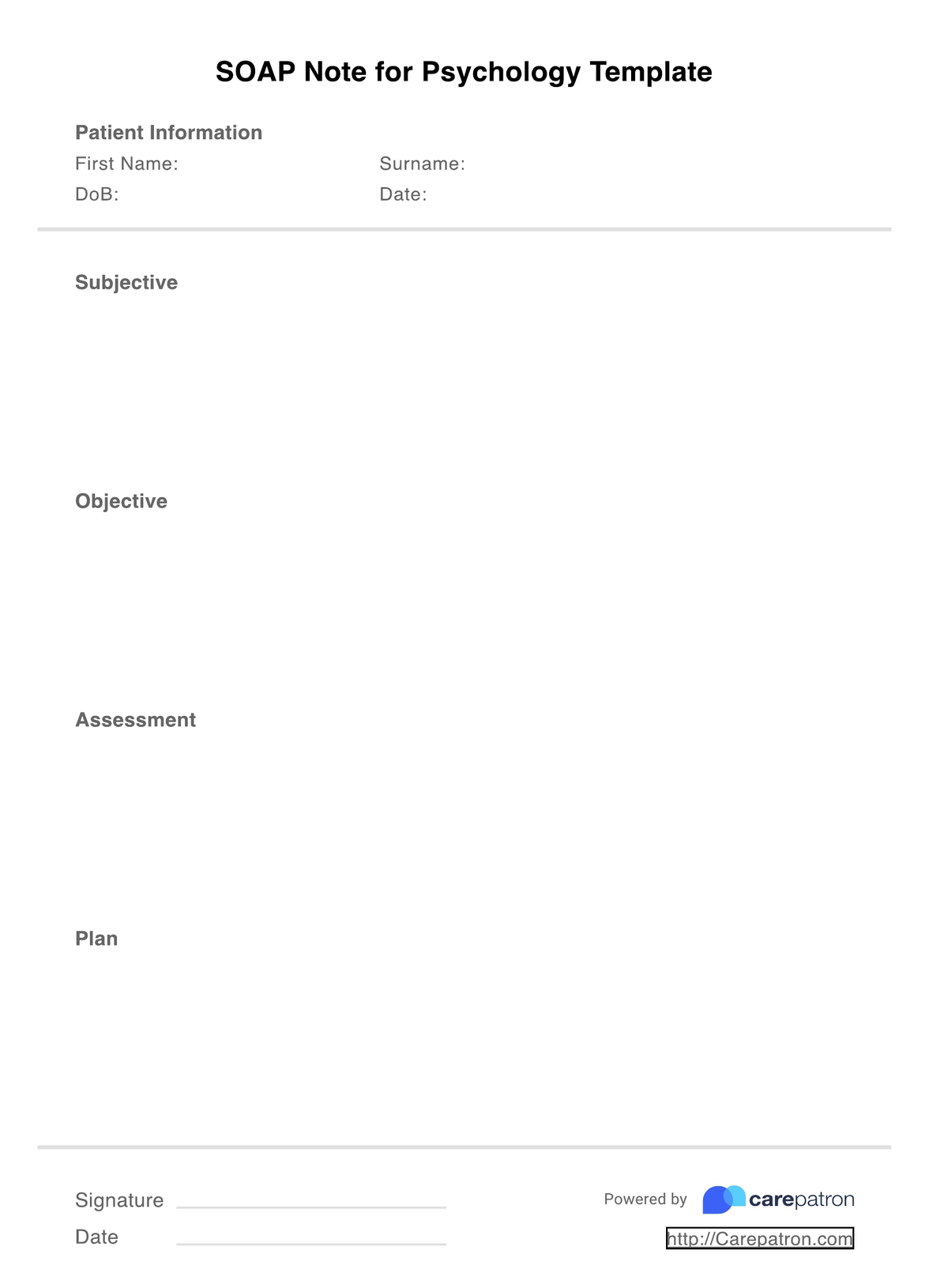
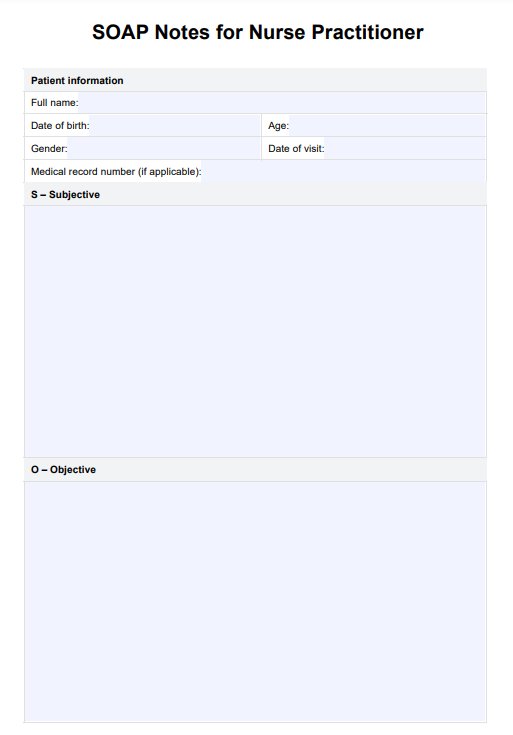
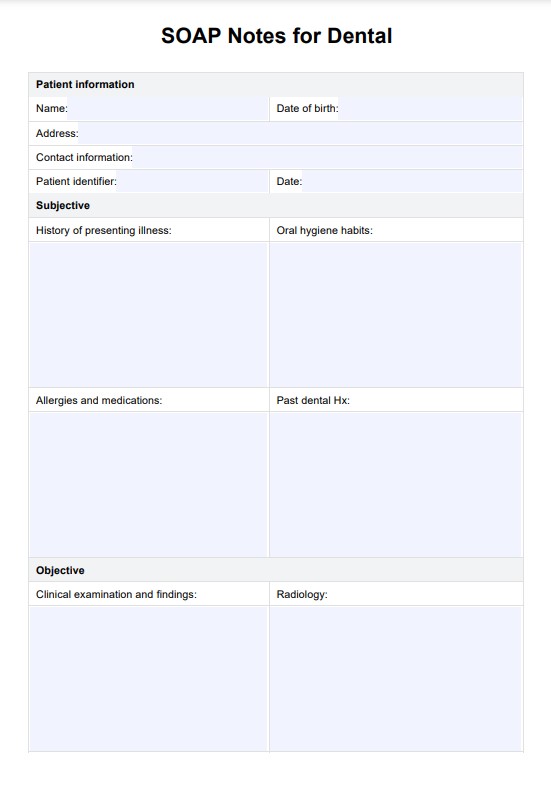
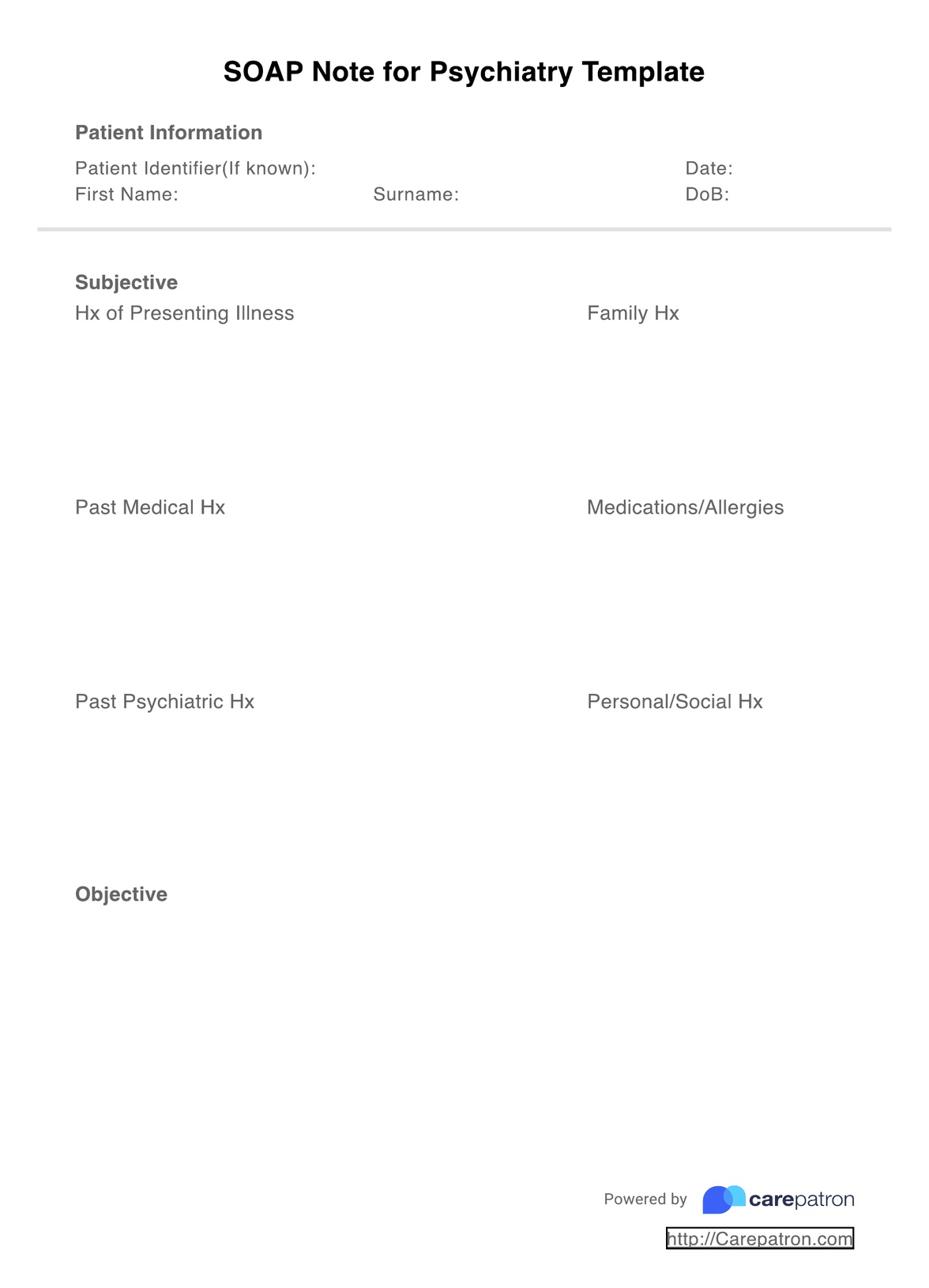
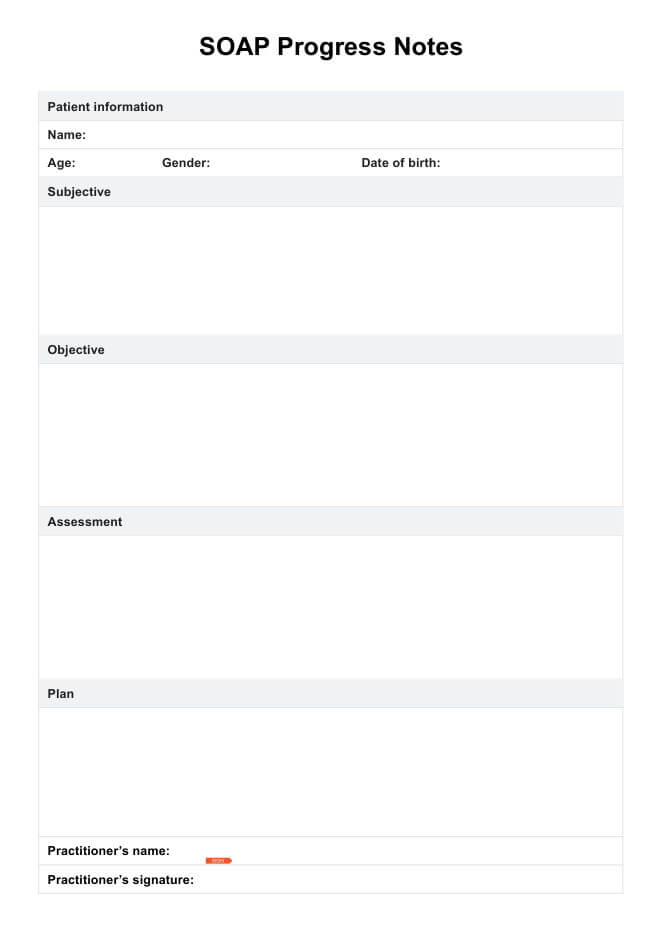
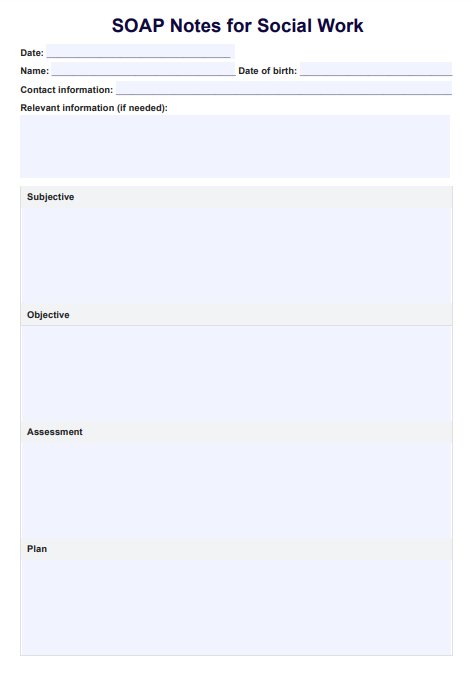
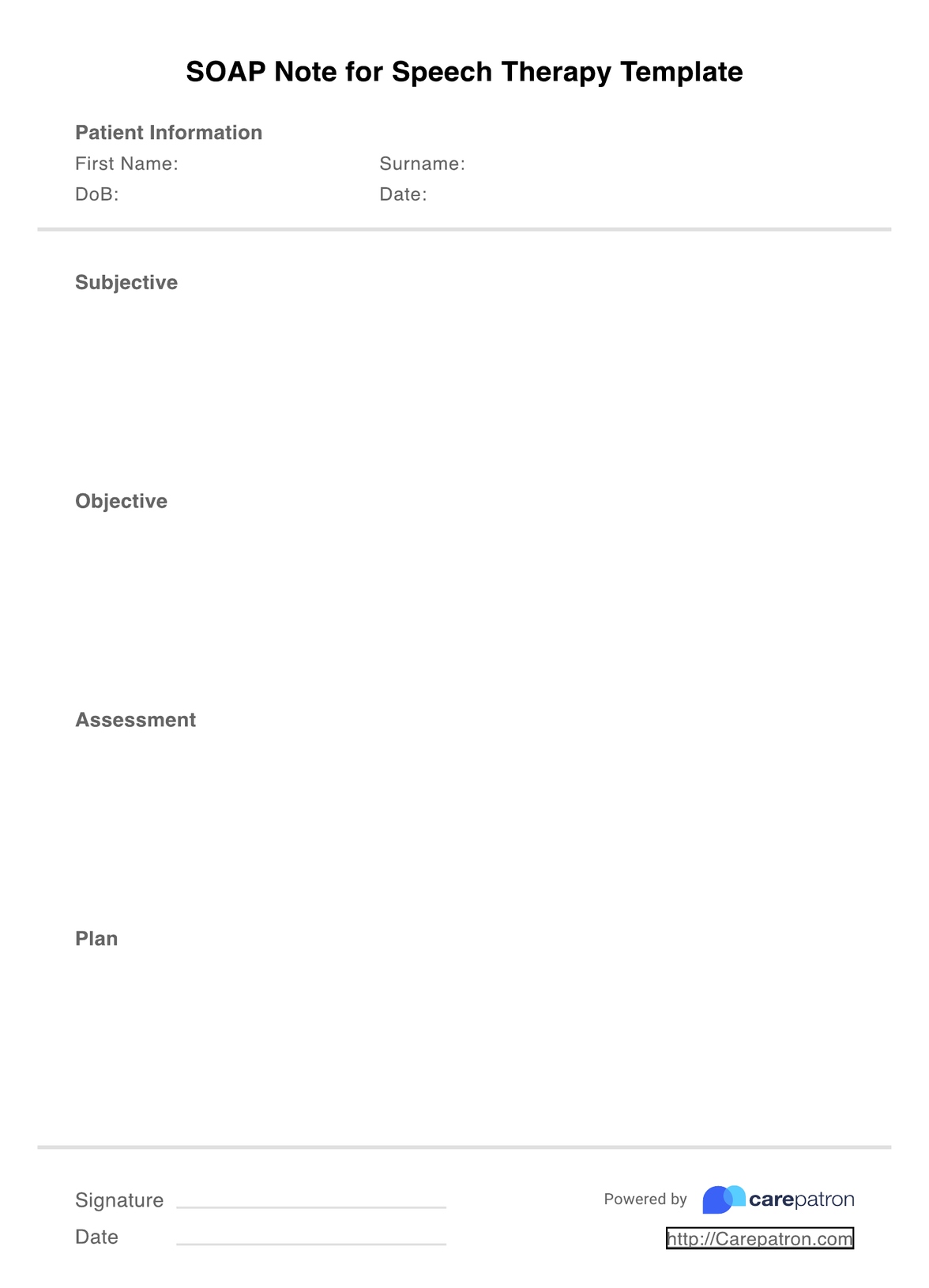
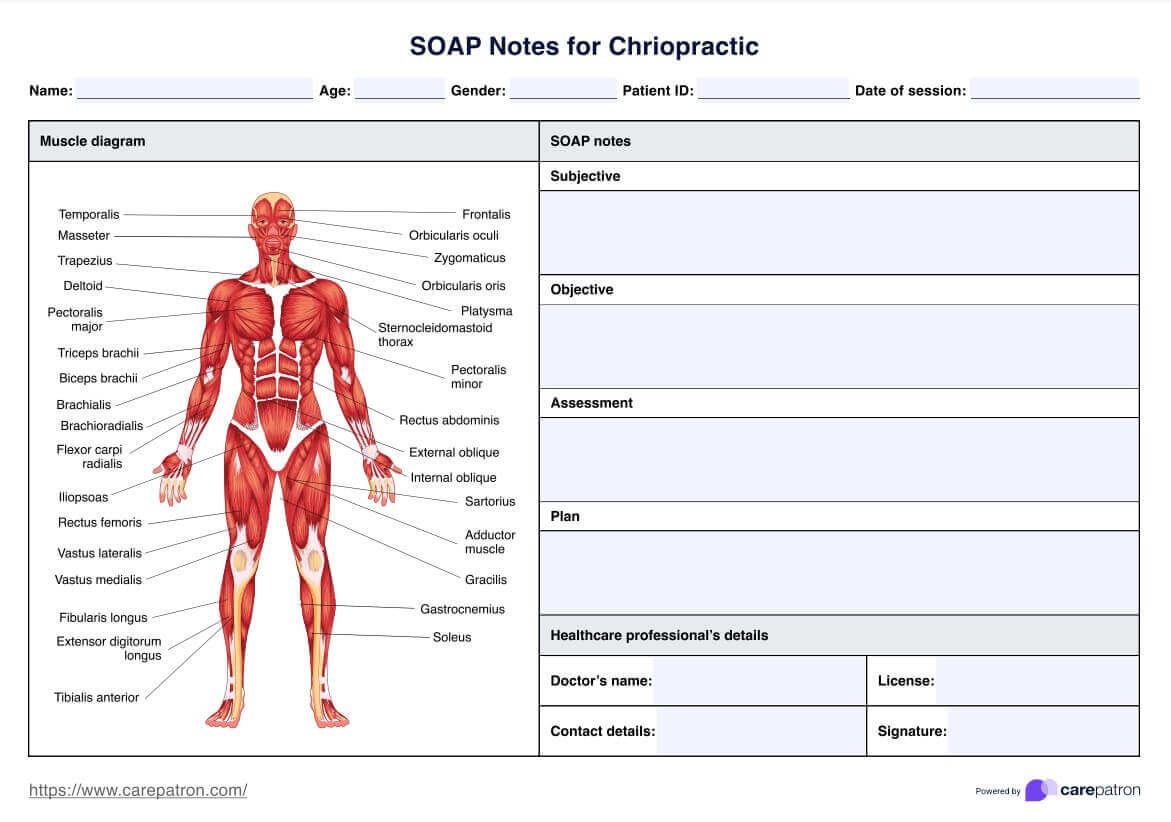
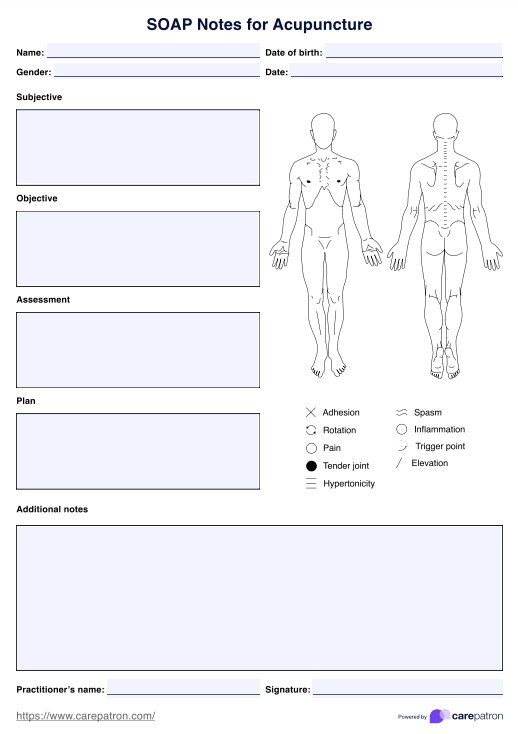
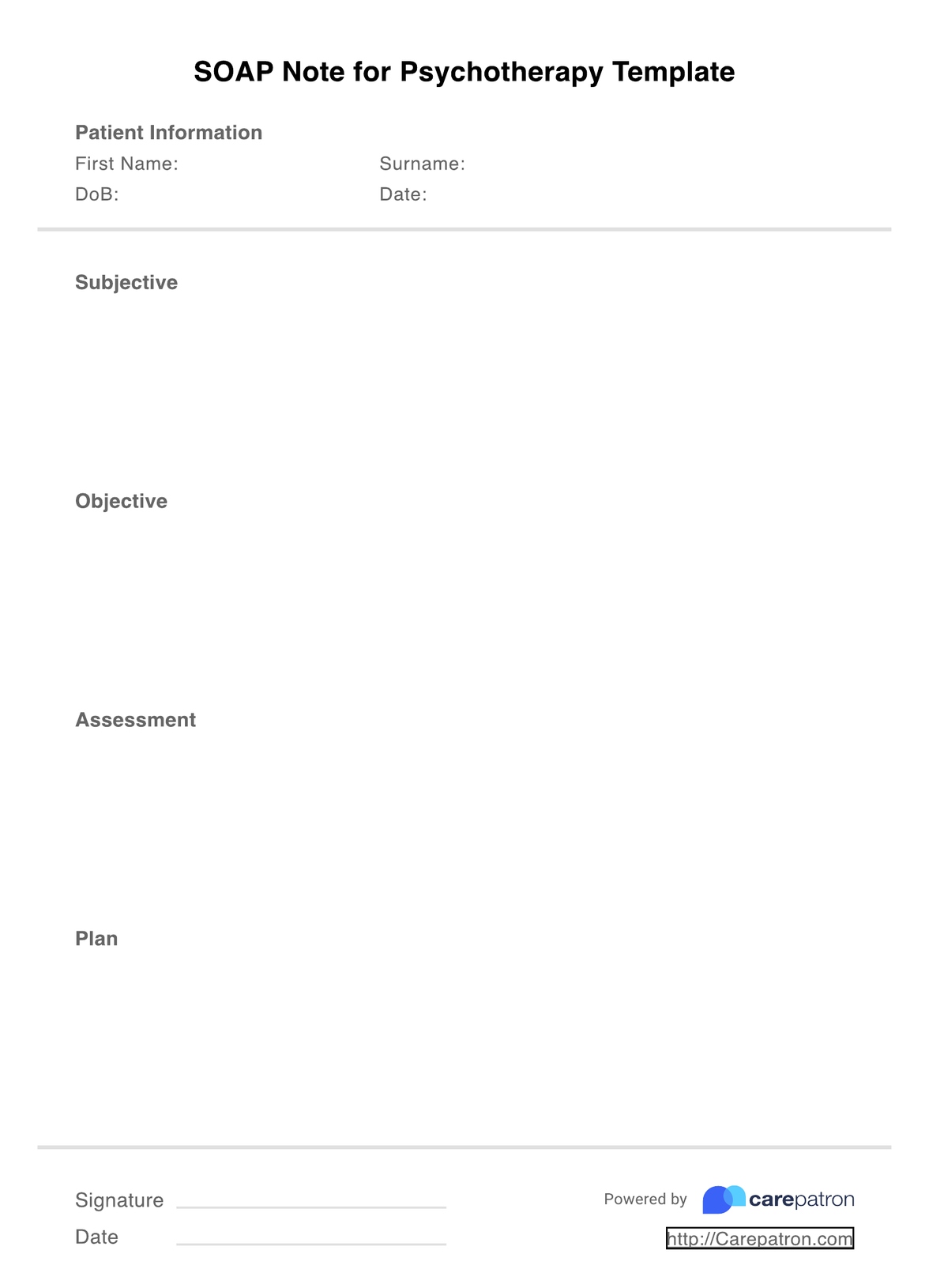
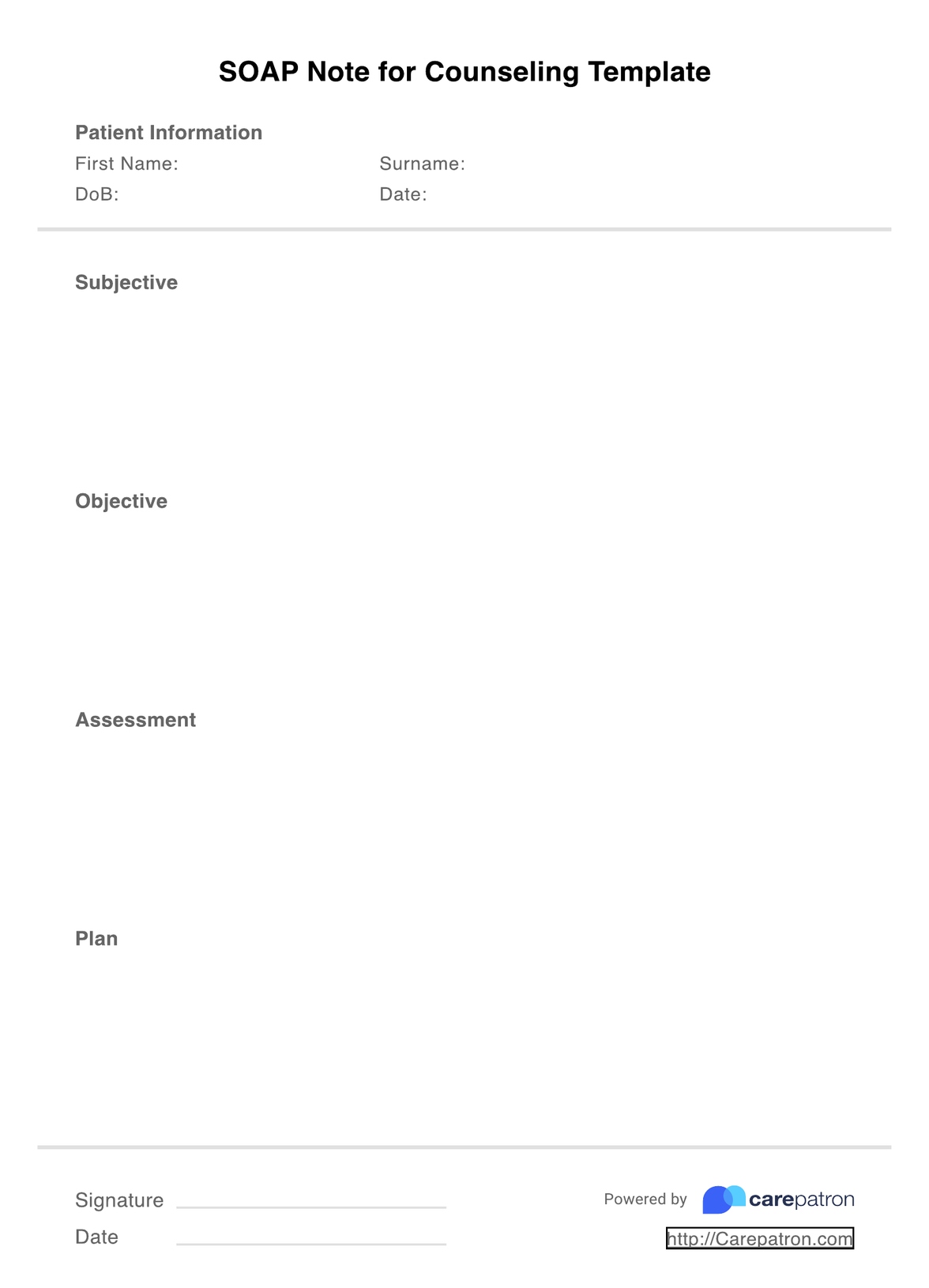
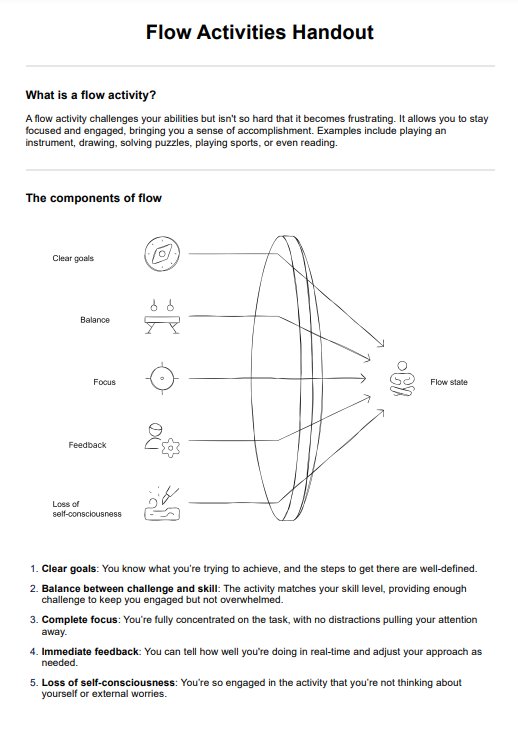
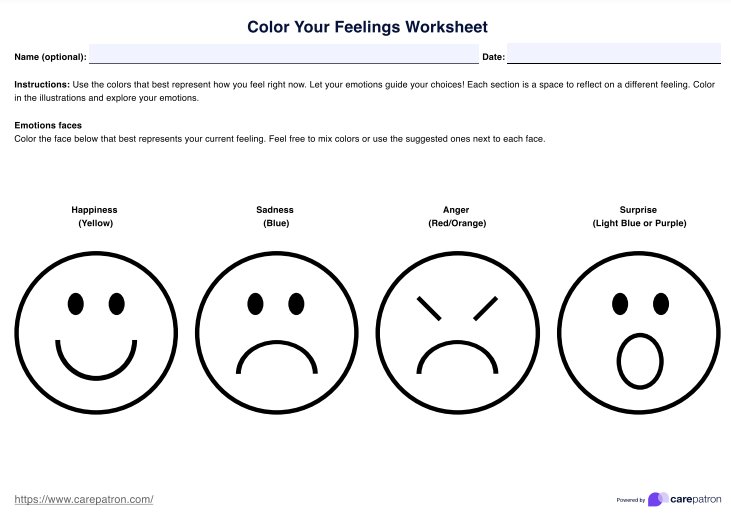
Therapy SOAP notes are one of the most common clinical documentation formats, as they capture rich clinical information and contribute to more informed treatment plans. Following a SOAP note for therapy example ensures that you get it right every time, and integrating our embedded template guarantees higher accuracy regarding your client. Writing SOAP notes covers four essential sections, which include the following:
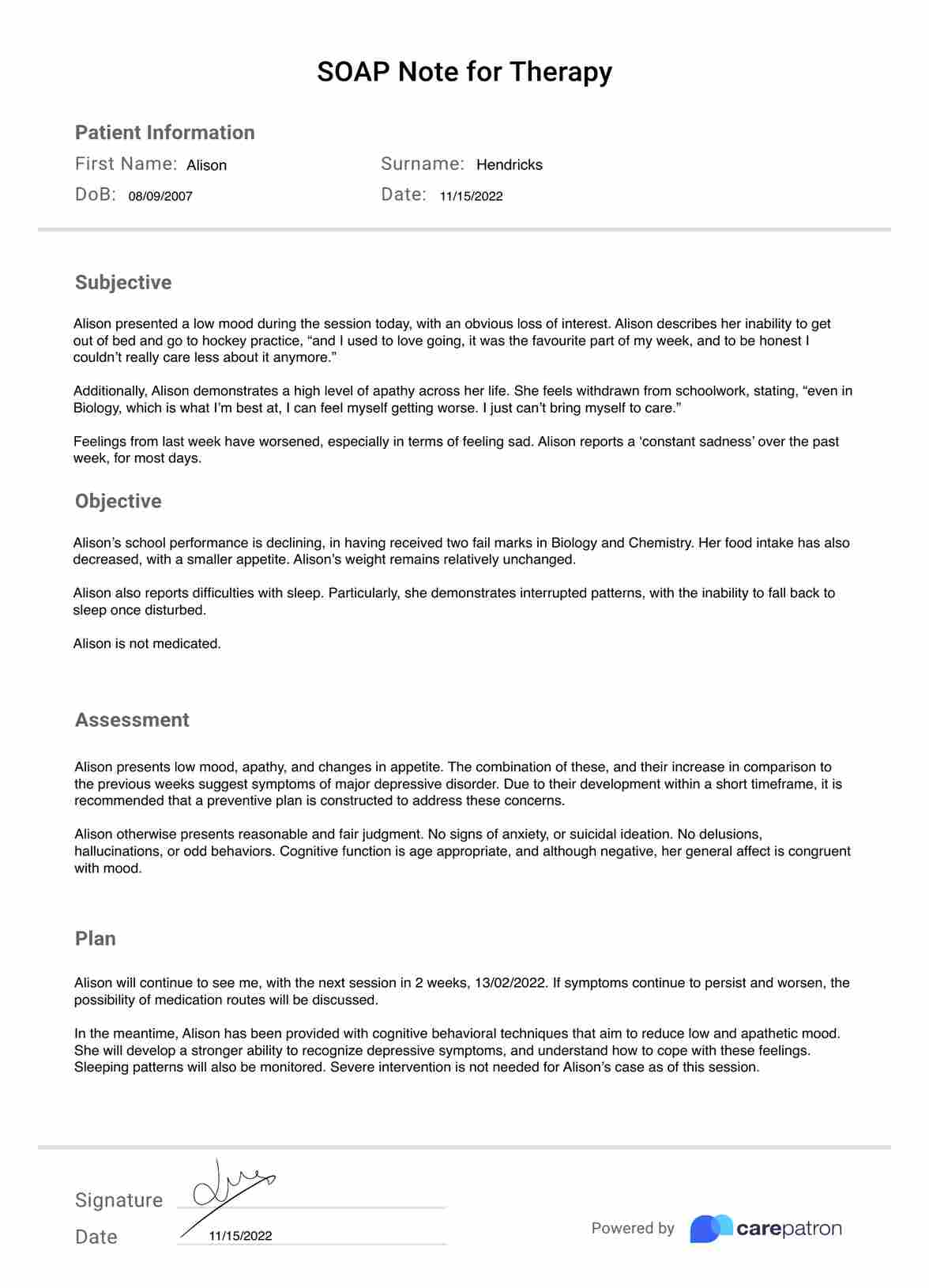
Subjective
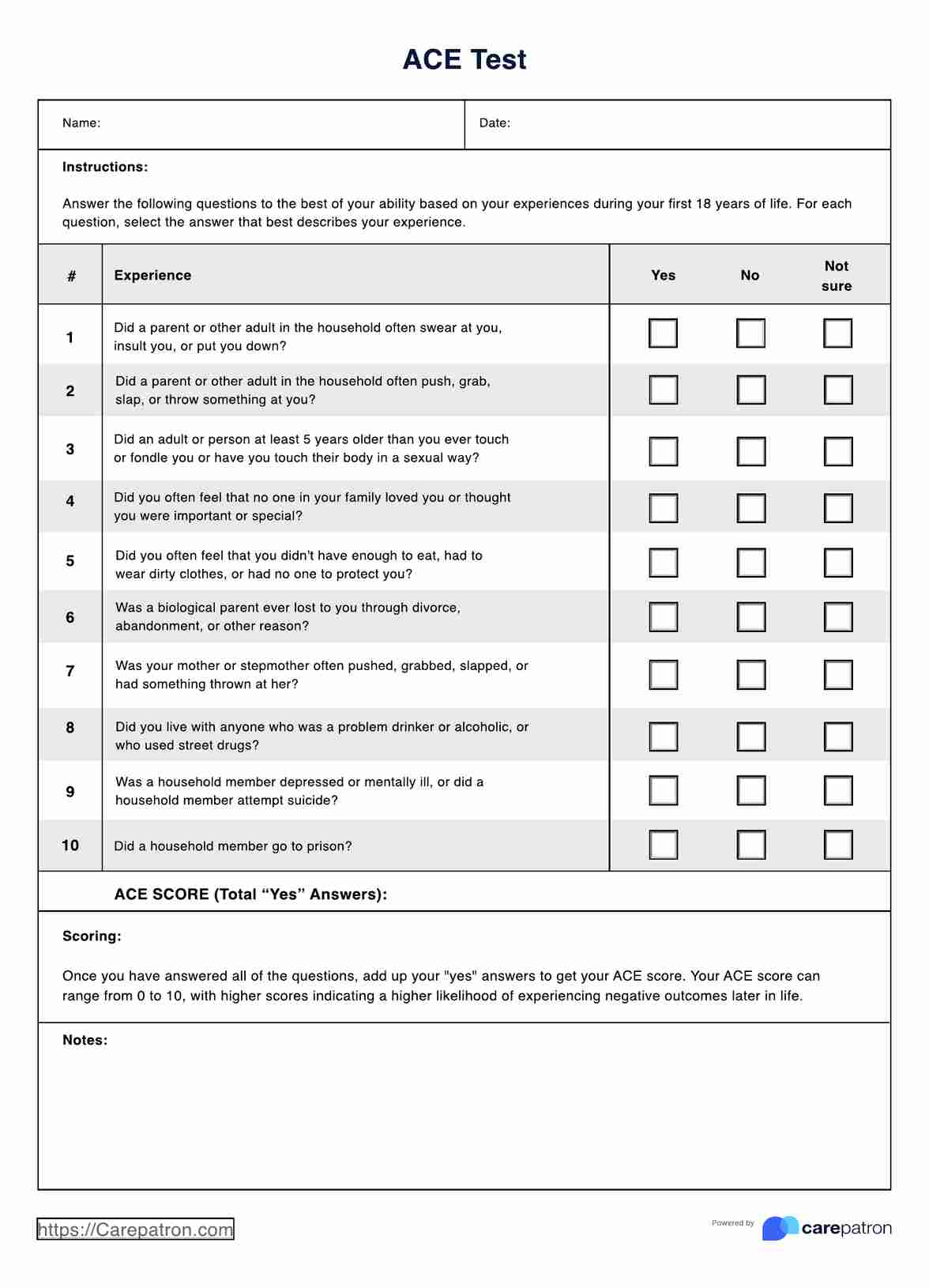
This section focuses on the client's unique experience and aims to address their symptoms and concerns through their perspective and determine the patient's chief complaint. Expect to include direct quotes, secondhand commentary from close relatives, and annotations of their current physical state.
Objective
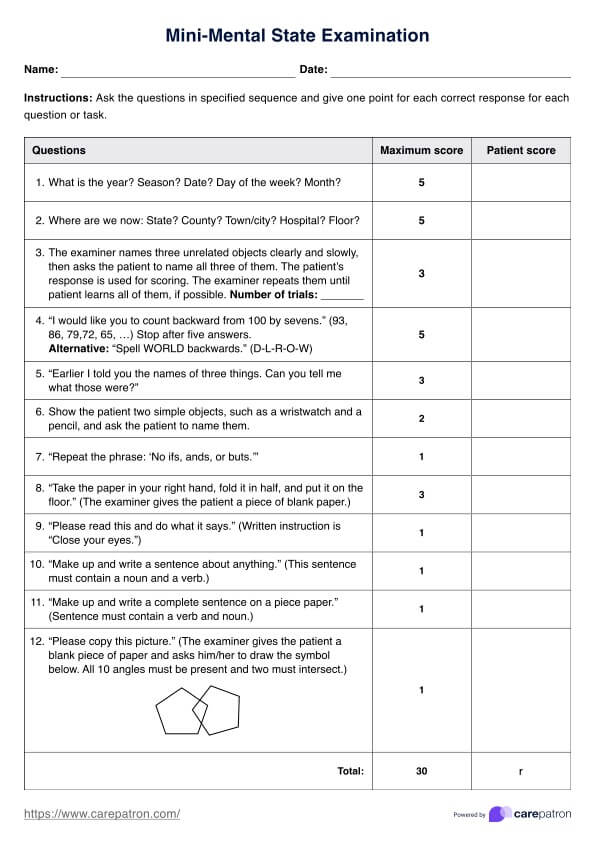
The objective section covers all observable facts using measured data. This may entail vital signs, such as blood pressure, height, and weight, as well as other assessments, the patient's medical records, and X-ray evidence. It is scientifically based, with all statements requiring supporting evidence.
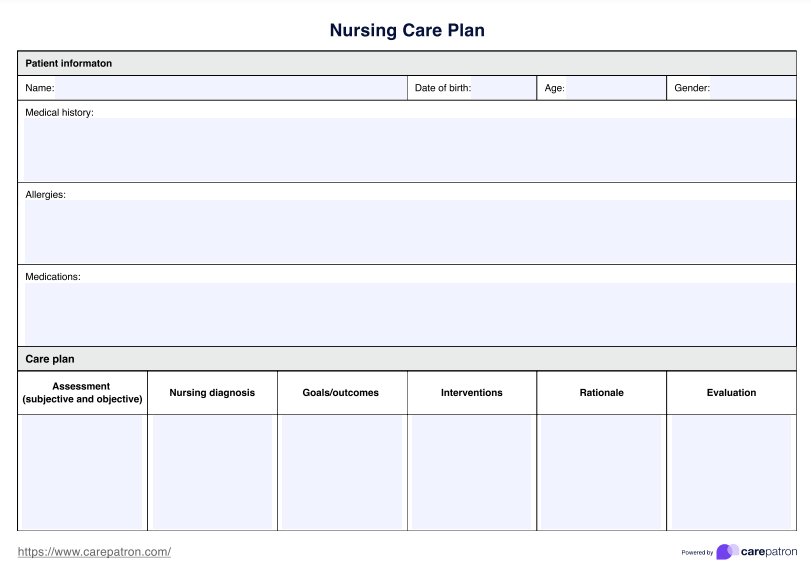
Assessment
The assessment section synthesizes subjective and objective information and requires an overall clinical assessment. This should summarize the client's health and typically involves notes on current medications and treatments and how they are progressing in each aspect.
Plan
In the final section, you must develop a plan to define and implement your client's next course of action for the patient's treatment. This may mean amending current treatment plans or recommending a new one entirely.
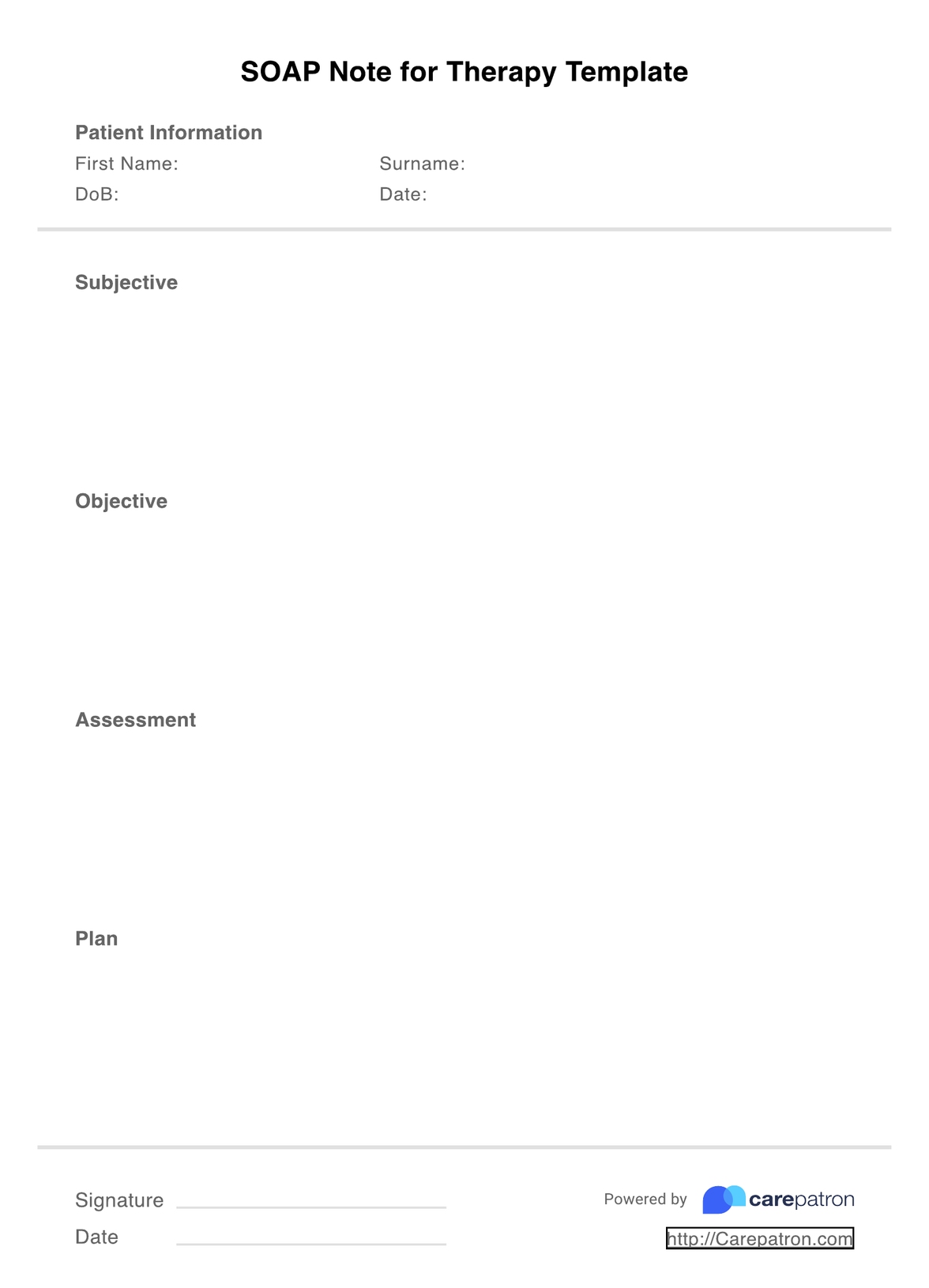
SOAP Notes for Therapy Template
SOAP Notes for Therapy Example
How to use this SOAP note for therapy template
Using SOAP note templates for your therapy practice can significantly boost the quality of your clinic. However, you may be wondering how exactly you use them. Fortunately, using SOAP notes is a super easy, intuitive tool that enables you to work smarter and improve the formatting of your note-taking.
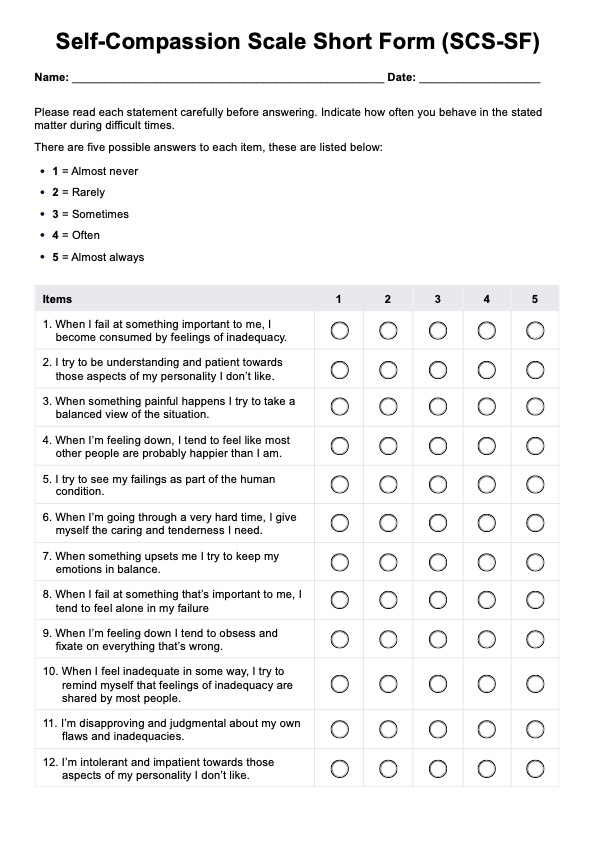
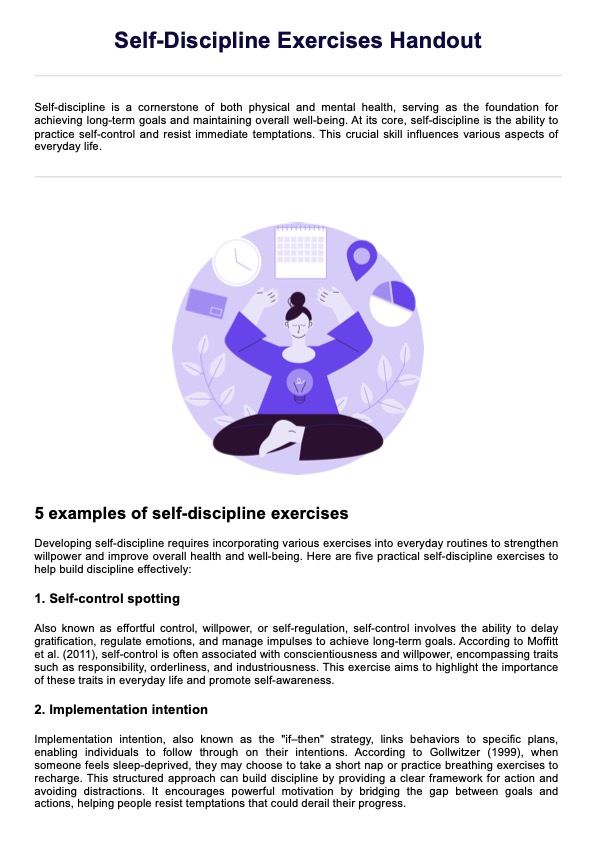
Step 1: Download the PDF template
Before you proceed, ensure you have the template downloaded on your chosen note-taking device. Your PDF software should also allow you to edit the page.
Step 2: Fill out your credentials
At the top of the page, you must fill out the date and time of your session with the client, their name and ID, and your professional details.
Step 3: Complete the four SOAP sections
Fill out the four subjective, objective, assessment, and plan sections, ensuring you cover all bases. Having all evidence in one place is crucial, and all information is brief and concise. Observing and documenting the client's mood and affect is vital. Remember that other practitioners may need to evaluate your notes, especially in case of legal action, so you should maintain a professional tone, with only factual data included.
Step 4: Sign
You should sign the document at the bottom of the page for verification, legal, and insurance purposes. This recognizes authority and ownership and ensures that you are accountable for the expertise you provide.
Step 5: Store your SOAP notes
After saving your SOAP note, storing the document within a HIPAA-compliant platform is very important. This significantly reduces the risk of security breaches and ensures your information is safeguarded and protected.
Who can use this template?
Mental health SOAP notes use a medically universal format, making them highly applicable across various disciplines and mental health disorders. For example, an anxiety SOAP note template might help document generalized anxiety disorder (GAD).
Regardless of the type of therapy field that you work in, almost all mental health practitioners can benefit from integrating this template within their workspace. Here are some of them:
- Cognitive behavioral therapists
- Dialectical behavioral therapists
- Addiction therapists
- Child therapists
- Clinical therapists
- Exercise therapists
- Trauma therapists
- Nutritional therapists
Although every mental health professional or therapist will conduct their business differently, and the content within the SOAP notes may be unique to the field, the format remains the same across all areas. The four subjective, objective, assessment, and plan areas will be covered in extensive detail, which is relevant for all types of therapy. Each SOAP note should also pertain to one individual, which is crucial to remember if you are more inclined to conduct group sessions.
Benefits of a therapy SOAP note template
Beyond necessity and saving time, there are several reasons why mental health professionals like you should incorporate SOAP notes into your practice. Here are some of them:
Promotes better clinical outcomes
With SOAP notes, you can effectively document a patient's medical records, track a client's health progress, and record more accurate information that touches on multiple subjective and objective realms. As a result, you can improve communication and your clinical decisions with a more accurate representation of the client's condition.
Ensures better consistency and organization
Standardizing your notes ensures professionalism and consistency. SOAP notes are an effective way to achieve this, as they allow you to maintain quality and criteria across clients. They organize information about the client's condition, combining assessment results, medication, and treatment plans in one place.
Enables collaboration
If needed, SOAP notes are a great way to collect secondhand assessments from the client's close relatives, providing a broader scope of their health. This unique approach enables healthcare practitioners to draft progress notes and treatment plans with the client's immediate needs.
.png)
Commonly asked questions
You must always provide a source if quoting a client, their close relatives, or even a healthcare professional. This professional practice ensures you have a solid foundation for reference if needed in the future.
Some clients may have more clinical information than others, and that's okay. However, a SOAP note should be 1-2 pages, with 3 pages indicating too detailed. Remember that SOAP notes should be an overview, with only necessary information summarized.
While you most certainly can handwrite SOAP notes, electronic is preferred. They are faster to create, and voice-to-text transcription services enable more accurate notes. Carepatron, amongst many other platforms, also provides a clinical documentation storage option, meaning you can protect all information. If you still prefer handwritten, consider scanning and storing these on a secure cloud platform.

.webp)




-template.jpg)