The primary nursing priority for respiratory failure is to see patient outcomes and ensure adequate gas exchange by optimizing oxygenation and ventilation. This includes monitoring abnormal breath sounds, assessing lung expansion, and managing respiratory function to prevent further deterioration.
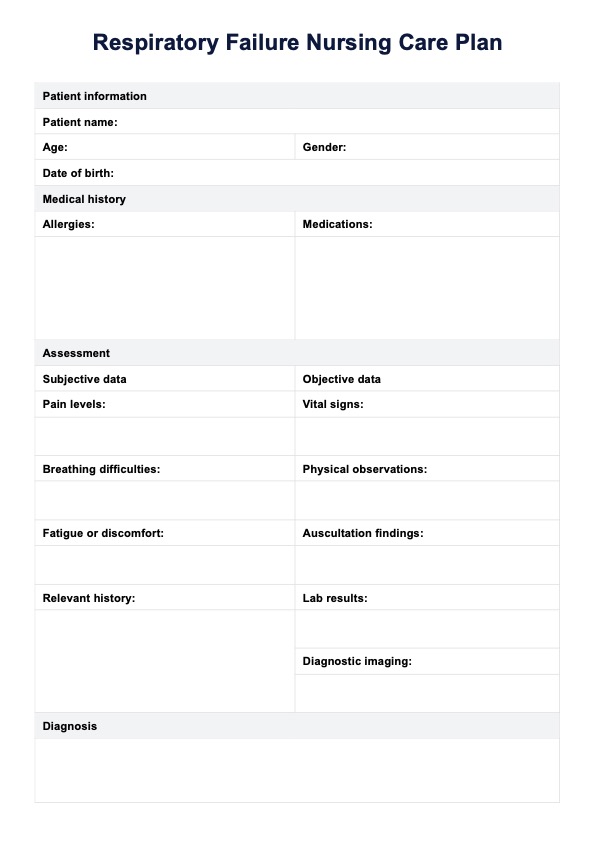
Respiratory Failure Nursing Care Plan
Elevate your patient care skills and learn to create effective care for respiratory failure with Carepatron's Respiratory Failure Nursing Care Plan template.
Use Template
Respiratory Failure Nursing Care Plan Template
Commonly asked questions
A common nursing diagnosis for respiratory distress is an ineffective breathing pattern due to impaired oxygenation, which may result from conditions like chronic lung disease or chronic respiratory failure.
Common nursing diagnoses for respiratory-related problems include Impaired Gas Exchange, Ineffective Airway Clearance, and Risk for Aspiration related to decreased cough reflex or altered level of consciousness.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











