Quantitative Sensory Testing
Explore Quantitative Sensory Testing (QST) with our free downloadable template. Learn how QST measures and assesses pain sensitivity, neuropathic pain, and sensory function.


What is Quantitative Sensory Testing?
Quantitative Sensory Testing, or QST testing, is a method used to assess and measure an individual's sensory nerve function by testing their response to specific stimuli. It is particularly useful in diagnosing conditions characterized by either reduced or heightened pain sensitivity, such as neuropathic pain, and in identifying abnormalities in sensory perception. This testing can help determine the severity and scope of nerve damage and contribute to tailoring personalized treatment plans for patients.
Conditions Quantitative Sensory Testing helps with
Quantitative Sensory Testing is a valuable diagnostic tool for a variety of medical conditions and injuries that impact sensory function and pain perception:
- Neuropathic pain: QST helps differentiate among various types of neuropathic pain, providing insights into the specific nerve fibers involved. This is crucial for tailoring targeted treatments for postherpetic neuralgia or diabetic neuropathy.
- Diabetes: Early detection of diabetic neuropathy is possible with QST by identifying diminished sensation to thermal and mechanical stimuli. This early diagnosis is key in implementing preventative measures to manage symptoms and prevent progression.
- Systemic diseases: Conditions such as multiple sclerosis and fibromyalgia, which can alter sensory perceptions and cause pain or discomfort, are assessed using QST to evaluate the extent of sensory nerve involvement and guide management strategies.
- Chemotherapy-induced peripheral neuropathy: For patients undergoing chemotherapy, QST is used to assess the onset and progression of peripheral neuropathy caused by the toxic effects of chemotherapeutic drugs. This helps adjust chemotherapy doses or add neuroprotective agents.
- Complex regional pain syndrome (CRPS): QST can measure changes in pain sensitivity and sensory thresholds, providing detailed information that supports the diagnosis of CRPS and monitors the efficacy of treatments.
Each of these applications underscores the versatility of the QST methodology in enhancing our understanding of sensory impairments and refining patient care across multiple medical disciplines.
Components of Quantitative Sensory Testing
Quantitative Sensory Testing is a sophisticated diagnostic approach that evaluates the sensory function of subjects by testing various aspects of nerve response. It is comprised of multiple components:
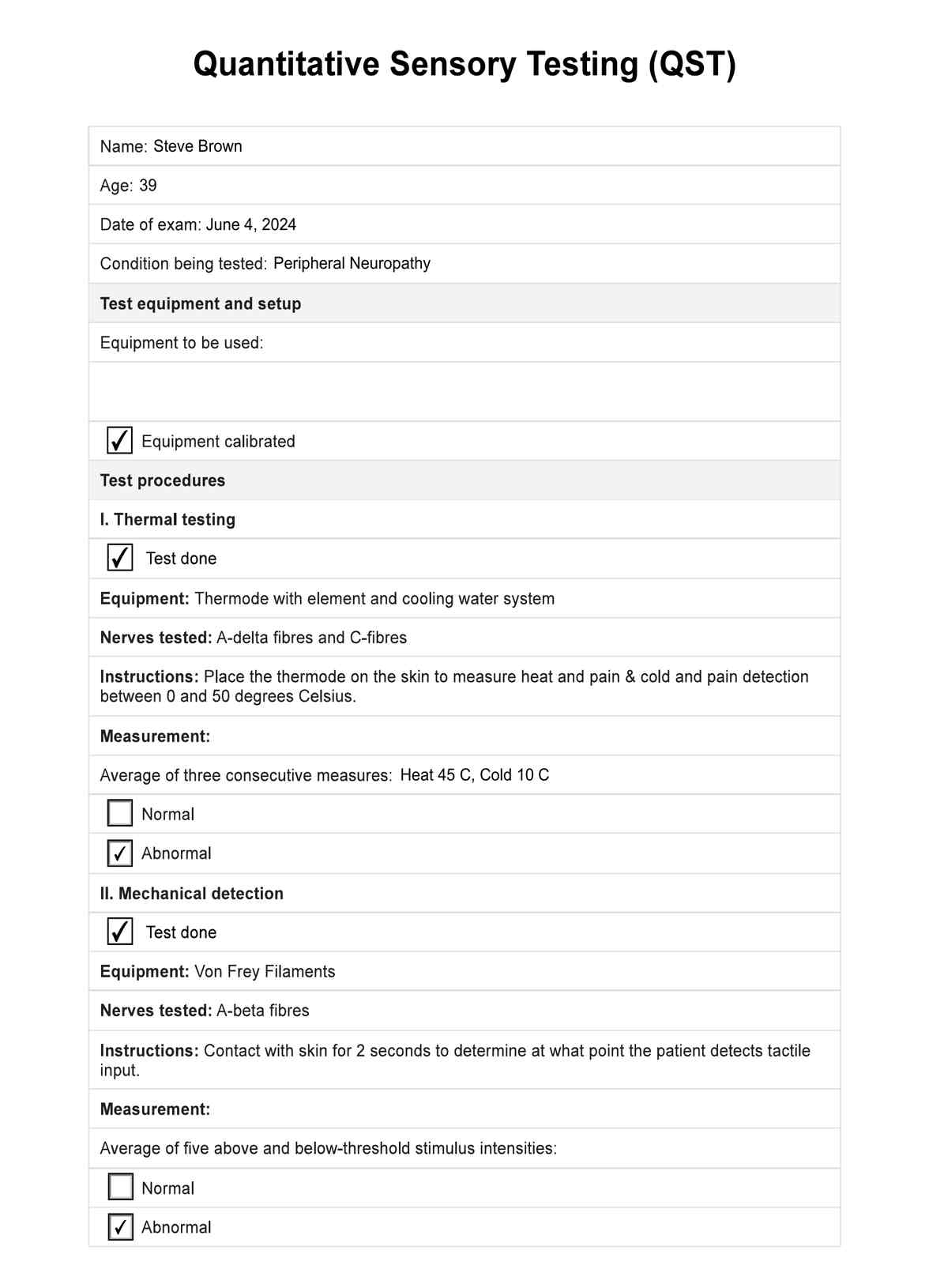
- Thermal testing: This test measures the individual's ability to perceive temperatures, assessing responses to heat and cold stimuli. This helps identify nerve damage or dysfunction related to thermal perception, which is crucial for neuropathic pain and paradoxical heat sensation.
- Mechanical sensitivity: This involves testing the response to touch and pressure, helping to determine thresholds for tactile and mechanical pain. It is vital for diagnosing conditions that involve altered mechanical sensitivity, such as diabetic neuropathy and fibromyalgia.
- Pain response: This component evaluates the patient's reaction to painful stimuli (nociceptive testing) to determine pain thresholds and tolerance. It is particularly useful in understanding the severity and type of pain, such as neuropathic pain or increased pain sensitivity.
- Vibration testing: Assesses the sensitivity to vibration, which can indicate the status of nerve function, particularly those that carry vibration and touch sensations from the periphery to the brain. This test is essential for detecting early signs of diseases affecting peripheral nerves.
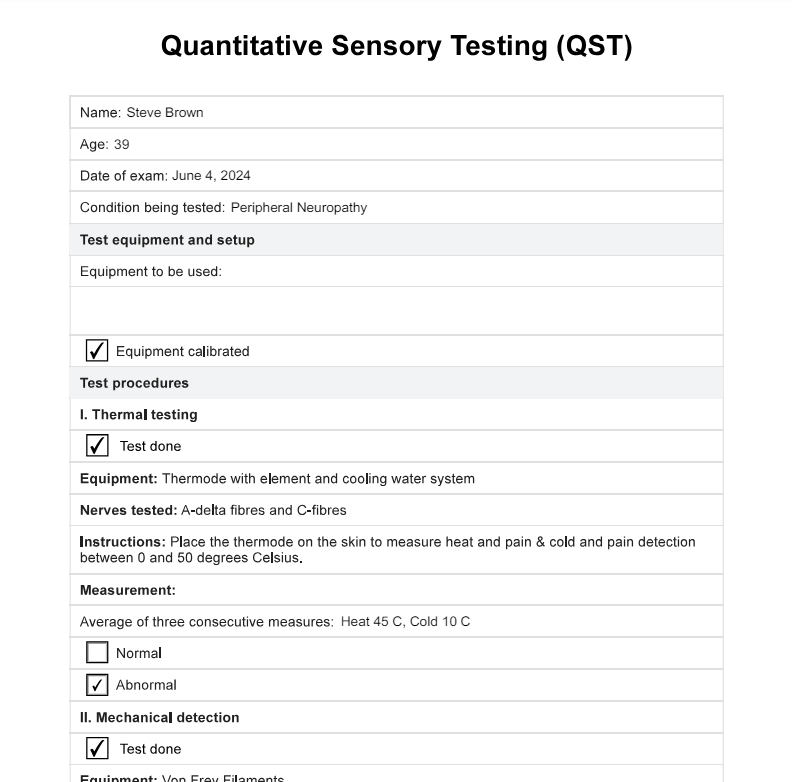
Quantitative Sensory Testing Template
Quantitative Sensory Testing Example
How to do Quantitative Sensory Testing
Performing QST involves a structured assessment procedure to ensure accurate and reliable results:
- Preparation: The skin area where the tests will be conducted is prepared, ensuring clean and normalized to room temperature to avoid external influences on sensory perception.
- Stimulation: Specialized devices deliver controlled thermal, mechanical, or vibrational stimuli to the skin. These devices can adjust the intensity and duration of the stimuli to measure the sensory thresholds precisely.
- Response recording: The patient's responses are meticulously recorded, noting the exact points at which sensations are perceived or when pain is initiated. This step is crucial for mapping sensory function and identifying deviations from normal sensory processing.
These components and procedures make QST a valuable tool in the clinical assessment of sensory function and pain management, providing key insights into the underlying mechanisms of sensory and pain disorders.
How does our Quantitative Sensory Testing template work?
Here’s how to enhance the explanation of the QST template:
Step 1: Download our template
Start by downloading our QST template to ensure a standardized approach to sensory testing. You can also choose to fill it out online instead.
Step 2: Prepare the patient and the equipment
Before starting, verify that all necessary equipment is operational and the patient is properly prepared. This includes ensuring the testing environment is suitable and that the patient understands the procedures. Calibrate each piece of equipment that will be used.
Step 3: Do the tests
The template guides clinicians through each phase of the sensory testing. It provides a systematic approach for applying stimuli and accurately recording the methods used, ensuring that each test is conducted consistently across different sessions or clinicians.
Step 4: Document results
This part of the template is designed to record detailed patient responses. Clinicians can note the thresholds at which sensations are detected, and pain is perceived and report any significant patient remarks or clinical observations. This data is crucial for analyzing sensory function and making informed clinical decisions.
This structured template streamlines the process of conducting quantitative sensory tests. It enhances the accuracy and reliability of the results reported, providing a valuable tool for diagnosing and managing sensory disorders.
Results, interpretation, and next steps
Upon completing the QST, the evaluation process unfolds as follows:
Results interpretation
Specialists meticulously analyze the collected data to establish sensory thresholds and pinpoint any abnormalities in sensory function. This stage is crucial for detecting and diagnosing conditions affecting sensory perception.
Clinical decision making
Using the insights gained from the QST results, healthcare providers can make informed decisions about additional diagnostic evaluations or begin appropriate treatment strategies tailored to the patient's needs.
Follow-up measures
Follow-up QST sessions may be periodically conducted to effectively track sensory impairments' evolution or assess ongoing treatments' impact. This continual health monitoring helps adjust treatments as necessary and evaluate the long-term health outcomes of therapeutic interventions.
These steps ensure that each phase of the sensory testing contributes effectively to comprehensive patient care, enhancing diagnostic accuracy and therapeutic outcomes.
Commonly asked questions
Quantitative Sensory Testing (QST) is crucial for diagnosing neuropathic pain by measuring responses to controlled sensory stimuli like heat, cold, and mechanical pressure. It assesses heat pain and sensitivity and can identify paradoxical and heat pain sensations often indicative of neuropathic conditions.
Psychological factors can significantly influence Quantitative Sensory Testing (QST) outcomes by affecting a patient's pain perception. Stress, anxiety, and expectations can alter how pain stimuli are processed, underscoring the need to consider psychological assessments alongside the evaluation of patients' QST results.
Yes, Quantitative Sensory Testing (QST) can be instrumental in identifying individuals at risk of developing disorders characterized by increased pain sensitivity, such as fibromyalgia pain or chronic post-surgical pain, by measuring baseline pain thresholds and responses to painful stimuli.

.jpg)