Interventions for a patient with respiratory distress may include administering supplemental oxygen, positioning for optimal lung expansion, monitoring respiratory status, providing respiratory medications, and initiating ventilatory support if necessary.
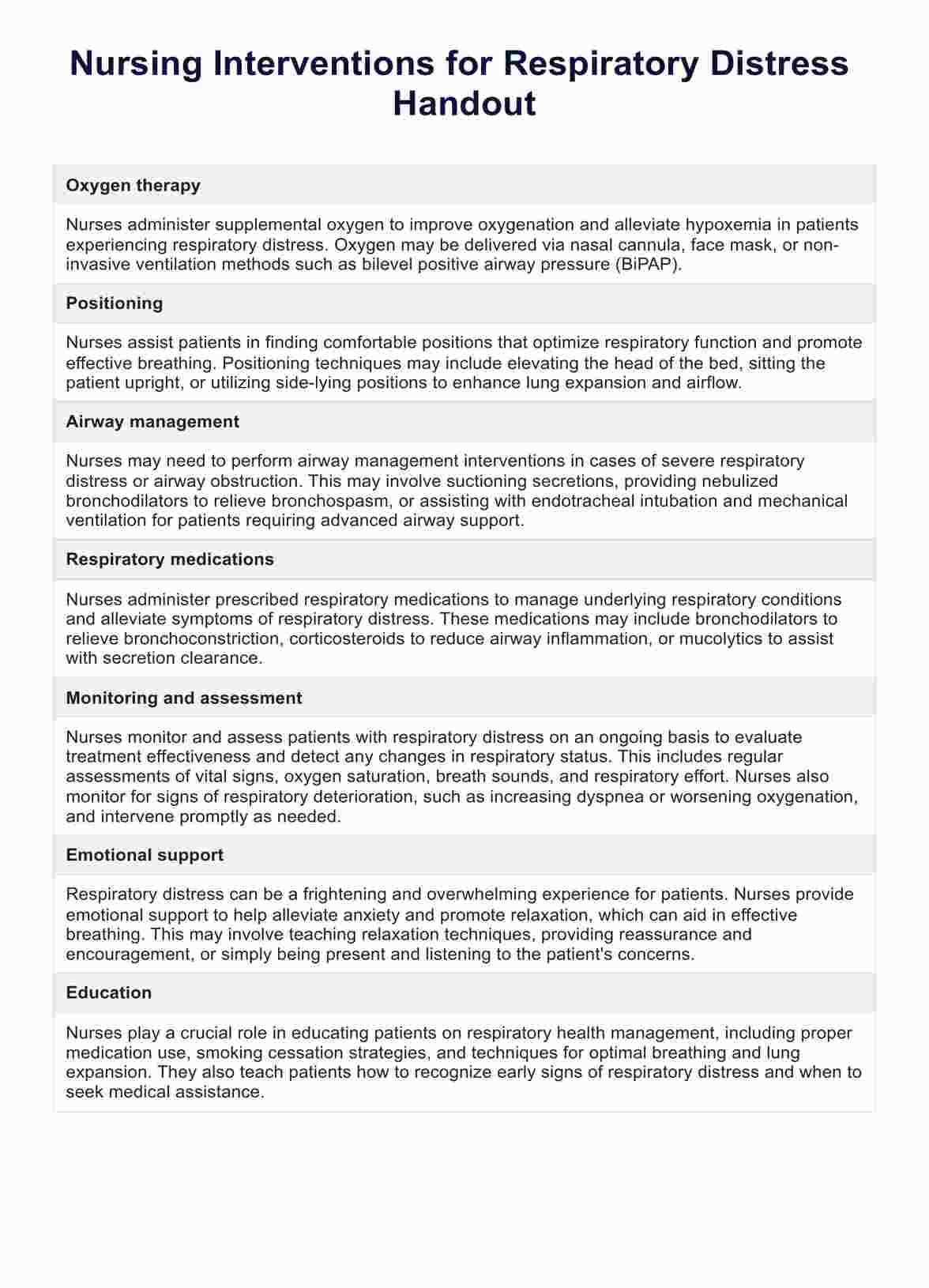
Nursing Interventions for Respiratory Distress Handout
Discover essential nursing interventions for managing respiratory distress with a helpful example PDF download from Carepatron. Level up your skills now!
Use Template
Nursing Interventions for Respiratory Distress Handout Template
Commonly asked questions
Caring for a person in respiratory distress involves maintaining a patent airway, supporting oxygenation, assessing vital signs, administering prescribed medications, and closely monitoring for signs of deterioration.
The immediate action for respiratory distress is to assess the patient's airway, breathing, and circulation (ABCs), administer oxygen if available, and summon additional assistance if needed.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











