Mental Status Exam Template
Use our concise and customizable Mental Status Exam Template to evaluate clients' mental state and functioning in a structured way.


What is a Mental Status Exam?
A Mental Status Exam (MSE Assessment) is a structured psychiatric assessment tool used by healthcare professionals to evaluate an individual's cognitive, emotional, and behavioral functioning. It is the psychological equivalent of a physical exam and provides valuable insights into the patient's mental state. The MSE template covers several domains: appearance, behavior, speech, mood, thought process, thought content, perception, cognition, insight, and judgment. This involves assessing whether a client's presentation is within the normal range of responses (Sadock et al., 2015).
The MSE is commonly used to diagnose mental health conditions and develop therapeutic interventions. Furthermore, it assists in assessing the risk of harm to self or others. Understanding how to administer an MSE can be helpful in treatment planning and identifying immediate intervention needs.
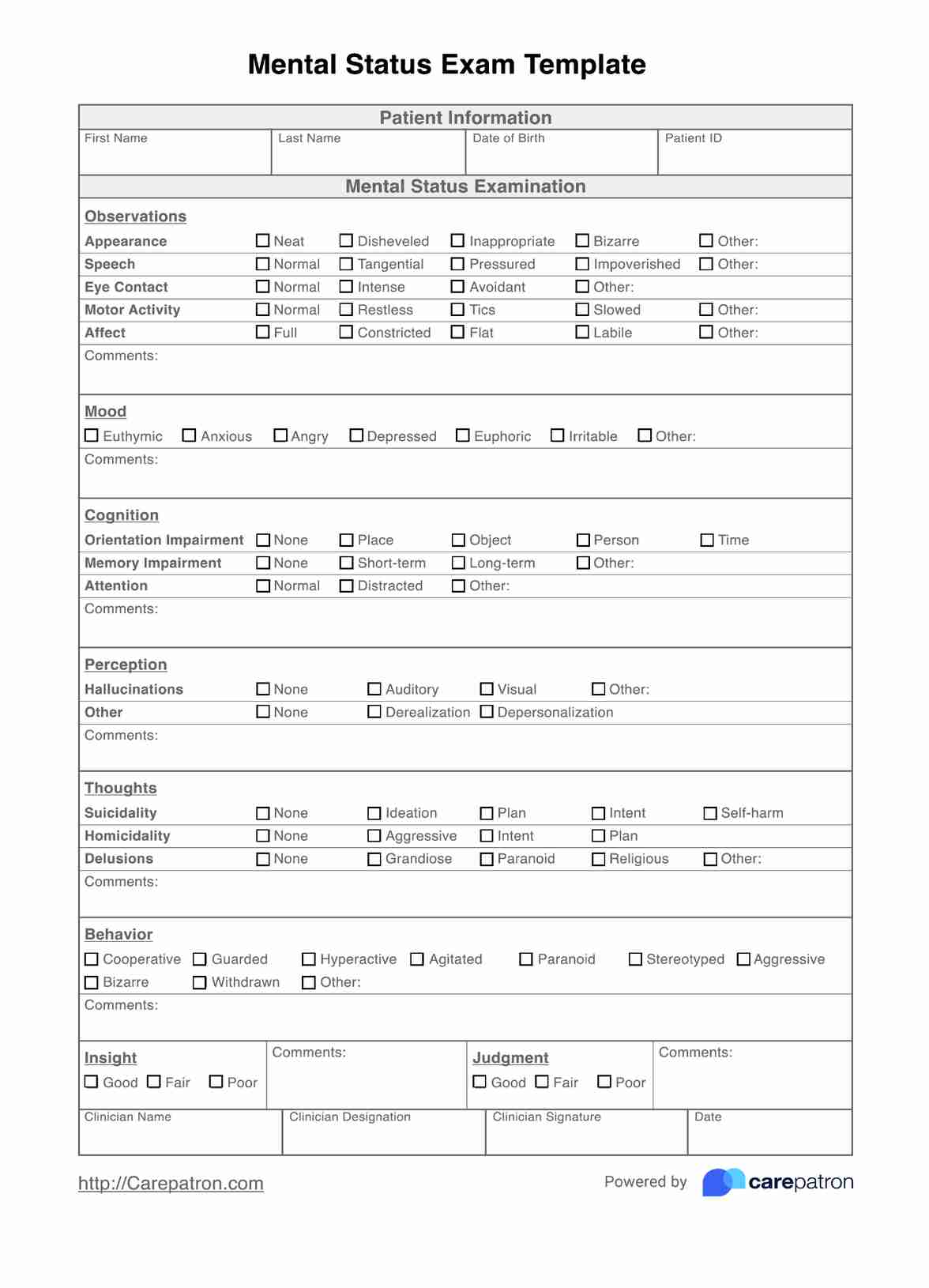
Mental Status Exam Template
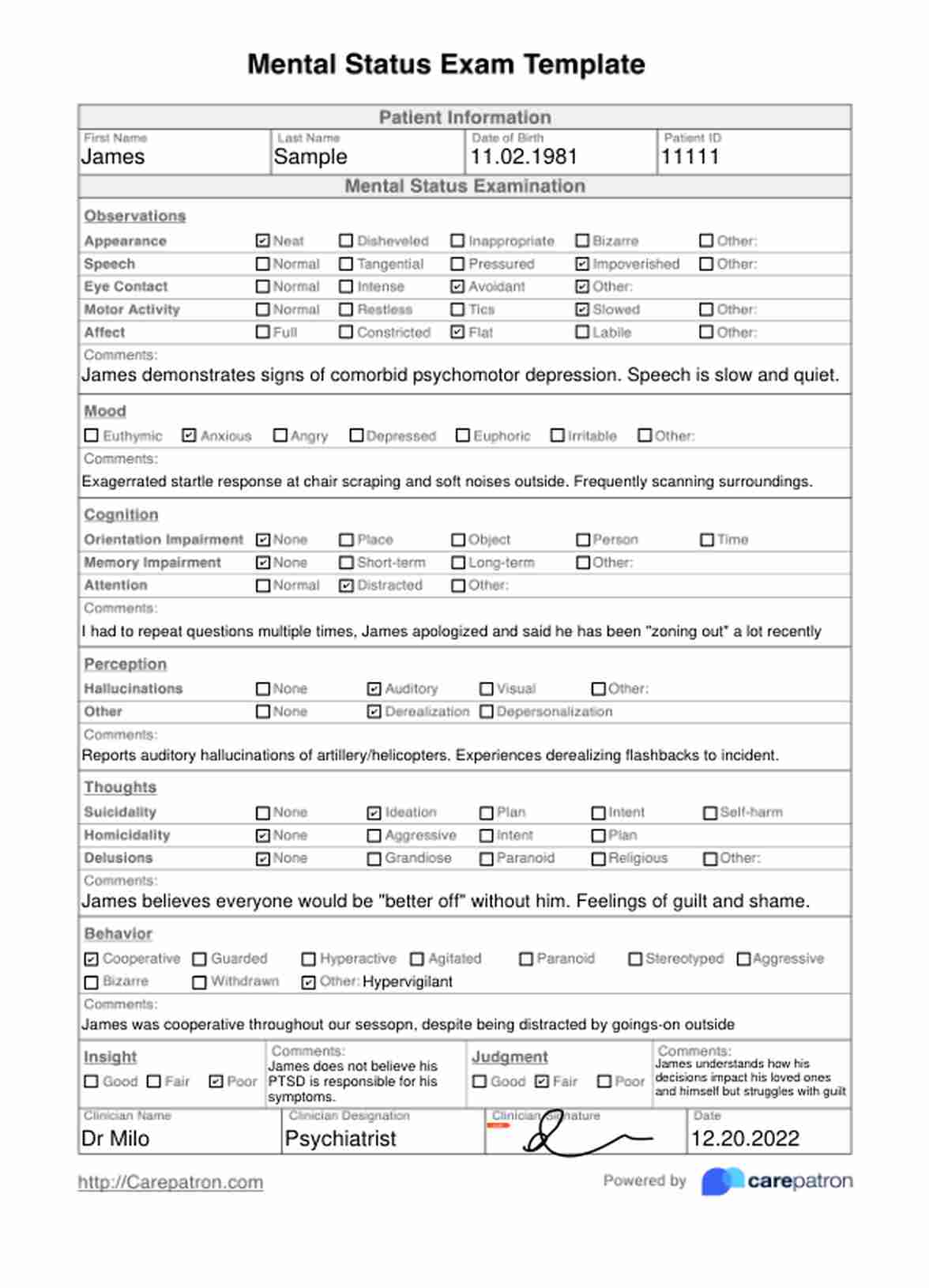
Mental Status Exam Template Example
What is included in a Mental Status Exam?
While it can be tailored to the specific needs of the patient, a comprehensive Mental Status Exam typically covers these key areas (Voss & Das, 2022):
Appearance and behavior
The Mental Status Exam begins with observing the patient's appearance and behavior, including personal hygiene, whether they are dressed appropriately, eye contact, facial expression, and posture. A practitioner might also note repetitive movements or abnormal movements during the session. These observations can provide clues about the patient's mental status, physical health, emotional state, and potential neurological conditions.
Speech
Assessing the patient's speech involves evaluating qualities such as rate, volume, articulation, and coherence. Abnormalities in speech, such as pressured speech, monotonous speech, slurred speech, or word salad (incoherent speech), can indicate an underlying mental health problem or cognitive impairment.
Mood and affect
The Mental Status Exam assesses the patient's affect, which refers to their emotional expression, and their mood, which refers to their subjective emotional state. Healthcare professionals observe the patient's facial expressions, eye contact, and body language, which can be mood-congruent or incongruent.
Thought process and content
Evaluating the patient's thought process involves assessing their thoughts' logical flow and organization. Practitioners may also explore the content of the patient's thoughts, including the presence of any delusions (fixed and false beliefs), hallucinations (perceptual abnormalities such as auditory hallucinations), loose associations, overvalued ideas (unreasonable and sustained belief of less than delusional intensity), or obsessions.
Cognition
The cognitive domain of the Mental Status Exam assesses various aspects of the patient's cognitive functioning, including orientation (awareness of self, time, and place), attention, concentration, memory (recent and long-term), language abilities, and executive functioning (problem-solving, abstraction, and fair judgment).
Insight and judgment
Insight refers to the patient's understanding and awareness of their mental health condition. At the same time, judgment involves evaluating the patient's ability to make reasonable decisions and understand the consequences of their actions. Poor insight and impaired judgment can often accompany various psychiatric disorders and personality disorders and may influence treatment adherence and decision-making.
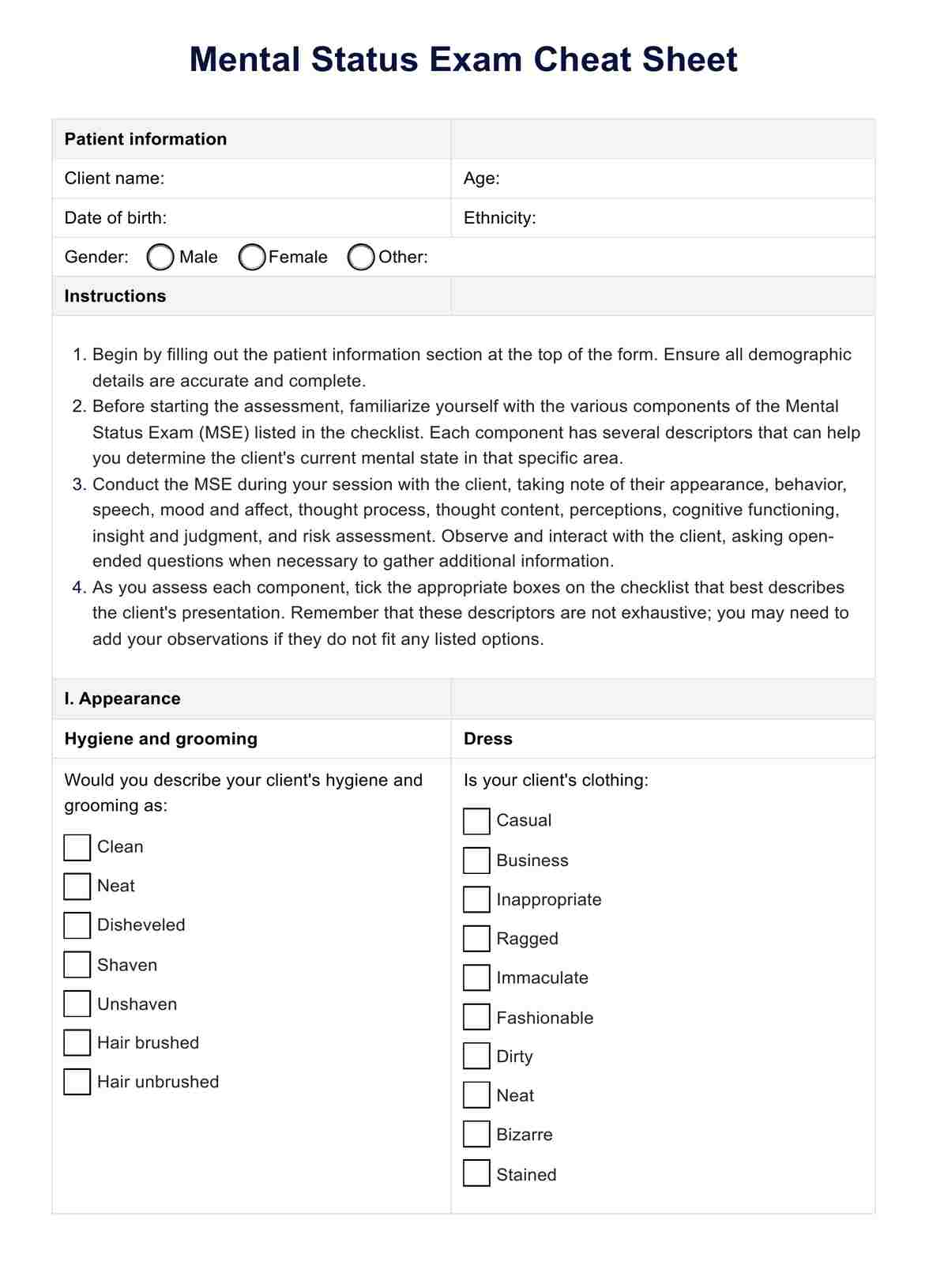
How to use this free Mental Status Exam Template
To start using this template in your own practice, healthcare providers can follow these steps:
Step 1: Gather information
Before conducting the mental status exam, review the client's medical history, stated age, presenting concerns, and any relevant background information. This will help you tailor the exam and focus on areas requiring further testing and exploration.
Step 2: Observe appearance and behavior
Start the exam by observing physical signs. This includes the client's appearance, their grooming, hygiene, and clothing. Note any unusual behaviors, such as unusual movements, agitation, or signs of self-neglect. Pay attention to their eye contact, posture, and overall presentation.
Step 3: Assess speech and language
Evaluate the client's speech patterns, including rate, tone, and volume, and note any abnormalities. Additionally, assess their language abilities, including comprehension, naming, and repetition.
Step 4: Explore mood, thought process, and content
Assess their mood and affect, noting any incongruence between their reported mood and observed emotional expression. Evaluate the client's thought process, including their thoughts' logical flow, organization, and coherence. Explore the content of their thoughts, looking for any delusions, hallucinations, or obsessions.
Step 5: Evaluate cognition, insight, and judgment
Assess the client's cognitive functioning, including orientation to time and current location, attention, concentration, memory, and executive functioning. Determine the client's level of insight into their condition and evaluate their judgment and decision-making abilities.
Step 6: Complete notes and comments
As you complete the MSE, add any comments to elaborate as needed. These comments may be useful for remembering important points you wish to return to with your patient, and it's best to note these down as soon after observing as possible.
Read our blog article about how to conduct a mental status exam to learn more.
Scoring and interpretation
Accurately interpreting the results of a mental status exam (MSE) is crucial for providing appropriate care and support to individuals. When interpreting the MSE results, it is essential to consider the individual's baseline functioning, cultural background, and any potential factors that may influence their presentation during a session. The observations should be interpreted in the context of the individual's unique circumstances and presenting concerns.
Significant deviations from expected norms or changes from the individual's baseline functioning may indicate the presence of cognitive impairment, mental illness, or other underlying health issues that require further evaluation and intervention.
It's important to note that the interpretation of the MSE should be based on the overall clinical picture, considering the patient's medical history, presenting symptoms, and any additional diagnostic information. Scoring and observing alone may not provide a definitive diagnosis, but it can help identify areas of concern and guide further evaluation or treatment planning.
When should you do a Mental Status Examination?
A Mental Status Examination is a crucial assessment tool that healthcare professionals should consider administering to evaluate a patient's mental and cognitive functioning. Here are some common scenarios when conducting this would be appropriate:
Suspected cognitive impairment
If a patient exhibits signs of cognitive decline, such as forgetfulness, confusion, or difficulty with daily activities, a mental status examination like the Mini-Mental State Examination template (MMSE test) or the Montreal Cognitive Assessment (MoCA) can help identify the presence and severity of cognitive impairment, which may be indicative of conditions like dementia or other neurological disorders.
Mental health concerns
A comprehensive mental status examination is recommended when a patient presents with symptoms of a potential mental health condition, such as depression, anxiety, psychosis, or substance misuse. The MSE can help assess the patient's level of insight, thought processes, and the presence of abnormal belief, thought insertion, or thought broadcasting.
Changes in behavior or functioning
If a patient experiences significant changes in their behavior, mood, or ability to carry out daily activities, a mental status examination can help identify potential underlying mental health issues or cognitive impairments that may be contributing to these changes.
Eating disorders
In cases of suspected eating disorders, such as anorexia nervosa, a mental status examination can provide valuable information about the patient's thought processes, body image distortions, and level of insight regarding their condition.
Trauma or head injury
After a traumatic event or head injury, a mental status examination can help assess the patient's cognitive functioning, both short-term and long-term memory, and overall mental state.
Clinical psychology and psychiatric evaluations
In clinical psychology and psychiatric settings, a mental status examination is often a crucial component of the initial evaluation and ongoing monitoring of patients with various mental health conditions, personality disorders, or thought disorders, such as thought blocking or loose associations.
References
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences/clinical psychiatry (11th ed.). Wolters Kluwer Health.
Voss, R. M., & Das, J. M. (2022). Mental status examination. National Library of Medicine; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK546682/
Commonly asked questions
To write a brief Mental Status Exam (MSE), focus on key areas such as appearance, behavior, speech, mood, affect, thought process, thought content, cognition, insight, and judgment. Provide a concise description of the individual's presentation in each area, noting any abnormalities or noteworthy observations to provide a picture of their mental functioning during assessment.
The five categories of the Mental Status Exam (MSE) typically include appearance and behavior, speech and language, mood and affect thought content, and cognitive function. Each category assesses different aspects of an individual's mental state to evaluate their cognitive and emotional functioning comprehensively.
To write a good Mental Status Exam (MSE), be concise but thorough. Objectively describe your observations across all relevant domains. Organize your assessment in a logical flow. Use clear, professional language with objectivity. Document any positive and negative findings that may aid diagnosis and treatment planning.












-template.jpg)