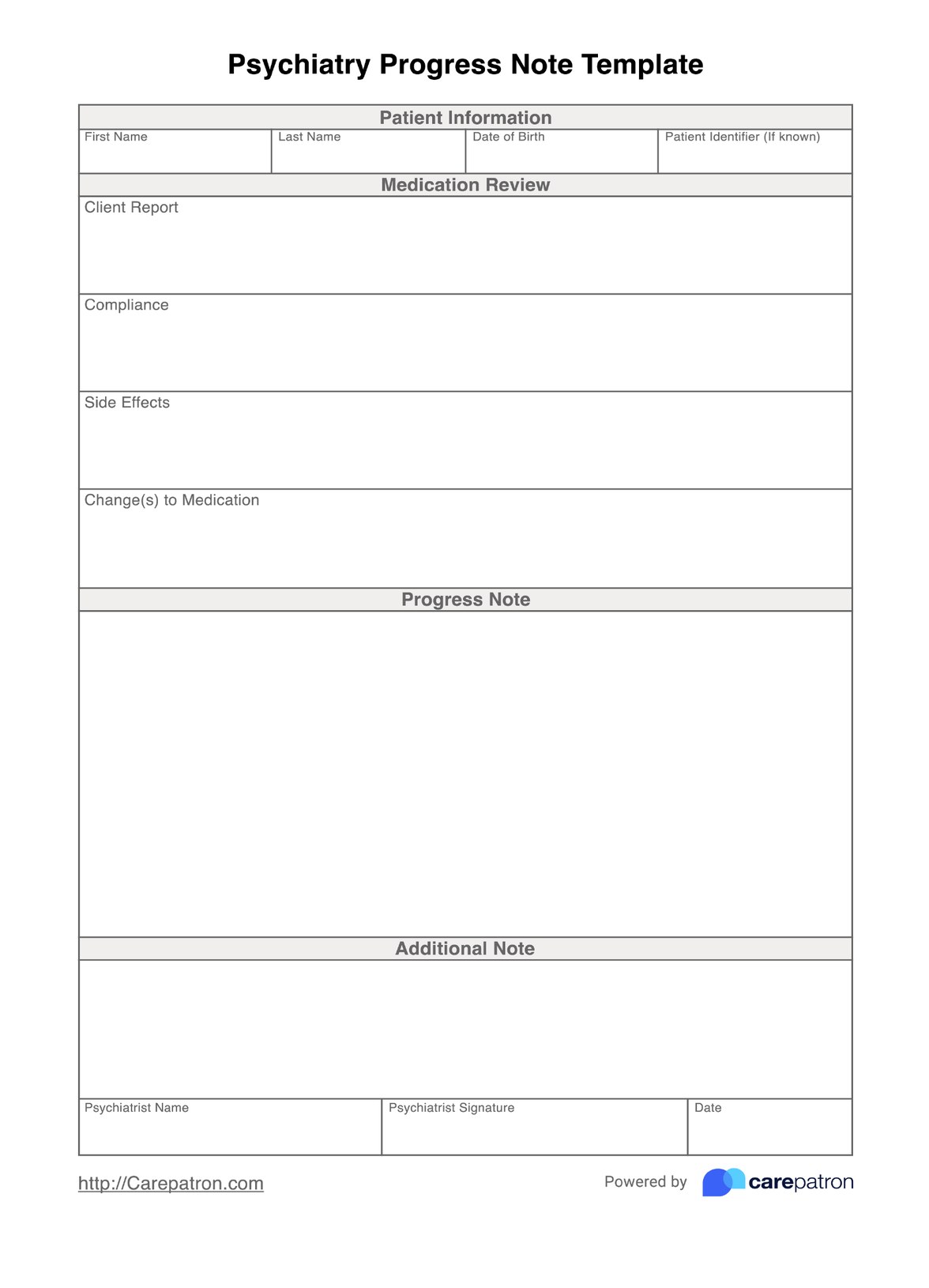
A psychiatric progress note should include all relevant updates on your patient’s condition since their last appointment with you. This might include responses to medication, subjective reports of their mood or behavior since the last time they saw you, their compliance with medication, and any proposed changes to their treatment plan.
Psychiatry Progress Note Template
Standardize your note-taking using our psychiatry progress note template, specially designed to save psychiatrists time and keep their notes organized.
Psychiatry Progress Note Template Template
Commonly asked questions
Progress notes are designed to be concise updates at each follow-up appointment following an initial consultation. As such, if a particular detail is unchanged or irrelevant to the patient’s progress, it can be omitted or noted as “no change”.
Your patient’s full medical history is generally taken in their initial consultation with you. As these progress notes are designed for appointments following their initial consultation, we don’t recommend you note down your patient’s entire history in this progress notes template. Instead, your patient’s interval history, i.e. their history since the last time they saw you, should be documented including their interval medication history, and results of any additional psychiatric examinations or mental status examinations.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











