Motor Assessment Scale
Carepatron's Motor Assessment Scale free PDF download provides a comprehensive understanding of motor assessment and give accurate diagnosis.


What is a stroke?
A stroke occurs when blood flow to a specific part of the brain is disrupted, either due to a blockage in a blood vessel (ischemic stroke) or when a blood vessel bursts (hemorrhagic stroke). This interruption deprives the brain tissue of oxygen and nutrients, leading to cell damage and potentially permanent neurological deficits. Among the expected consequences of acute stroke is the impairment of motor function, which affects muscle control and movement.
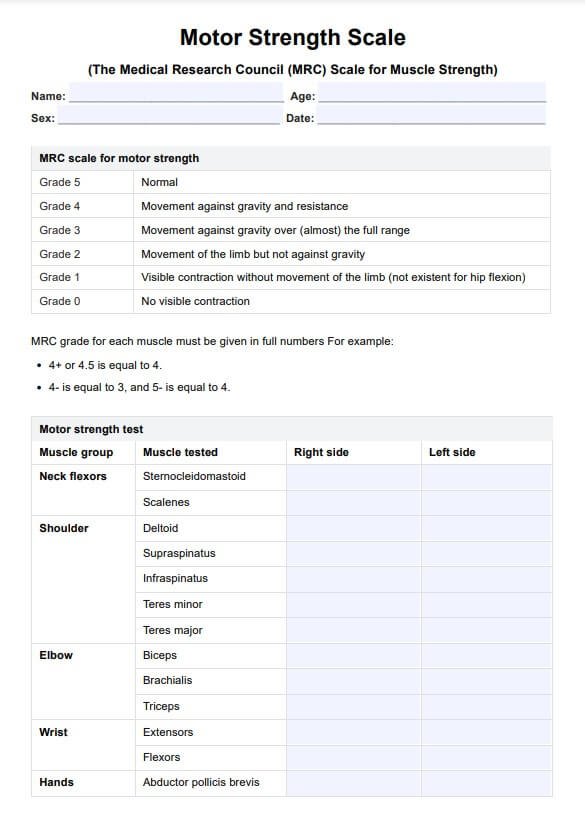
Assessing motor function post-stroke in clinical rehabilitation is paramount to designing effective treatment plans. Tools like the Action Research Arm Test (ARAT) are frequently employed to evaluate upper limb function, which is crucial for daily activities. Physical therapy, a cornerstone of stroke rehabilitation, focuses on restoring muscle strength, coordination, and range of motion.
Muscle tone, another aspect assessed during stroke rehabilitation, refers to the tension or resistance level in muscles at rest. Managing muscle tone aids in improving movement quality and function. Through physical medicine interventions and clinical rehab techniques, stroke patients undergo targeted therapies aimed at enhancing motor skills and overall functionality.
Reliability in stroke assessment tools ensures consistency in evaluating patient progress and treatment efficacy over time. With reliable measures, clinicians can track changes in motor function, muscle strength, and coordination, enabling tailored interventions to optimize recovery outcomes for stroke survivors.
How to diagnose a stroke
Diagnosing a stroke promptly is crucial for initiating appropriate treatment and minimizing long-term consequences. Here are the key steps and procedures involved:
- Assessment of symptoms: Recognize common signs of stroke such as sudden numbness or weakness in the face, arm, or leg, especially on one side of the body. Other symptoms include confusion, trouble speaking or understanding speech, difficulty seeing, dizziness, and severe headache.
- FAST test: Use the FAST acronym to assess for signs of stroke quickly: face dropping, arm weakness, speech difficulty, and time to call emergency services if all of these symptoms are present.
- Medical history review: Gather information about the patient's medical history, including risk factors such as hypertension, diabetes, smoking, and previous strokes or transient ischemic attacks (TIAs).
- Physical examination: Conduct a thorough neurological examination to assess motor function, sensation, coordination, and reflexes. Look for asymmetry or weakness in facial muscles, arm drift, and abnormal gait.
- Diagnostic tests: Perform imaging studies such as a CT scan or MRI to visualize the brain and identify areas of ischemia or bleeding. Additionally, a CT angiography or MR angiography may be used to evaluate blood flow in the cerebral arteries.
- Blood Tests: Analyze blood samples to assess for abnormalities such as elevated levels of glucose, lipids, or clotting factors, which may indicate an increased risk of stroke.
- Electrocardiogram (ECG or EKG): Record the electrical activity of the heart to detect arrhythmias or other cardiac abnormalities that could contribute to stroke risk.
- Carotid ultrasound: Use ultrasound imaging to assess for narrowing or blockages in the carotid arteries, a common cause of ischemic stroke.
- Lumbar puncture (spinal tap): Occasionally, a lumbar puncture may be performed to analyze cerebrospinal fluid for signs of bleeding or infection.
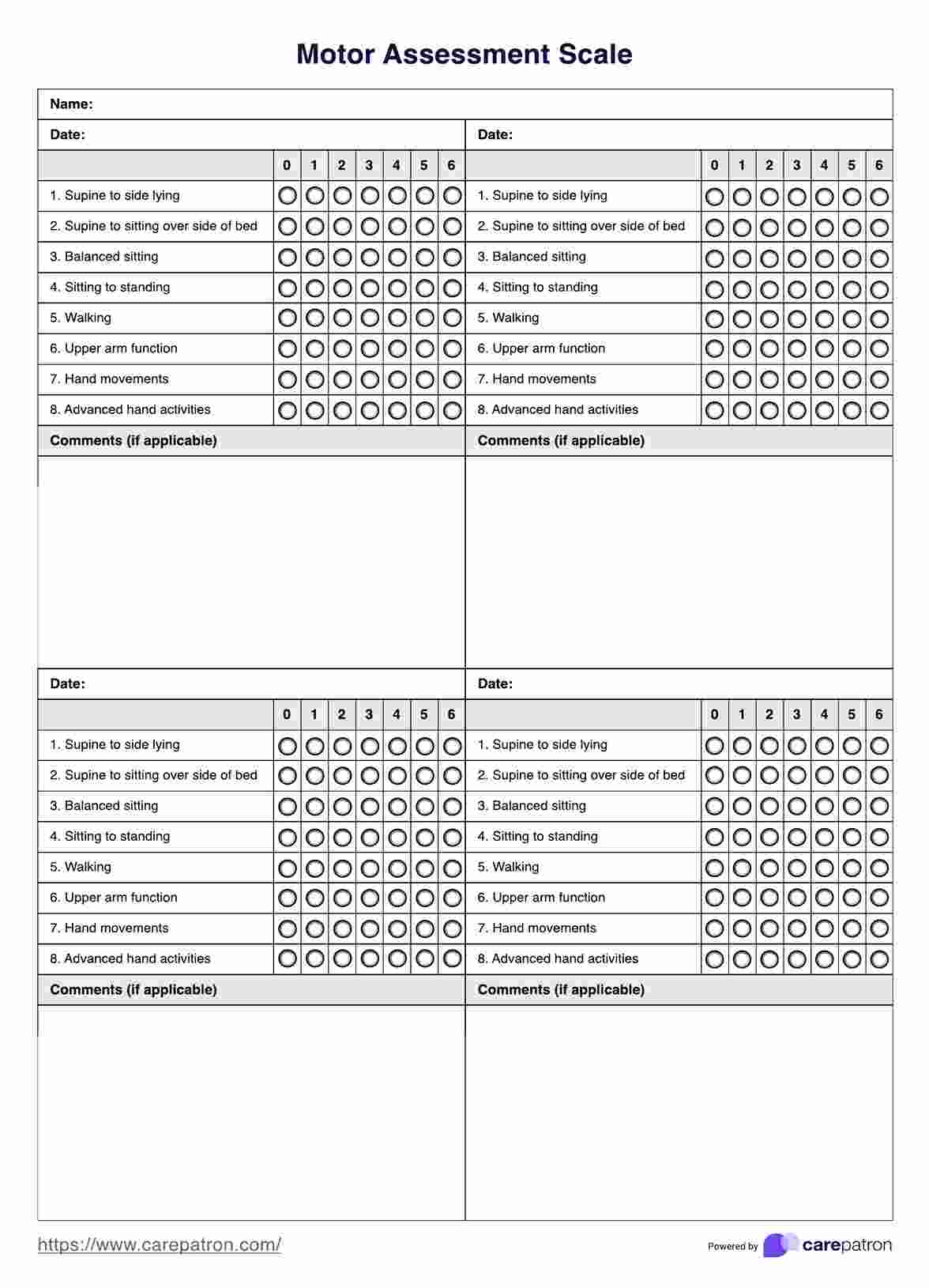
Motor Assessment Scale Template
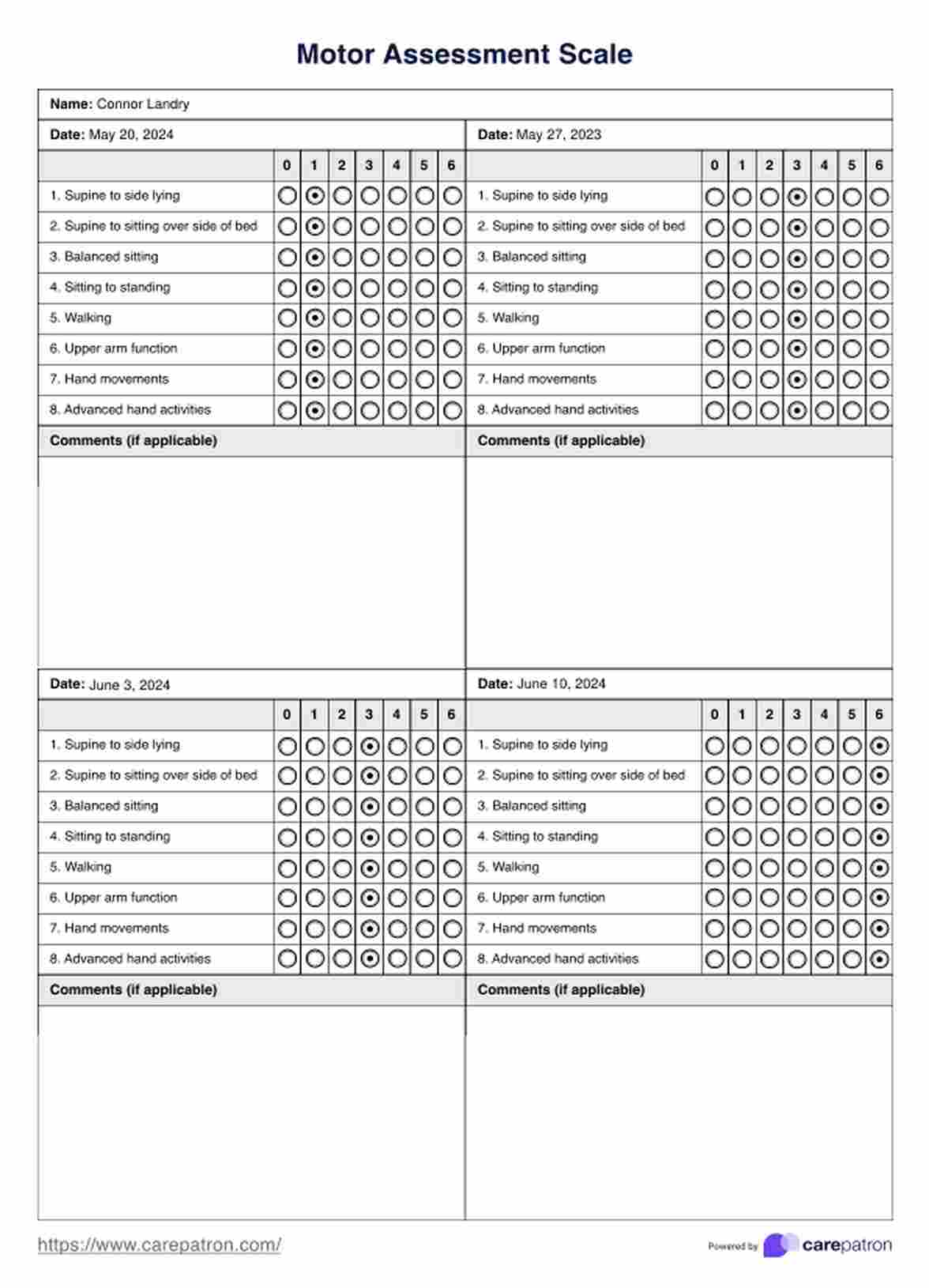
Motor Assessment Scale Example
What is the Motor Assessment Scale?
The Motor Assessment Scale (MAS) is a standardized tool healthcare professionals use to assess motor function in patients recovering from stroke or other neurological conditions. It evaluates motor abilities across eight key areas: reaching, grasping, gripping, and walking. Each area consists of specific tasks that are scored based on the patient's performance, providing a comprehensive motor function measurement.
Reliability and validity are essential to the MAS, ensuring consistency and accuracy in assessing patients' motor abilities. The scale's reliability indicates its consistency in producing similar scores when administered repeatedly to the same patient. At the same time, validity refers to its ability to accurately measure what it intends to assess.
MAS scores provide valuable information about a patient's motor recovery progress, helping clinicians tailor rehabilitation interventions to address specific needs. By assessing muscle strength, coordination, and control, the MAS assists in identifying areas of improvement and tracking changes over time.
Despite its usefulness, the MAS has limitations, including its focus on motor function assessment and its reliance on the observer's judgment. Additionally, it may not fully capture the nuances of motor recovery, particularly in patients with severe impairments or those affected by factors such as age or comorbidities. However, its responsiveness to changes in motor function makes it a valuable tool in assessing and monitoring patients' progress during rehabilitation.
Scoring
Scoring the Motor Assessment Scale involves assigning numerical values to the patient's performance on specific tasks within each of the eight areas.
Positive indicators include successful completion of tasks with minimal assistance, while negative indicators encompass difficulties or inability to perform tasks independently.
Scores range from 0 to 6 for each item, with higher scores indicating better motor function. The total score is calculated by summing the scores across all areas, providing an overall assessment of the patient's motor abilities.
Clinicians use MAS scores to gauge progress, guide treatment planning, and monitor changes in motor function over time.
What are the next steps?
After completing the Motor Assessment Scale, the following steps typically involve using the assessment results to inform treatment planning and rehabilitation strategies.
Clinicians analyze the MAS scores to identify areas of strength and weakness in the patient's motor function, guiding the development of targeted interventions to address specific needs. These interventions may include physical therapy exercises, occupational therapy techniques, adaptive equipment, or assistive devices to promote motor recovery and enhance functional independence.
Regular reassessment using the MAS helps track progress over time and adjust treatment plans to optimize rehabilitation patients' outcomes.
How does our Motor Assessment Scale template template work?
Our Motor Assessment Scale template by Carepatron provides medical professionals with a user-friendly tool for evaluating patient motor function. Here's a step-by-step guide on how to utilize this template effectively:
Step 1: Access the template
Log in to your Carepatron account and navigate to the MAS template section. Select the appropriate patient profile or create a new one if needed.
Step 2: Complete patient information
Enter relevant patient details such as name, age, medical history, and any pertinent clinical information.
Step 3: Administer the assessment
Follow the instructions provided within the template to administer the Motor Assessment Scale to the patient. Record their performance on each task within the eight areas of motor function.
Step 4: Score the assessment
Use the built-in scoring system to assign numerical values to the patient's performance on each item. The template automatically calculates the total score based on the scores entered for each area.
Step 5: Analyze results
Review the assessment results to identify areas of strength and weakness in the patient's motor function. Use this information to tailor rehabilitation strategies and treatment plans accordingly.
Step 6: Monitor progress
Regularly reassess the patient using the Motor Assessment Scale template to track progress over time. Compare scores from previous assessments to gauge improvement or identify any deterioration in motor function.
Step 7: Collaborate with the care team
Share the assessment results with other patient care team members, including therapists, physicians, and caregivers, to ensure coordinated and comprehensive care.
Benefits of using our template
Our Motor Assessment Scale template by Carepatron offers numerous advantages for medical professionals engaged in assessing and monitoring patients' motor function. Here are five key benefits:
Enhanced reliability and validity
The template ensures consistency and accuracy in assessing motor function, contributing to reliable measurement outcomes. With standardized scoring criteria and clear task instructions, clinicians can confidently assess patients using a validated tool.
Streamlined assessment process
Carepatron's template simplifies the motor assessment process, allowing for efficient administration and scoring. Built-in features automate calculations and scoring, saving time for busy healthcare professionals.
Comprehensive evaluation
The template covers multiple aspects of motor function across eight areas, comprehensively evaluating the patient's abilities. This holistic approach enables clinicians to assess various motor skills, from upper limb function to mobility and gait.
Facilitates research and comparison
By using a standardized assessment tool, clinicians can generate comparable data across patients and settings. This facilitates research efforts to understand motor recovery patterns, treatment outcomes, and disability management strategies.
Tailored rehabilitation planning
The assessment results obtained through the template inform personalized rehabilitation plans tailored to each patient's individual needs. By identifying areas of strength and weakness, clinicians can design targeted interventions to optimize motor function and improve functional outcomes.
Treatment for stroke patients
After a stroke, prompt and comprehensive treatment is essential to minimize brain damage and improve outcomes. Here are several treatment options available for stroke patients:
1. Medications
Depending on the type of stroke, medications such as clot-busting drugs (thrombolytics) or antiplatelet agents may be administered to dissolve blood clots or prevent further clot formation.
2. Rehabilitation therapy
Rehabilitation therapy, including physical therapy, occupational therapy, and speech therapy, plays a crucial role in stroke recovery. These therapies focus on improving motor function, mobility, coordination, speech, and cognitive skills.
3. Surgical interventions
Surgical interventions may sometimes be necessary to remove blood clots, repair damaged blood vessels, or reduce brain swelling. Procedures such as carotid endarterectomy or angioplasty with stenting may be performed to improve blood flow to the brain.
4. Lifestyle modifications
Making lifestyle changes such as adopting a healthy diet, maintaining a regular exercise routine, quitting smoking, and managing conditions like hypertension, diabetes, and high cholesterol can help reduce the risk of recurrent strokes.
5. Supportive care
Stroke patients may require ongoing medical care and support to manage complications such as infections, swallowing difficulties, and depression. Palliative care or hospice services may be provided to improve quality of life for patients with advanced stroke or terminal illness.
Commonly asked questions
The Motor Assessment Scale (MAS) is a standardized tool used to assess motor function in patients recovering from stroke or neurological conditions. It evaluates motor abilities across eight key areas, providing a comprehensive measurement of motor function.
The General Tonus Motor Assessment Scale (GTMAS) is a subset of the MAS, focusing specifically on assessing muscle tone and reflexes in patients with neurological impairments. It evaluates muscle tone, reflexes, and associated reactions to provide insights into neuromuscular function.
Motor Assessment Scale (MAS) is scored based on the patient's performance on specific tasks within each of the eight areas of motor function. Each task is assigned a numerical value ranging from 0 to 6, with higher scores indicating better motor function. The total score is calculated by summing the scores across all areas.