Impaired Urinary Elimination Nursing Diagnosis
Explore essential insights and effective strategies for managing Impaired Urinary Elimination Nursing Diagnosis to enhance patient care and improve outcomes.


What is impaired urinary elimination?
Impaired urinary elimination refers to difficulty or disruptions in the body’s normal process of voiding urine. This condition often affects bladder function and leads to complications like urinary incontinence and urinary retention. This issue can arise from spinal cord injuries, UTIs, bladder dysfunction, medications, pelvic wounds, cognitive impairments, or renal diseases, all impacting bladder function and overall health. When bladder function is compromised, it can result in bladder distention and decreased urine output, often causing significant discomfort and potential risks for urinary tract infection.
Urinary retention is common in these cases, where urine builds up, increasing bladder distention and possibly leading to bladder irritation. Recurrent urinary tract infections can exacerbate symptoms and further impair bladder function. For many patients, impaired urinary elimination calls for a targeted treatment plan involving pelvic floor exercises to strengthen support structures and reduce urinary incontinence. Supporting patients in managing impaired urinary elimination is vital for improving their overall quality of life.
Symptoms of impaired urinary elimination
Impaired urinary elimination can present symptoms that disrupt normal bladder function, impacting patient well-being and daily activities. Recognizing these signs is critical for healthcare professionals to provide timely and effective interventions. Below are some of the most common symptoms associated with impaired urinary elimination:
- Urinary incontinence: Involuntary urinary leakage can range from mild to severe, impacting quality of life.
- Urinary retention: Incomplete bladder emptying, often resulting in frequent, small urine output.
- Bladder distention: Noticeable swelling in the lower abdomen due to accumulated urine in the bladder.
- Frequent urinary tract infections: While also noted as one of the causes, this recurrent infection indicates potential underlying bladder dysfunction.
- Bladder irritation: Symptoms may include pain, burning, or urgency during urination.
- Reduced urine output: A marked decrease in urine produced, signaling potential underlying conditions.
Properly diagnosing impaired urinary elimination, including specific issues like stress urinary incontinence or reflex urinary incontinence, empowers practitioners to improve patient care through evidence-based methods like bladder training.
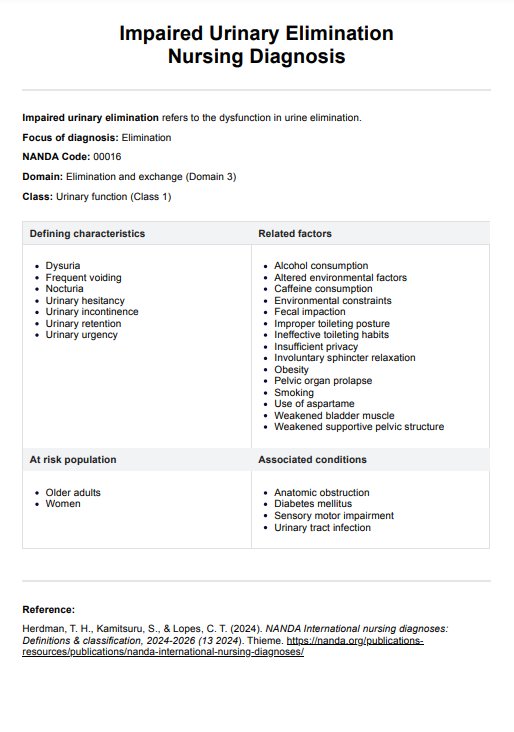
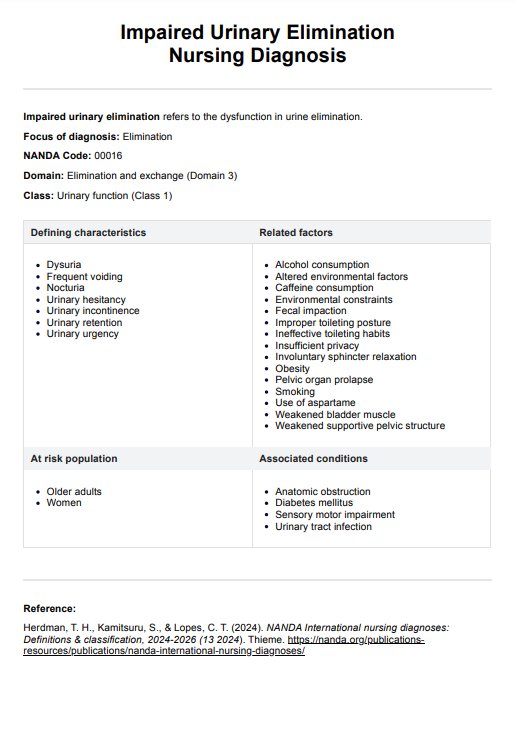
Impaired Urinary Elimination Nursing Diagnosis Template
Impaired Urinary Elimination Nursing Diagnosis Example
How to use our Impaired Urinary Elimination Nursing Diagnosis template
Our Impaired Urinary Elimination Nursing Diagnosis template is a clinical basis for assessing patients with varying urinary conditions, enabling healthcare providers to implement targeted nursing interventions. Below are the essential steps for using the template:
Step 1: Access the template
Begin by clicking “Use Template” on Carepatron to open the template. Our template for the Impaired Urinary Elimination Nursing Diagnosis is based on the NANDA-I guidelines. This ensures nurses follow a standardized framework for identifying, assessing, and managing urinary issues, leading to more consistent and effective patient care (Herdman, Kamitsuru, & Lopes, 2024).
Step 2: Use the nursing diagnosis template
Use the Impaired Urinary Elimination Nursing Diagnosis template as a guide to identify symptoms and contributing factors. This is helpful when documenting the patient’s urinary patterns and history for accurate diagnosis.
Step 3: Plan and implement care interventions
Develop a care plan for treating impaired urinary elimination based on the findings, including strategies like bladder training, medication adjustments, or wound care. Set measurable goals, monitor progress, and make adjustments during follow-ups.
Benefits
The impaired urinary elimination template offers structured support to guide clinical decisions and patient care. Below are key benefits of this template to enhance assessment, treatment planning, and patient outcomes.
Comprehensive symptom tracking
This template facilitates the thorough tracking of symptoms like frequent urination, urinary hesitancy, and bladder distension. Documenting these symptoms aids in identifying the specific type of impaired urinary elimination related to factors like lower abdominal discomfort or urinary infection, helping nurses tailor interventions effectively.
Improved assessment of bladder function
Using the template allows practitioners to systematically assess bladder contractility and bladder emptying, considering factors like decreased urinary output or difficulty initiating urination. This structure supports the accurate identification of issues related to bladder muscles, aiding in diagnosing conditions such as overactive bladder.
Enhanced diagnostic precision
With the help of this guide, nurses can use their clinical judgment of when to use diagnostic tests like urinalysis and bladder scanning to examine renal function and urinary flow.
Individualized care plans
The template aids in developing patient-specific plans by accounting for indwelling catheters, intermittent catheterization, and other unique needs. It ensures care plans address patient-specific issues such as bladder emptying challenges or urinary frequency, optimizing treatment for each individual.
Streamlined monitoring and adjustment
Having the template on hand facilitates an ongoing assessment of symptoms and response to interventions. This is particularly beneficial for managing symptoms of overactive bladder and assessing changes in urine elimination patterns, thus enhancing overall care quality.
Reference
Herdman, T. H., Kamitsuru, S., & Lopes, C. T. (2024). NANDA International nursing diagnoses: Definitions & classification, 2024-2026 (13 2024). Thieme. https://nanda.org/publications-resources/publications/nanda-international-nursing-diagnoses/
Commonly asked questions
Assessment for impaired urinary elimination requires a comprehensive evaluation that includes both subjective and objective data. Key findings may include patient-reported symptoms such as urgency, frequency, nocturia, or incontinence, alongside physical examination results like distended bladder or changes in skin integrity. Additionally, laboratory tests (e.g., urinalysis) can provide insight into possible infections or metabolic issues. A thorough understanding of the patient’s medical history and medication use is also crucial in identifying contributing factors.
Effective nursing interventions for managing impaired urinary elimination may involve both direct and indirect strategies. First, promoting regular toileting schedules can help reduce incontinence episodes. For patients with cognitive impairments, providing reminders or cues can enhance their ability to recognize the need to void. Implementing pelvic floor muscle training or bladder training programs can also be beneficial. Additionally, ensuring adequate fluid intake and assessing the patient's medications for potential side effects that contribute to urinary issues is essential. Collaborating with interdisciplinary teams, including urologists or physical therapists, may further enhance the management plan.
Evaluating the effectiveness of nursing interventions for impaired urinary elimination requires continuous monitoring and reassessment of the patient's condition. This involves tracking the frequency and characteristics of urinary episodes, assessing patient-reported outcomes related to comfort and confidence, and observing any changes in physical examination findings, such as bladder ditension. Documenting these findings allows for clear communication among healthcare providers and aids in adjusting care plans as necessary.