Hemorrhagic Shock Classification Table
Discover our comprehensive guide and free template on Hemorrhagic Shock Classification. Learn about the signs, causes, and treatments of hemorrhagic shock.


What is hemorrhagic shock?
Hemorrhagic shock is a critical medical condition that occurs when a significant and rapid loss of blood volume leads to a decrease in organ perfusion and acute circulatory failure. This type of shock is typically triggered by severe injuries or medical conditions that compromise the integrity of the vascular system, such as traumatic wounds, gastrointestinal bleeding, or ruptured aneurysms.
When the body loses blood rapidly, the remaining blood volume is insufficient to maintain adequate blood flow to organs and tissues. This underperfusion results in a lack of oxygen and nutrients critical for cellular function and survival. The body initially responds to blood loss by constricting blood vessels and increasing heart rate to maintain blood pressure and flow to vital organs. However, if blood loss continues and compensatory mechanisms are overwhelmed, the patient’s condition deteriorates, leading to multiple organ dysfunction.
The rapid onset and progression of hemorrhagic shock is a medical emergency that requires immediate and aggressive intervention. Treatment typically involves stopping the source of bleeding, rapidly replacing lost blood through transfusions, and supporting circulatory function to restore adequate organ perfusion. Timely management is crucial to prevent severe complications associated with hemorrhagic shock, including organ failure and death, highlighting the need for prompt diagnosis and treatment in affected individuals. Clinical evidence in support of transfusion guidelines for high-risk or critically ill patients is more difficult to obtain, and therapy is often guided by clinical judgment.
Signs and symptoms of hemorrhagic shock
The clinical symptoms of hemorrhagic shock can vary depending on the severity of blood loss but typically include:
- Confusion or decreased alertness
- Pale, cold, clammy skin
- Rapid and weak pulse
- Low blood pressure, particularly systolic blood pressure falling below normal ranges
- Shallow, rapid breathing
- Decreased urine output
Causes of hemorrhagic shock
Common causes include:
- Severe traumatic injuries (e.g., from accidents or violent encounters)
- Internal bleeding due to ulcers, ectopic pregnancy, or vascular ruptures
- Surgical complications
- Significant postpartum hemorrhage
Dangers of hemorrhagic shock
Hemorrhagic shock is a severe condition where significant blood loss leads to dangerously low blood pressure, cutting off the oxygen supply to vital organs. Without timely treatment, this lack of oxygen can cause irreversible damage to the brain, heart, and kidneys, potentially leading to organ failure and death. The body's response to compensate for blood loss—such as increased heart rate—can further strain the heart and exacerbate the situation. Therefore, rapid medical intervention is crucial to restore blood volume, stabilize vital signs, and prevent a cascade of life-threatening complications.
Hemorrhagic Shock Classification Table Template
Hemorrhagic Shock Classification Table Example
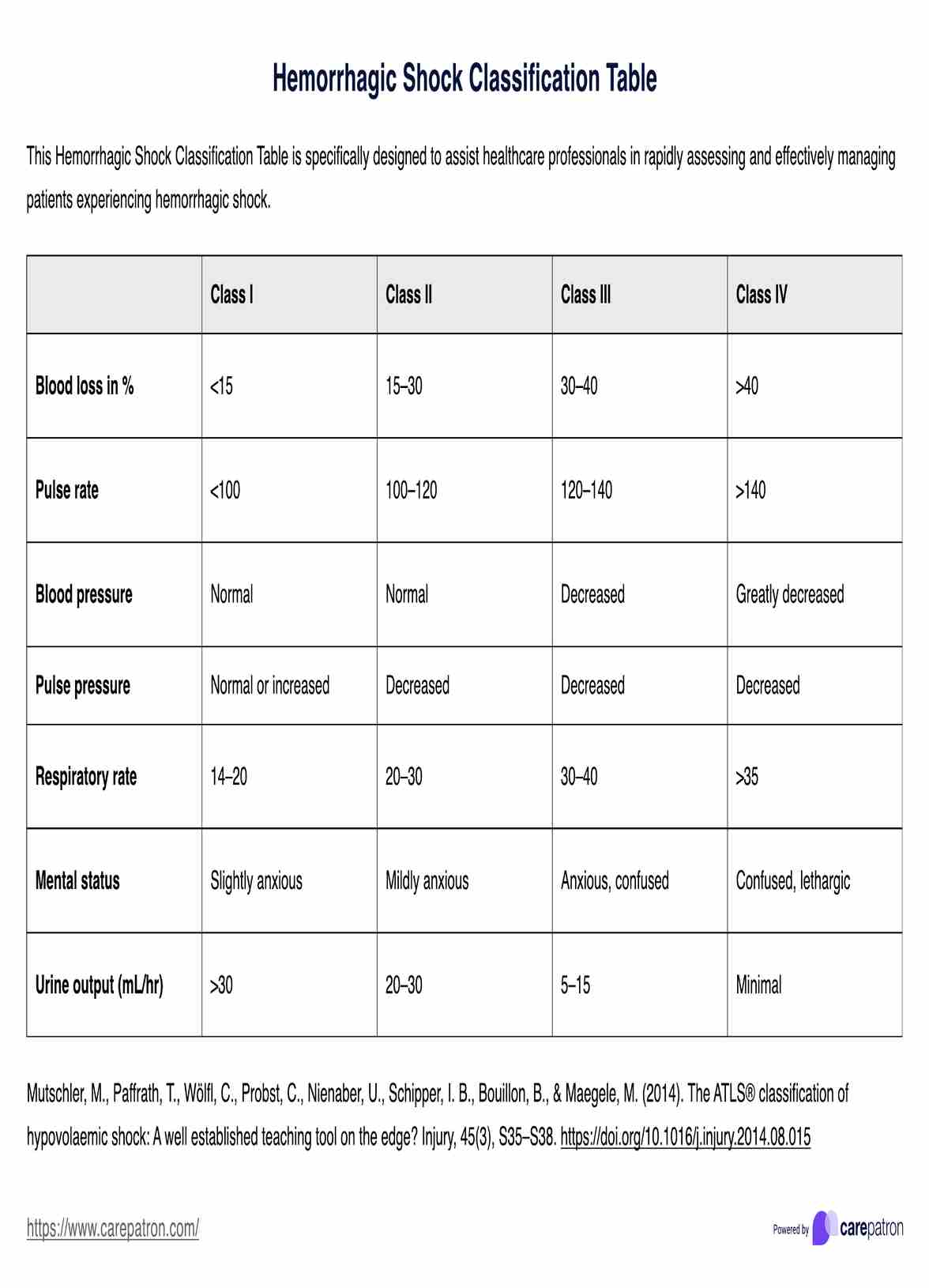
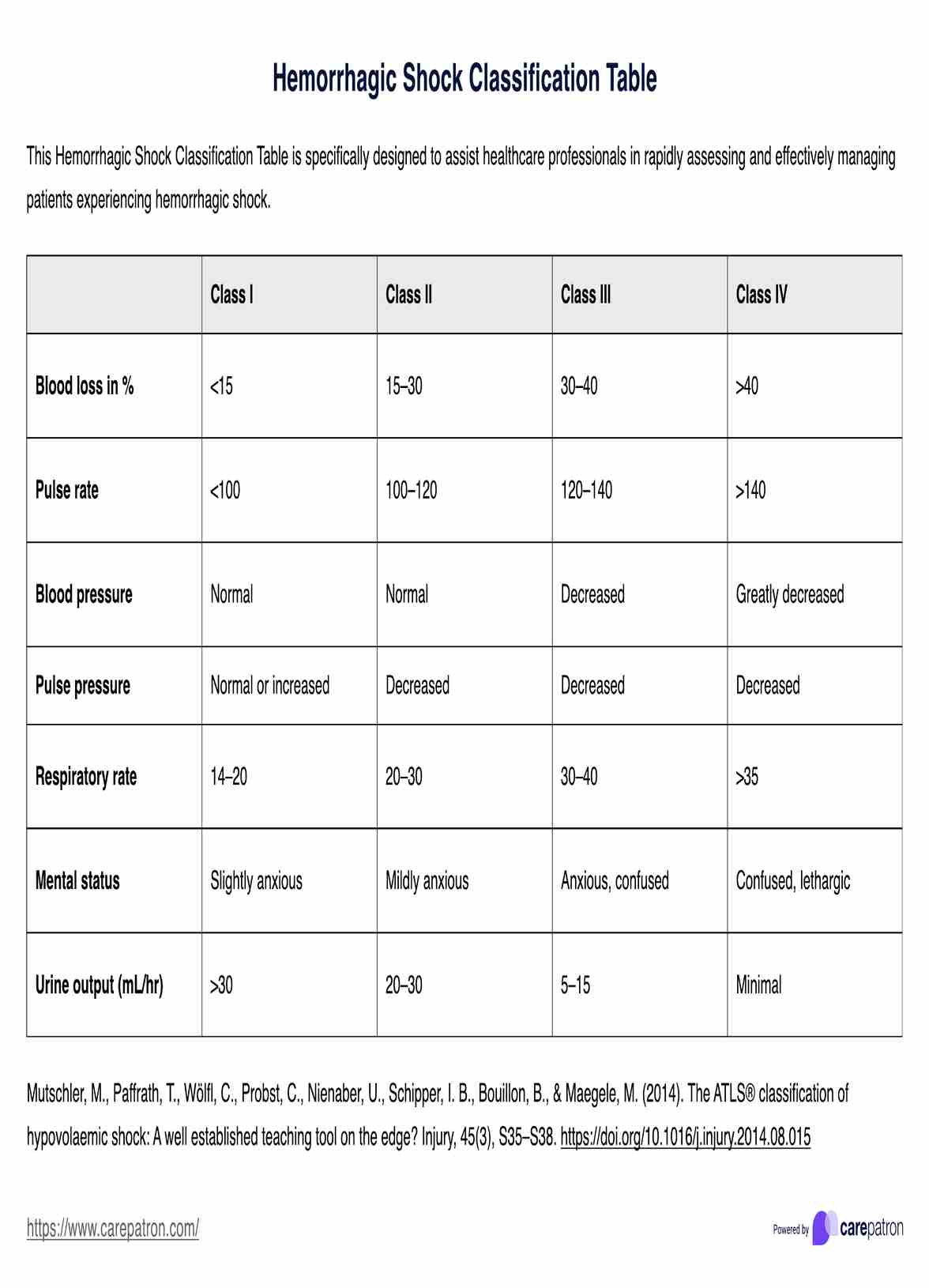
Four classes of hemorrhagic shock
The classification of hemorrhagic shock is generally divided into four classes based on the estimated percentage of total blood volume lost:
- Class I: Up to 15% blood volume loss; often no change in vital signs.
- Class II: 15-30% blood volume loss, tachycardia, and a slight decrease in blood pressure.
- Class III: 30-40% blood volume loss; marked tachycardia, decreased pulse pressure, altered mental status.
- Class IV: Over 40% blood volume loss; severe decreases in blood pressure and perfusion, lethargy, or coma.
What is a Hemorrhagic Shock Classification Table?
A Hemorrhagic Shock Classification Table is an essential clinical tool healthcare providers use to rapidly determine the severity of hemorrhagic shock in patients. This table is structured to facilitate immediate assessment by categorizing shock into four distinct classes based on a combination of clinical and diagnostic criteria. These criteria include blood pressure, heart rate, mental status, and other vital signs for a swift evaluation.
Treatments for hemorrhagic shock and blood transfusions
Effective management of hemorrhagic shock is critical and requires a multi-faceted approach to stabilize the patient and prevent further complications. Treatment strategies include:
- Immediate fluid resuscitation: The prompt administration of fluids, primarily through blood transfusions, is essential to restore circulating blood volume and maintain blood pressure.
- Surgical intervention: For patients with active bleeding, especially from penetrating trauma or severe injuries, surgical intervention is critical to locate and control the source of bleeding.
- Advanced Trauma Life Support (ATLS) Protocols: Implementing ATLS protocols provides a structured approach to the critical care of trauma patients, ensuring that life-threatening conditions are identified and treated swiftly. Predictive models for classifying hypovolemic shock, including those for patients with spinal cord injury, utilize machine learning algorithms and feature selection methods to predict blood loss and determine the ATLS shock class.
- Continuous monitoring and support: Patients in hemorrhagic shock require intensive monitoring in a critical care setting. This involves regular assessment of vital signs, blood oxygen levels, and other physiological parameters to guide ongoing treatment decisions and interventions.
Together, these treatment modalities form a comprehensive response to hemorrhagic shock, optimizing patient outcomes and enhancing recovery.
Commonly asked questions
Monitor blood pressure, heart rate, respiratory rate, and mental status closely.
Immediate treatment is crucial for hemorrhagic shock, especially after significant trauma. Rapid intervention is vital to stabilize blood pressure and control bleeding, following Advanced Trauma Life Support (ATLS) guidelines to prevent severe complications in critically ill patients.
While not all cases are preventable, rapid medical response and appropriate preventive measures in high-risk situations can reduce the incidence.

.jpg)