Fluid and Electrolyte Imbalance Nursing Care Plan
Discover key strategies for managing fluid intake, electrolyte balance, and nursing interventions for imbalances. Download the PDF guide now!


What is fluid and electrolyte imbalance?
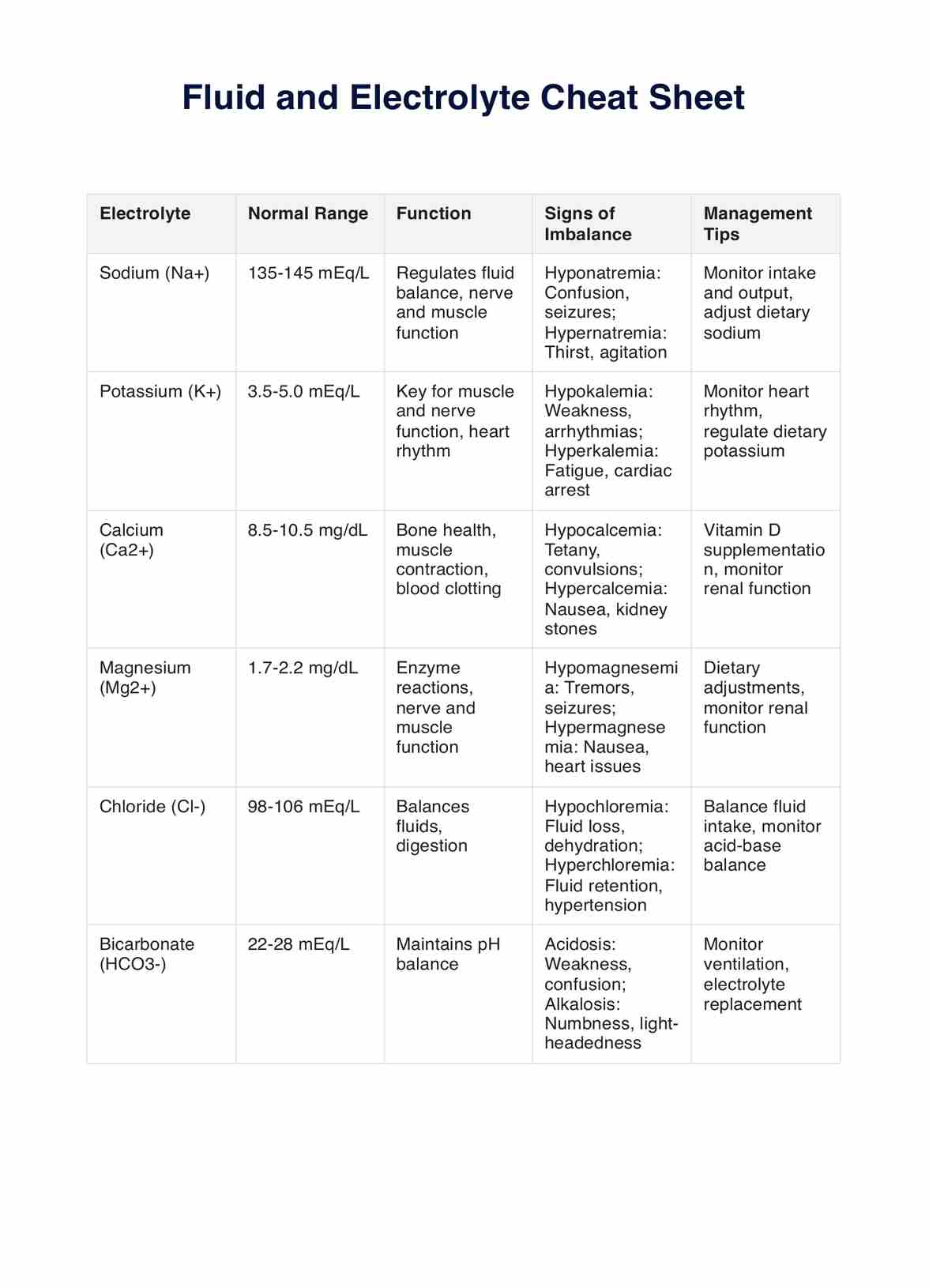
Fluid and electrolyte imbalance occurs when there are significant disruptions in the fluid and electrolyte balance within the body, which is essential for maintaining key physiological functions. Electrolyte imbalances, particularly with sodium, potassium, and calcium, can affect processes such as nerve function, muscle contraction, and blood pressure regulation. Maintaining the correct balance of body fluids, including intracellular fluid, extracellular fluid, and intravascular fluid, is critical to overall health.
Imbalances in these levels often result from conditions like kidney disease, fluid volume excess, fluid volume deficit, dehydration, or excessive fluid intake. In clinical settings, it is vital to quickly identify and address these imbalances to maintain normal electrolyte levels, restore fluid balance, and prevent further complications.
Symptoms of fluid and electrolyte imbalance
Recognizing the signs of fluid and electrolyte imbalances is critical for early intervention and formulating an adequate Fluid and Electrolyte Imbalance Nursing Care Plan. Key symptoms include:
- Altered mental status: Electrolyte disturbances, particularly imbalances that affect brain function, can cause confusion, disorientation, or lethargy.
- Muscle weakness: Imbalances in potassium and calcium levels can result in muscle weakness, cramping, or decreased mobility. Proper electrolyte balance is crucial for muscle function.
- Abnormal heart rhythms: Electrolyte imbalance, such as hypokalemia (low potassium) or hypercalcemia (high calcium), can lead to arrhythmias and palpitations, highlighting the need to monitor serum electrolyte levels.
- Changes in blood pressure: Both excess and deficient fluid volume can lead to fluctuations in blood pressure, which can result in dizziness or syncope. It's essential to monitor blood pressure regularly in patients with suspected imbalances.
- Concentrated urine output: Dehydration or fluid retention related to kidney disease may cause decreased urine output and darker, concentrated urine. It's important to monitor urine output and assess for signs of fluid volume imbalance.
Understanding these symptoms allows for timely nursing interventions such as monitoring fluid intake and oral fluid intake, adjusting sodium intake, and tracking vital signs. Implementing an appropriate electrolyte imbalance nursing diagnosis is key to providing the best care for patients and preventing complications associated with excess or deficient fluid volume.
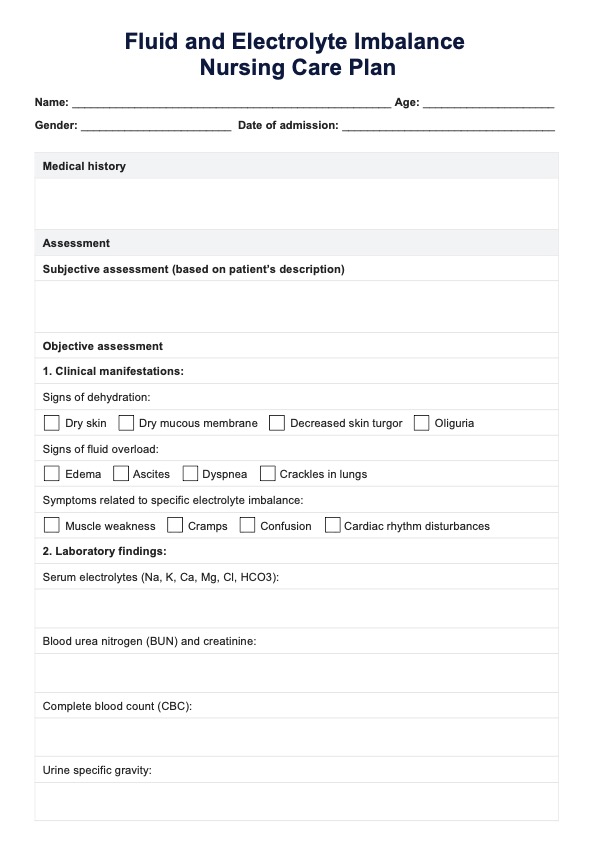
Fluid and Electrolyte Imbalance Nursing Care Plan Template
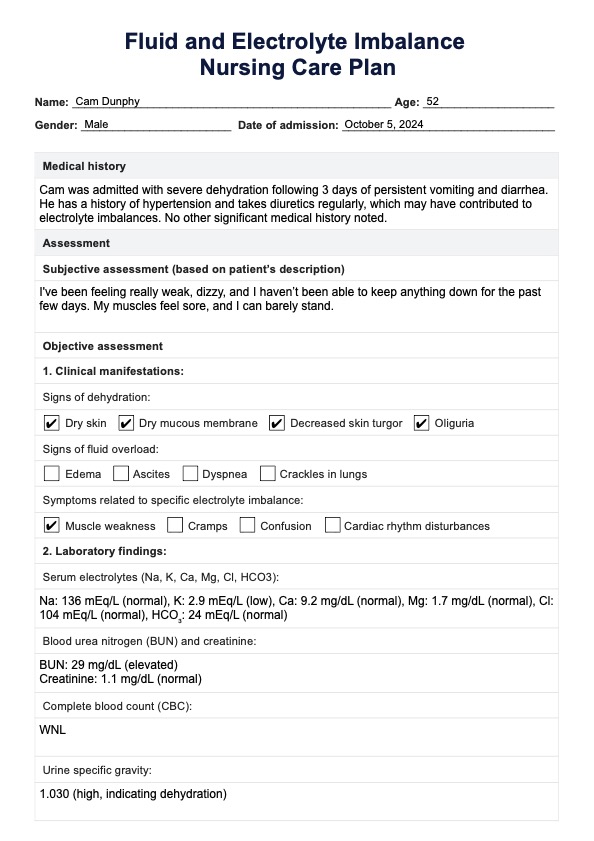
Fluid and Electrolyte Imbalance Nursing Care Plan Example
How does this template work
Follow these five steps to effectively use the Fluid and Electrolyte Imbalance Nursing Care Plan template to assess, monitor, and manage patients experiencing fluid and electrolyte imbalances:
Step 1: Assess the patient’s fluid and electrolyte status
Begin by thoroughly assessing the patient’s fluid and electrolyte balance, including fluid intake, signs of fluid volume excess or deficient fluid volume, and electrolyte levels. Evaluate for signs and symptoms of electrolyte imbalances, such as muscle weakness, abnormal blood pressure, fluid retention, or concentrated urine.
Monitoring vital signs, urine output, and body fluids (such as intracellular and extracellular fluid) will help determine the patient’s overall fluid status.
Step 2: Develop an electrolyte imbalance nursing diagnosis
Based on the assessment, a specific electrolyte imbalance nursing diagnosis must be established. Determine whether the patient is experiencing fluid volume deficits, excess fluid, or an electrolyte imbalance (e.g., sodium intake imbalances or potassium issues).
This step is crucial for addressing electrolyte disturbances and tailoring the care plan to the patient's condition.
Step 3: Establish goals and outcomes
Ensure that the goals and outcomes of the care plan are measurable, patient-centered, and realistic. The goals and outcomes should also be specific to the type of electrolyte imbalance identified in Step 2.
For example, if the patient has a fluid volume deficit, a goal could be to increase their fluid intake by a certain amount per day. If they have an excess of sodium or potassium, the goal may be to decrease their intake of these electrolytes.
Step 4: Implement nursing interventions
Carry out targeted nursing interventions based on the diagnosis. This may include managing fluid intake, adjusting sodium intake, administering intravenous fluids, and monitoring the patient’s respiratory rate for signs of fluid retention or fluid volume excess. Make sure each intervention is guided by a rationale
Ensure that the patient’s electrolyte balance is maintained by tracking their hydrogen ion concentration and monitoring for any complications related to kidney disease.
Step 5: Reassess and adjust the care plan
Regularly evaluate the patient's fluid and electrolyte status, tracking changes in electrolyte levels, vital signs, and fluid volume. Adjust the nursing care plan as needed to respond to improvements or worsening conditions, ensuring that normal electrolyte levels are maintained and fluid volume deficits or excesses are corrected promptly.
Benefits of using a Fluid and Electrolyte Imbalance Nursing Care Plan
A Fluid and Electrolyte Imbalance Nursing Care Plan is essential to ensure timely and effective management of fluid and electrolyte imbalances. This structured approach allows for accurate assessment, targeted nursing interventions, and continuous monitoring, ultimately promoting fluid balance and preventing complications. These are the benefits:
1. Facilitates systematic assessment and intervention
A comprehensive care plan provides a structured framework for nurses to assess fluid and electrolyte status systematically. Following a standardized approach, nurses can efficiently gather relevant data, identify risk factors, and develop appropriate interventions tailored to the patient's needs.
2. Promotes early detection of imbalances
A designated care plan enables nurses to monitor blood pressure and promptly recognize signs and symptoms of fluid and electrolyte imbalances. Early detection allows for timely intervention, preventing complications such as dehydration, electrolyte disturbances, and cardiac abnormalities.
3. Enhances patient outcomes through individualized care
A personalized care plan ensures interventions are tailored to address each patient's needs and preferences. By considering factors such as medical history, comorbidities, and lifestyle factors, nurses can deliver individualized care that maximizes the effectiveness of treatment and promotes positive outcomes.
4. Improves communication and continuity of care
A documented care plan serves as a communication tool among healthcare team members, facilitating collaboration and ensuring continuity of care. By documenting assessments, interventions, and outcomes, nurses can communicate the patient's progress and response to treatment, promoting coordinated care delivery.
Commonly asked questions
Developing a nursing care plan for fluid retention and electrolyte imbalance can take anywhere from 30 minutes to several hours, depending on the complexity of the patient's condition, required assessments, and individualized interventions.
You can monitor fluid intake by accurately tracking oral and intravenous fluids administered. Document all intake amounts, assess urine output and adjust the care plan based on changes in fluid balance and vital signs.
Common signs and symptoms of electrolyte imbalances include muscle weakness, cramps, fatigue, irregular heartbeats, changes in mental status, and abnormal blood pressure. In severe cases, cardiac arrhythmias or seizures may occur.