Breastfeeding Care Plan Chart
Learn how a Breastfeeding Care Plan Chart helps mothers and babies with structured guidance, addressing challenges, and promoting successful breastfeeding.


How does a breastfeeding care plan work?
A breastfeeding care plan is designed to support the mother and her infant's breastfeeding journey by providing structured guidance and addressing potential challenges. It's tailored to fit individual needs and circumstances but typically involves several key elements:
1. Assessment
The nursing care plan often begins with a thorough assessment of the mother and the baby. This includes medical histories, current health status, and any breastfeeding issues they may face. The lactation consultant or healthcare provider may observe a feeding session to assess the baby's latch, the mother's comfort, and the feeding positions.
2. Setting objectives
The objectives of the care plan are set based on the initial assessment. Goals include achieving a pain-free latch, establishing a regular feeding schedule, gaining appropriate weight, or increasing milk supply. These goals are specific, measurable, achievable, relevant, and time-bound (SMART).
3. Implementation
The care plan outlines specific strategies and actions to meet the set objectives. This can include:
- Education on breastfeeding techniques: Teaching the mother different positions for breastfeeding can make the process easier and more effective.
- Schedule and feeding frequency recommendations: Advising how often to feed the baby based on age and needs can help establish a routine and maintain milk supply.
- Management of breastfeeding problems: Providing solutions for common issues like sore nipples, engorgement, and blocked ducts.
4. Support mechanisms
The plan should include support resources such as access to a lactation consultant, links to local breastfeeding support groups, and information on online forums. This ensures that the mother feels supported and can get help when needed.
5. Monitoring and adjustment
Regular follow-up appointments are scheduled to monitor the progress of the mother and baby. During these check-ups, the care plan can be adjusted based on their current needs and challenges. This might involve tweaking feeding techniques, addressing new issues, or reassessing goals.
6. Documentation
Keeping detailed records of feeding times, durations, and any issues encountered is crucial. This documentation helps track progress and identify patterns or recurring issues.
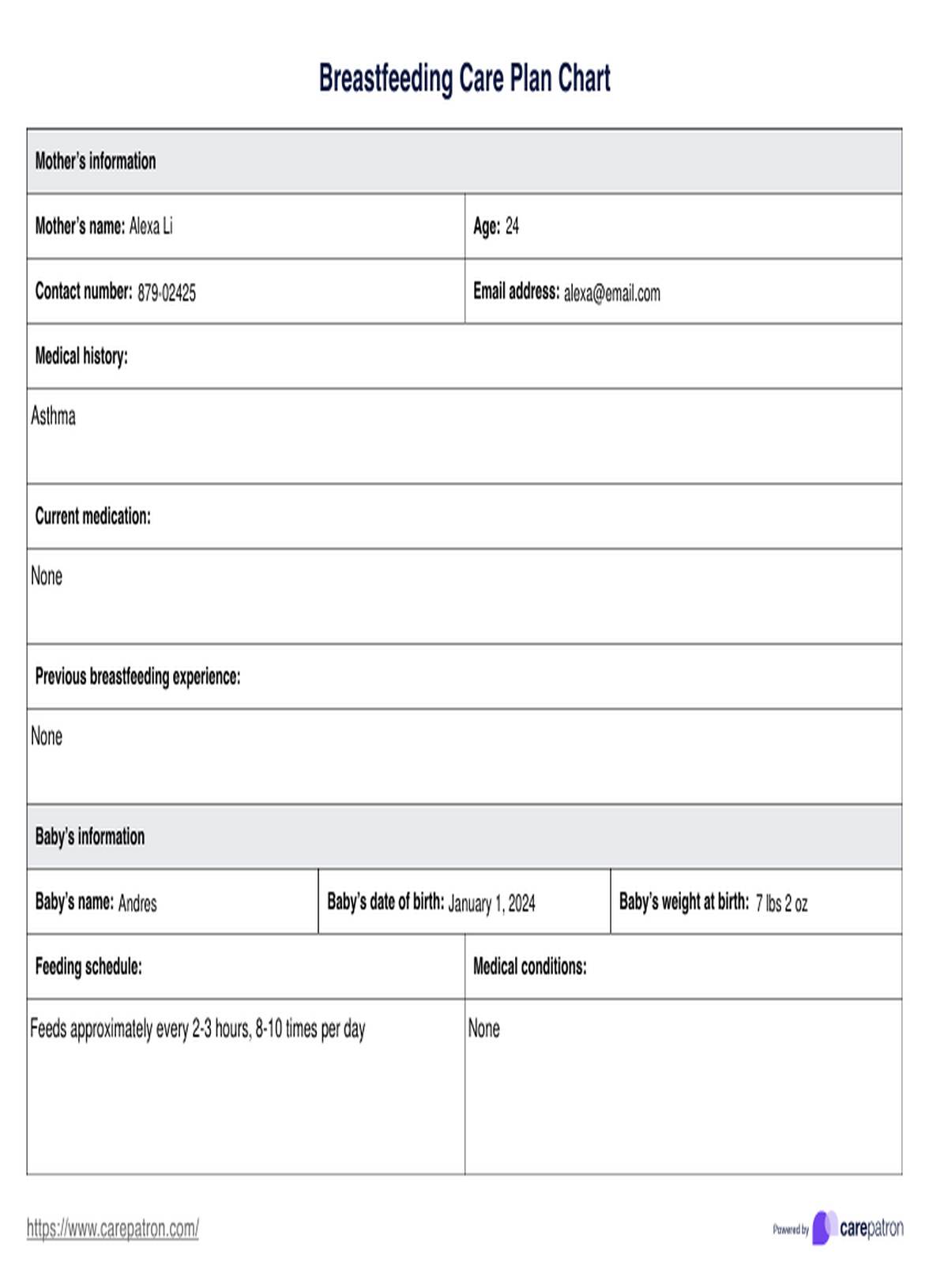
Breastfeeding Care Plan Chart Template
Breastfeeding Care Plan Chart Example
When does breast milk supply begin?
Breast milk supply typically begins to develop during pregnancy, with the breasts starting to produce colostrum, the first form of milk, as early as the second trimester. However, the most significant changes affecting breast milk amount occur later in pregnancy and immediately following birth. Colostrum is produced in small amounts during the last few months of pregnancy and continues to be produced for the first few days after the baby's birth.
The transition from colostrum to mature milk begins around the second to fifth day postpartum. This change is often called when the milk "comes in." During this time, the breasts may feel fuller and heavier as milk production increases significantly.
This mature milk provides the primary source of nutrition for the infant moving forward. The milk production process is largely driven by the hormone prolactin and the demand created by the baby’s feeding, which stimulates further production.
Common causes of inadequate milk supply
Inadequate milk supply is a common concern among breastfeeding mothers. Understanding various risk factors can contribute to this situation and help address and manage the issue effectively. Here are some of the common causes of low milk supply:
- Infrequent feeding or pumping: Breast milk production is largely driven by demand. Less frequent breastfeeding or pumping can lead to reduced milk production as the body adjusts to the perceived lower demand.
- Poor latch: If babies do not latch properly, they may not effectively remove milk from the breast. This ineffective milk removal can signal the body to produce less milk.
- Maternal health issues: Conditions such as retained placenta fragments, hormonal imbalances (like thyroid disorders or polycystic ovary syndrome), previous breast surgery, or certain medications can negatively impact milk production.
- Use of certain medications: Some medications, including hormonal contraceptives that contain estrogen, can decrease milk supply. Breastfeeding mothers need to discuss any medications they are taking with their healthcare provider.
- Insufficient glandular tissue: Some women have insufficient glandular tissue in their breasts, limiting the amount of milk produced.
- Stress and fatigue: Emotional and physical fatigue can impact the body’s ability to produce milk. High stress levels can interfere with the release of oxytocin, a hormone that helps with the milk ejection reflex.
- Poor diet and dehydration: Adequate hydration and nutrition are crucial for optimal milk production. A diet lacking sufficient calories or fluids can lower milk supply.
- Smoking: Smoking has been shown to reduce milk production and can also alter the composition of breast milk.
Addressing these issues often involves a combination of medical evaluation, improved breastfeeding techniques, lifestyle adjustments, and, in some cases, using supplements or medications to help enhance milk production.
Consulting with a lactation consultant or healthcare provider can provide tailored guidance and emotional support to overcome challenges related to low milk supply.
Does skin-to-skin contact impact milk production?
Yes, skin-to-skin contact, known as kangaroo care, can positively impact breastfeeding production. This practice involves holding the baby close to the skin, offering several benefits that promote and enhance breastfeeding.
Some of the ways skin-to-skin contact can affect milk production:
- Stimulation of hormones: Skin-to-skin contact helps increase the oxytocin levels in the mother's body. Oxytocin is a critical hormone in milk ejection reflex (let-down) and milk production. The physical closeness and sensory interaction with the baby stimulate the release of this hormone, which in turn helps milk flow more freely.
- Increased breastfeeding success: Babies held skin-to-skin are more likely to latch on to the breast correctly and breastfeed effectively. Effective breastfeeding encourages the breasts to produce more milk.
- Reduction of stress: Skin-to-skin contact can reduce stress and anxiety in both the mother and the baby. Lower stress levels in mothers can lead to better milk production, as stress can inhibit the production of necessary hormones like prolactin and oxytocin.
- Regulation of baby’s behavior: Babies who are held skin-to-skin often cry less and are more stable regarding their heart rate and temperature. This calm state can make it easier for babies to feed and for mothers to produce a steady milk supply.
- Increased feeding opportunities: Skin-to-skin contact keeps the baby close to the mother’s breasts, which can lead to more frequent feedings. Increased feeding signals the body to increase milk production.
Incorporating skin-to-skin contact into routine care after birth and the early postpartum period is highly encouraged as it supports breastfeeding, enhances maternal-infant bonding, and provides numerous other health benefits for both mother and baby.
How to use the chart during the breastfeeding process
Using a Breastfeeding Care Plan Chart effectively during the breastfeeding process can help ensure that both mother and baby receive the support and monitoring necessary for successful breastfeeding. Here’s how medical practitioners and mothers can use such a chart:
Nursing interventions for ineffective breastfeeding
When addressing ineffective breastfeeding in pregnant women, several nursing interventions can be crucial in helping both the mother and the infant establish more successful breastfeeding practices. Targeted interventions to consider:
Initial assessment
Use the template to assessment the mother and the child. Document the mother and the child's medical history, the child's feeding schedule as well as any details relevant to feeding assessment. This initial assessment will help identify any potential breastfeeding issues and allow for early intervention.
Set goals and interventions
Use the chart to document breastfeeding goals and care interventions to help the mother and child achieve successful breastfeeding. This can include information about proper latching techniques, frequency of feedings, positions for breastfeeding, and any issues or concerns that arise during the process.
Include support resources
The chart should also include resources for support, such as contact information for lactation consultants or breastfeeding support groups. This can help mothers address any challenges they may face during the breastfeeding process and ensure they have access to additional support when needed.
Track progress
You can also use the chart to monitor the mother and child's progress throughout their breastfeeding journey. Utilize the Progress Tracking section to jot down notes about the mother and child's progess and additional remarks on any improvements or challenges. This can help identify patterns and track the success of interventions.
Commonly asked questions
The World Health Organization recommends exclusive breastfeeding for the first six months of life, followed by continued breastfeeding and appropriate complementary foods up to two years of age or beyond.
No, breastfeeding does not inherently lead to poor weight gain. Breastfed babies typically gain weight steadily as breast milk provides all the necessary nutrients in the right amounts. Any concerns about weight gain should be discussed with a pediatrician.
Yes, exclusive breastfeeding is highly beneficial. It provides all the necessary nutrition a baby needs in the first six months of life, supports immune system development, and promotes a healthy bond between mother and baby.