Healthcare professionals, particularly neurologists and physical therapists, use the Modified Ashworth Scale to assess muscle spasticity in patients.
Modified Ashworth Scale
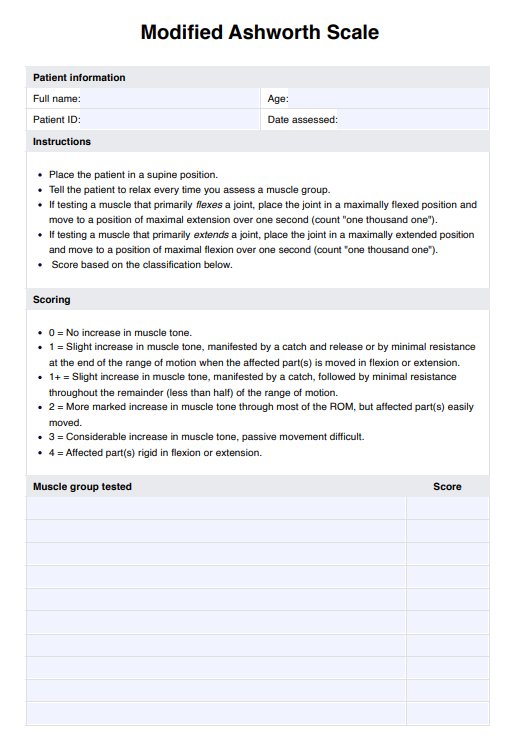
Use the Modified Ashworth Scale to measure the muscle tone of your patients with neurological problems and to measure the progress of spasticity.
Modified Ashworth Scale Template
Commonly asked questions
An assessment using the Modified Ashworth Scale typically takes a few minutes or longer, depending on the muscle group evaluated.
The examiner passively moves the patient's limb through its range of motion and grades the resistance felt during this movement. The perceived resistance is then scored according to the Modified Ashworth scale, with a score of 0 representing no increase in muscle tone and a score of 4 indicating that the limb is rigid in flexion or extension.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











