Clinical notes are essential documentation in healthcare that can take various forms, including SOAP notes, DAP notes, and BIRP notes. SOAP notes organize information into four categories: Subjective, Objective, Assessment, and Plan, making them widely used for documenting patient encounters. DAP notes focus on Data, Assessment, and Plan, providing a more concise format. BIRP notes are particularly useful in behavioral health settings and emphasize Behavior, Intervention, Response, and Plan. Each type serves specific purposes based on the patient's condition and treatment context.
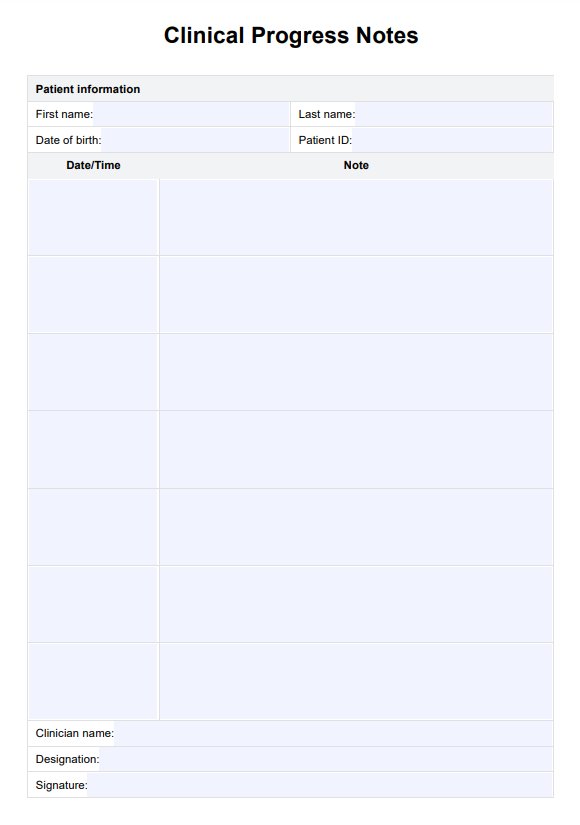
Clinical Progress Notes Template
Streamline your documentation with our Clinical Progress Notes Template in an easy-to-use PDF format.
Clinical Progress Notes Template Template
Commonly asked questions
Clinical notes in medical records are detailed accounts of patient interactions that document vital information such as the patient's medical history, symptoms, diagnoses, treatment plans, and follow-up care. These notes serve as a communication tool among healthcare providers, ensuring continuity of care and supporting clinical decision-making.
To write a clinical progress note, include essential details such as the date of service, patient identification information, and session duration. Use a structured format like SOAP or BIRP to organize your observations: document the patient's subjective experiences, the objective findings from your examination or assessment, your assessment of the patient's condition based on this information, and your plan for future treatment or interventions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











