Progress Notes For Psychotherapy Template
Our psychotherapy progress note template will streamline your workflow, create efficient notes faster, and enhance the quality of your care without compromise.


What are progress notes?
Progress notes are detailed written records documenting a client's progress, treatment interventions, and overall care plan. They are a crucial communication tool among healthcare providers to ensure continuity of care and informed decision-making. Beyond that, they are also a measure of accountability and help practitioners become more organized in clinical work.
Mental health progress notes
In the broader field of mental health, progress notes serve as a guide and roadmap through the client's treatment, including their symptoms, behaviors, and responses to various interventions. These progress notes help mental health professionals coordinate care and make informed decisions about the client's treatment plan.
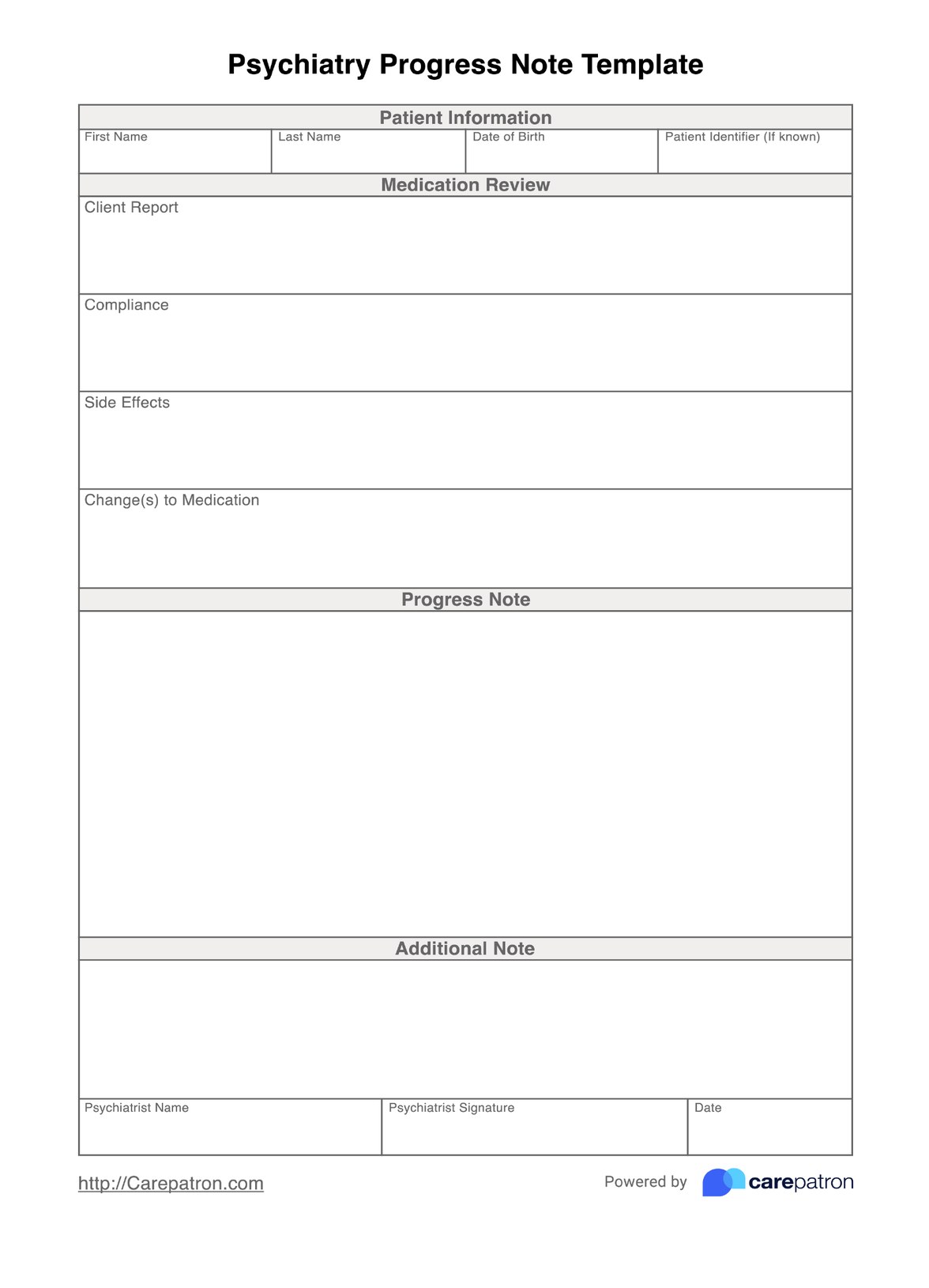
Progress notes in mental health settings may also include information about medication management, risk assessments, and coordination with other healthcare providers.
Progress notes in psychotherapy
Psychotherapy progress notes document a client's journey through treatment. A therapy progress note typically includes the client's presenting concerns, relevant background information, therapeutic interventions employed, the client's responses and client progress, and recommendations for future sessions (Tudor & Gledhill, 2022).
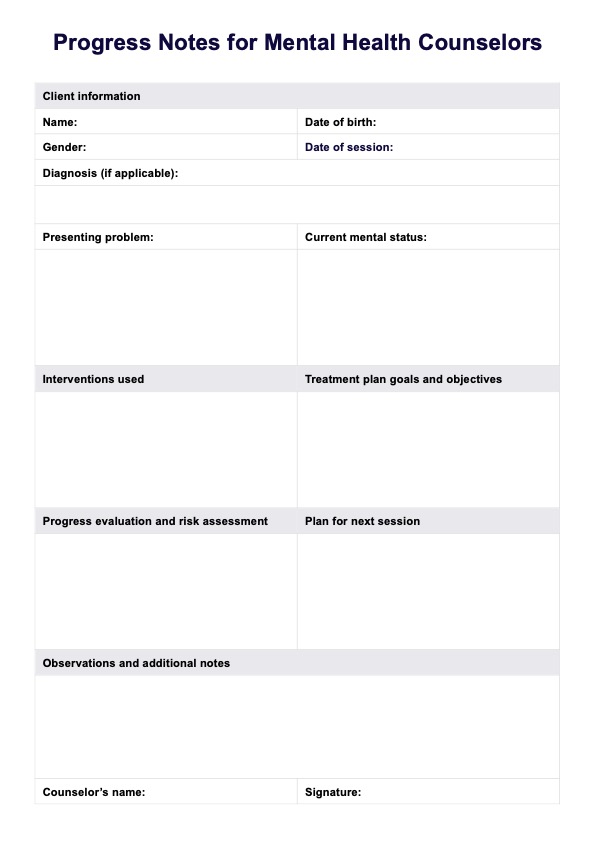
Counseling progress notes
Counseling progress notes, on the other hand, record the client's concerns, goals, and progress throughout the counseling process. For instance, a counseling note template typically includes the topics discussed during sessions, the client's responses and insights, and the counselor's observations and interventions.
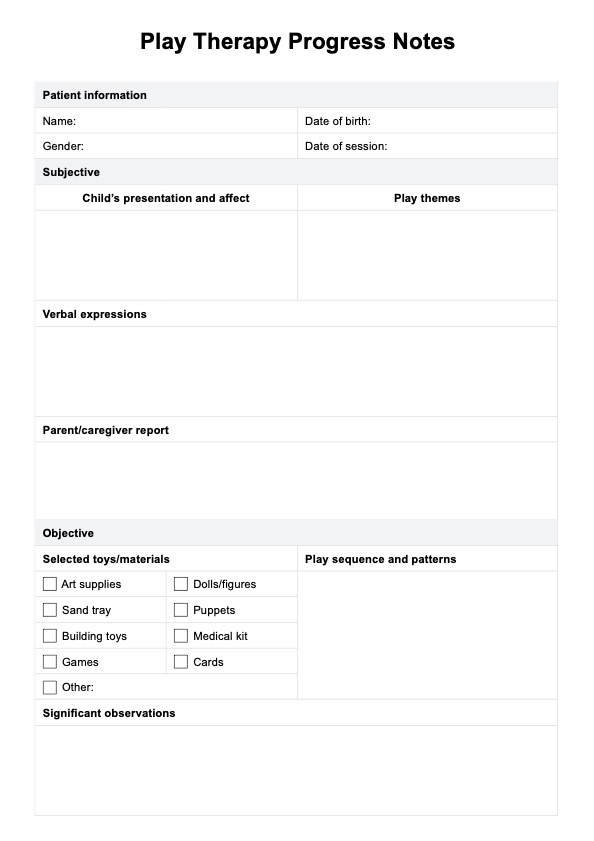
Group therapy progress notes
Progress notes in group therapy document the dynamics and interactions within the group and the progress of individual members. These notes typically include information about the group's focus, the topics discussed, the interventions used, and the responses and progress of individual members.
Group therapy notes help facilitators identify areas requiring further attention and ensure that the group's goals and objectives are met.
Progress notes are also used in various other mental health professions, such as social work, marriage and family therapy, and substance abuse treatment.
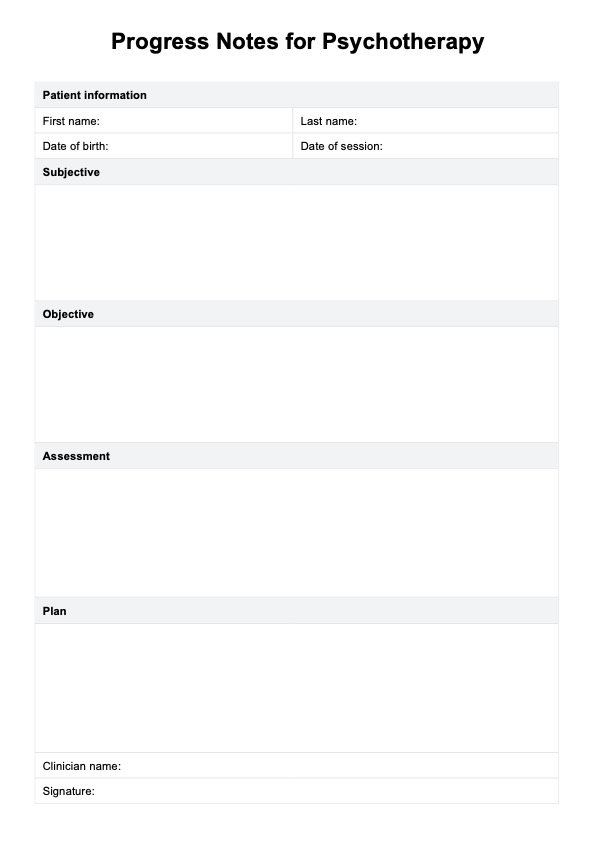
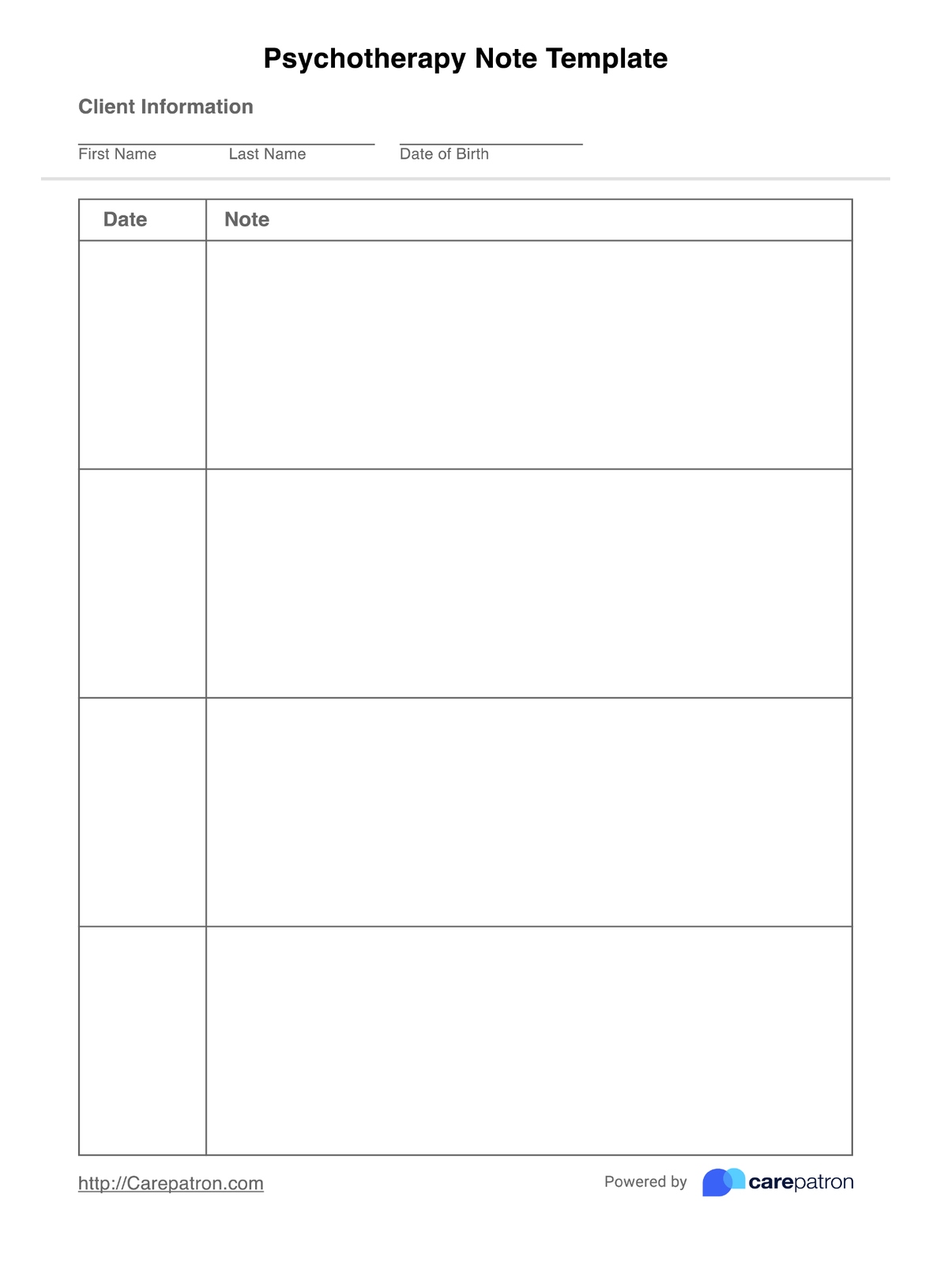
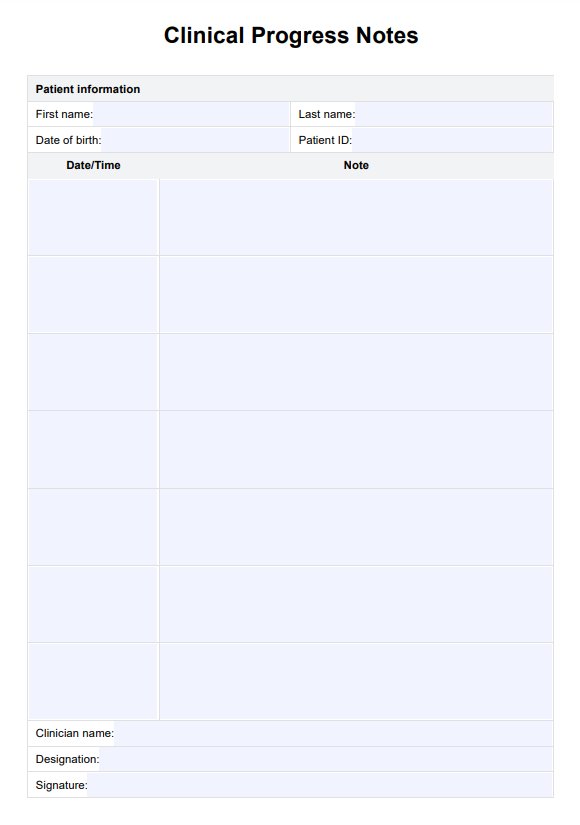
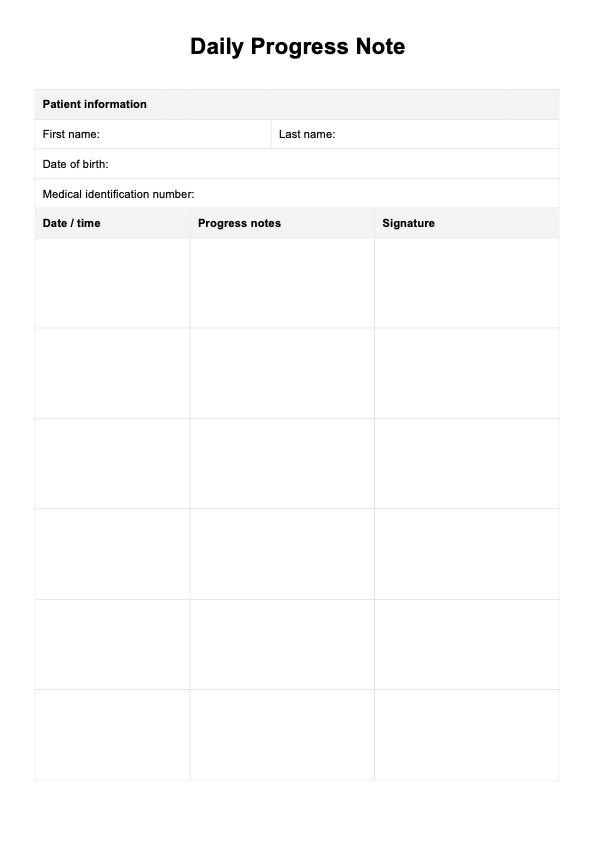
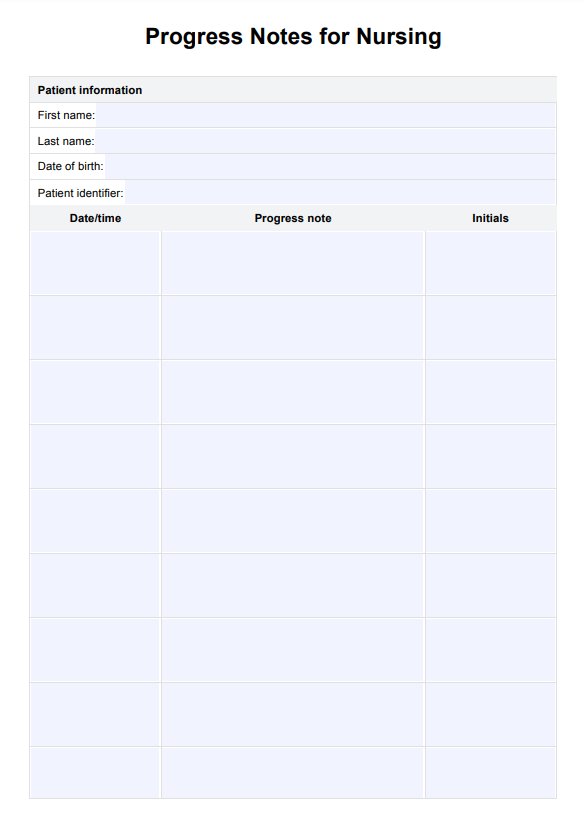
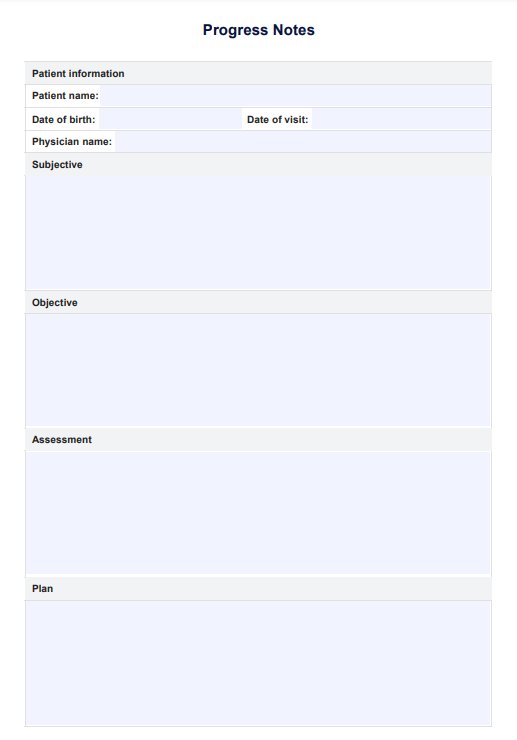
Progress Notes For Psychotherapy Template
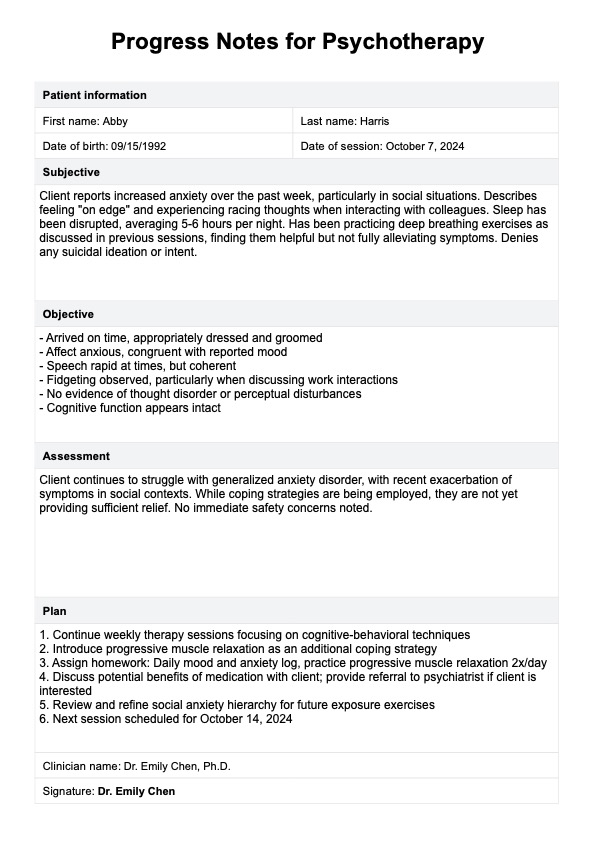
Progress Notes For Psychotherapy Template Example
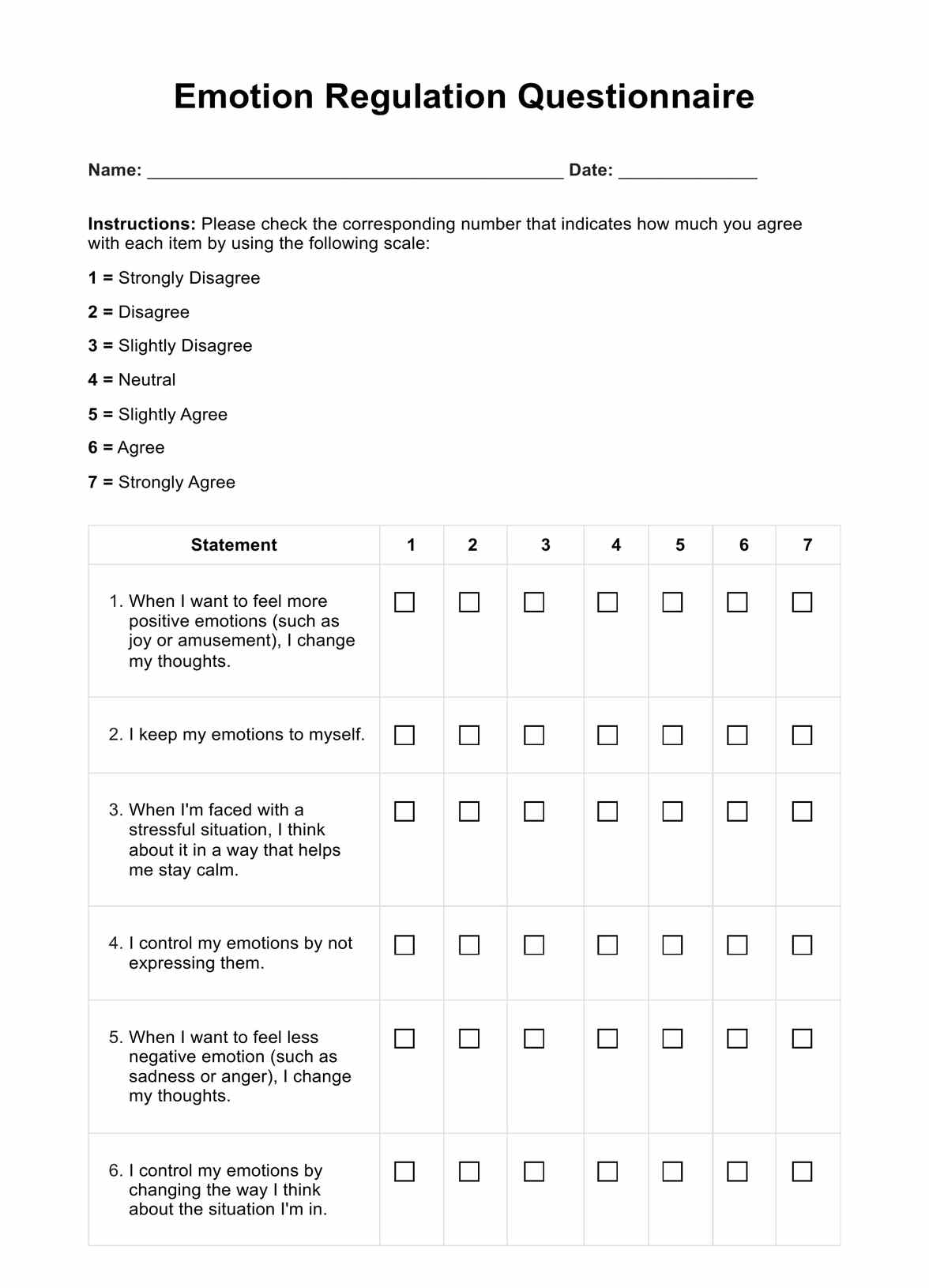
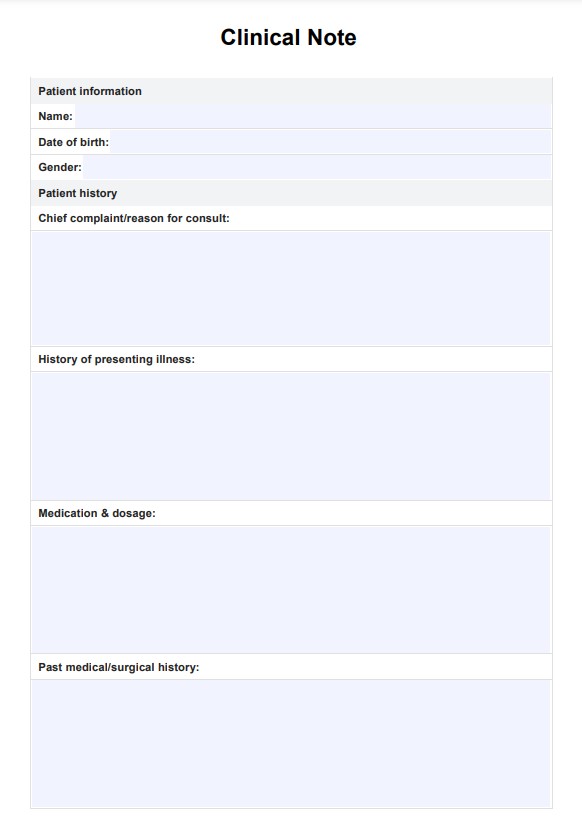
What should be included in progress note templates?
Effective progress notes typically include the following components:
- Client information: Basic details such as the client's name, date of birth, and session date. This ensures proper identification and helps maintain an organized record.
- Session type: Specifies whether it's an individual, group, or family therapy session. This contextualizes the information that follows.
- Presenting issues: A brief description of the primary concerns or symptoms the client is experiencing. This helps track the focus of treatment over time.
- Interventions used: Specific therapeutic techniques or strategies employed during the session. This documents the therapist's approach and allows for the evaluation of treatment effectiveness.
- Client's response: How the client reacted to the interventions or engaged in the session. This helps gauge the client's progress and the appropriateness of the chosen interventions.
- Assessment: The therapist's professional evaluation of the client's current status, including any changes in symptoms or functioning. This component synthesizes the session's information.
- Plan: Outlines the next steps in treatment, including future session goals, homework assignments, or referrals. This ensures continuity of care and guides future sessions.
- Risk assessment: This is a documentation of any potential risks or safety concerns, such as suicidal ideation or self-harm behaviors.
How to use this psychotherapy note template
Here's a step-by-step guide on how to use our template to help you write progress notes.
Step 1: Fill in patient information
Begin by entering the patient's basic details, including their first and last name, date of birth, and the date of the current session. This ensures proper identification and helps maintain an organized record of each encounter.
Step 2: Document session content
The template follows the widely used SOAP note format, which stands for Subjective, Objective, Assessment, and Plan. Record the patient's self-reported experiences, symptoms, and concerns. Note your observations of the patient's behavior, affect, and any measurable data. Provide your professional evaluation of the patient's current status and progress. Finally, outline the treatment plan, including future goals and interventions.
Step 3: Review and finalize
Take a moment to review the entire note for accuracy and completeness. Ensure that all relevant information has been captured and that the note provides a clear picture of the session and treatment direction.
Step 4: Sign the document
Complete the note by entering your name and signature. This step validates the note as an official record and meets legal and ethical documentation requirements.
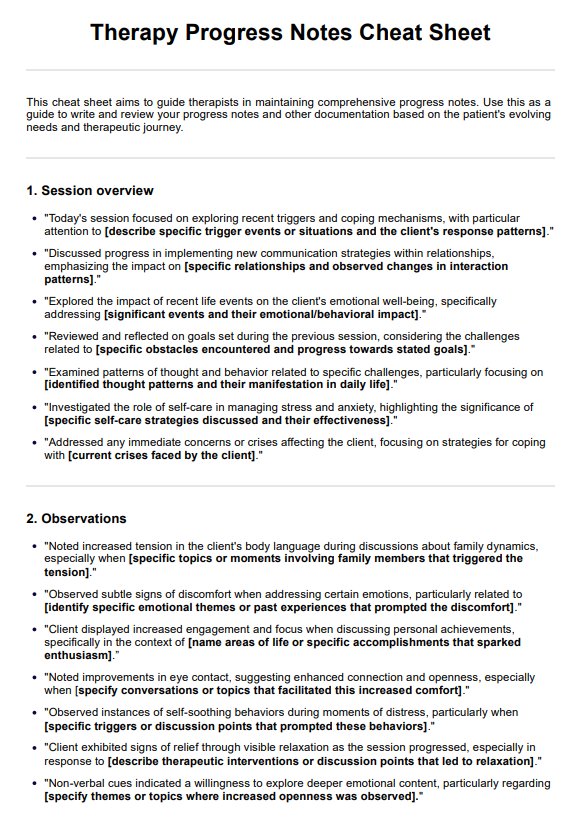
Progress notes formats you can use
There are several commonly used formats for clinical documentation. Each format has its own structure and emphasis, allowing practitioners to document relevant information in an organized and efficient manner. Since this template uses the SOAP format, here are some of the other widely used formats that you can use when writing therapy progress notes:
BIRP notes
BIRP stands for Behavior, Intervention, Response, and Plan. The BIRP format focuses on documenting the client's observed behaviors (Behavior), the therapeutic interventions employed (Intervention), the client's response to those interventions (Response), and the planned next steps or future interventions (Plan).
DAP notes
DAP notes consist of the Data, Assessment, and Plan sections. The Data section includes subjective and objective information about the client's presentation and reported experiences. The Assessment section includes the therapist's analysis and evaluation, while the Plan section outlines the proposed treatment goals and interventions.
Narrative notes
Narrative notes are written in a free-flowing, descriptive format without a specific structure. These notes provide a detailed account of the session, including the client's behavior, their statements, the therapist's observations, interventions used, and the client's responses. Narrative notes allow for more flexibility in documenting the therapeutic process.
Benefits of using this template
Implementing a structured progress notes template in psychotherapy practice offers numerous advantages that enhance both patient care and professional efficiency. Here are some key benefits:
Consistency in documentation
A standardized template ensures that essential information is captured consistently across all patient encounters. This uniformity makes it easier to track progress over time and facilitates better communication among healthcare providers.
Time efficiency
With a pre-structured format, clinicians can focus on filling in relevant information rather than spending time deciding what to include. This streamlined approach can significantly reduce the time spent on documentation, allowing more focus on patient care.
Improved clarity and readability
The organized format of a template enhances the clarity and readability of notes. This is particularly beneficial when reviewing past sessions or when other healthcare professionals need to quickly understand a patient's history and treatment progress.
Legal and ethical compliance
Well-structured progress notes serve as a legal record of patient care. Using a comprehensive template helps ensure that all necessary elements are included, meeting legal and ethical documentation standards.
Reference
Tudor, K., & Gledhill, K. (2022). Notes on notes: Note-taking and record-keeping in psychotherapy. Journal of Psychotherapy Aotearoa New Zealand, 26(2), 123–144. https://doi.org/10.9791/ajpanz.2022.12
Commonly asked questions
A psychotherapy note is a detailed record of a patient's psychotherapy session, including the patient's symptoms, treatment goals, and progress. It should include the date and time of the session, the patient's attendance and participation, and any notable events or behaviors. The note should also document the therapist's observations, impressions, and any relevant psychological or medical information.
A psychotherapy note is a detailed record of a patient's psychotherapy session, while a progress note summarizes the patient's overall progress and treatment plan. Psychotherapy notes are typically more detailed and focused on the specific session, while an individual progress note provides a broader overview of the patient's treatment and progress. Unlike progress notes, psychotherapy notes are kept confidential and not shared with other healthcare providers.
To write effective counseling notes, identify the key issues and goals discussed during the session. Use a clear and concise writing style, and include specific details about the patient's symptoms, behaviors, and progress. You can also use a counseling case notes template or a counselor notes template as a guide. Document any notable events or behaviors, and include any relevant psychological or medical information. Finally, review and edit your notes to ensure accuracy and completeness and keep them confidential and secure.

















-template.jpg)