What are therapy progress notes?
Therapy progress notes are essential clinical documents for mental health professionals, providing a comprehensive record of a client’s treatment journey. These clinical notes are crucial in tracking client progress, documenting therapeutic interventions, and capturing detailed information that supports continuity of care across therapy sessions.
Mental health progress notes follow a systematic approach to recording each therapy session. They capture the client’s presentation, therapeutic interventions used, and the client’s response to treatment, offering licensed therapists and healthcare professionals a structured way to document progress.
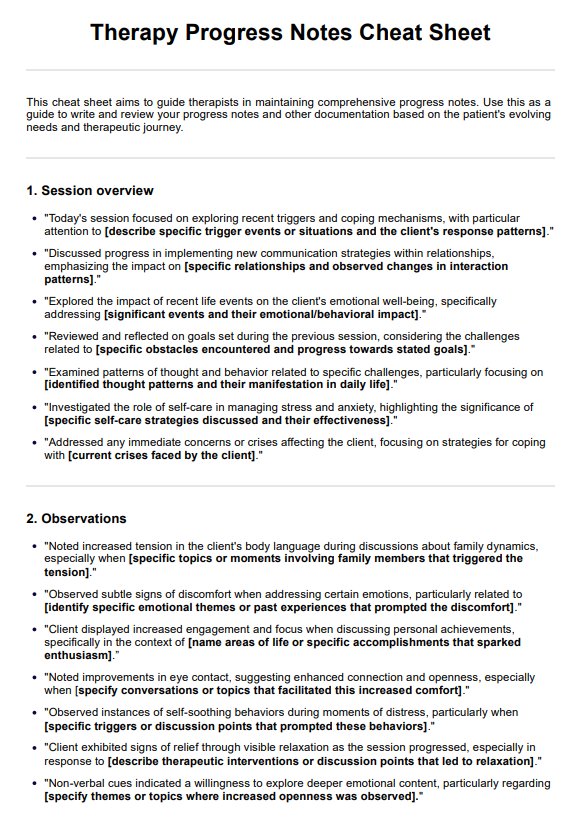
When writing progress notes, include the following key elements:
- Basic session information: (date, time, duration)
- Client’s mental status and presentation
- Topics discussed during the session
- Interventions used (such as coping skills and cognitive restructuring) and client’s response
- Assessment of progress toward treatment goals and clinical impressions
- Plans for future sessions or homework assignments
This quick reference guide ensures that therapy notes contain the relevant information, allowing for quality documentation that enhances client care and tracks therapeutic progress effectively.