Lead Poisoning Treatment Guidelines
Explore our comprehensive handout, which provides detailed, evidence-based guidelines for the treatment of lead poisoning to support effective care.


What is lead poisoning?
Lead poisoning, or lead toxicity, is a serious condition caused by the accumulation of lead in the body, which disrupts essential physiological processes. Lead mimics important minerals like calcium and iron, interfering with enzymes and cellular functions. Exposure commonly occurs through ingestion or inhalation from sources such as lead-based paint, contaminated soil, water from lead pipes, industrial emissions, and certain traditional medicines.
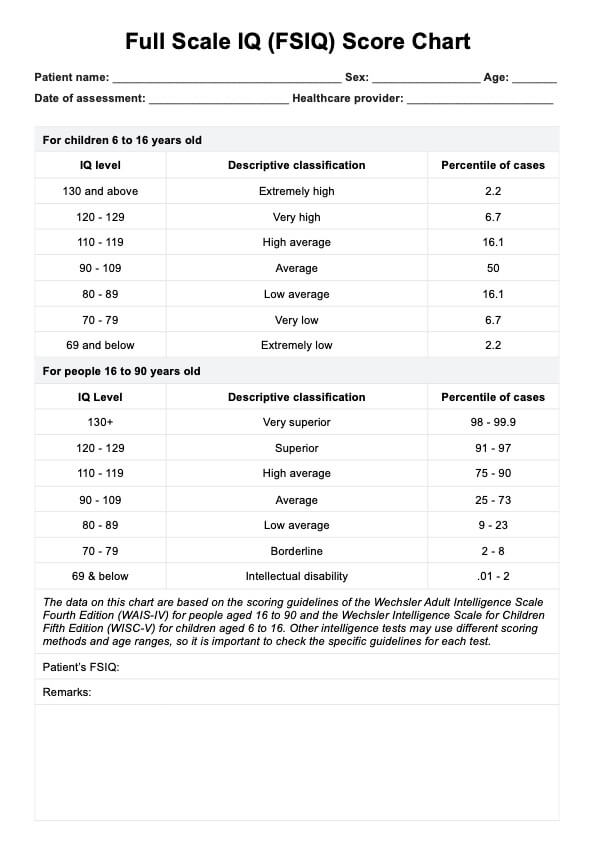
Symptoms vary depending on the level of exposure and age. In children, even low exposure can result in developmental delays, cognitive impairments, and behavioral issues, while severe cases may lead to seizures or death. Adults may experience hypertension, memory problems, and fertility issues, while pregnant women face increased risks of fetal brain damage and miscarriage.
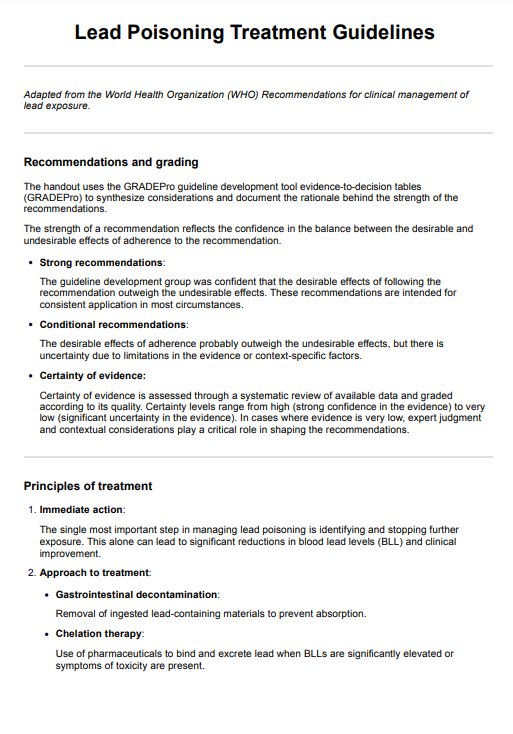
This handout summarizes the World Health Organization (WHO) recommendations for the treatment of lead exposure, focusing on evidence-based approaches such as chelation therapy and gastrointestinal decontamination to manage toxicity and reduce lead levels effectively.
http://Lead Poisoning Treatment Guidelines Template
http://Lead Poisoning Treatment Guidelines Example
Lead poisoning treatments
The treatment of lead poisoning aims to reduce blood lead levels (BLLs) and mitigate its toxic effects. Management varies depending on the severity of lead exposure, age, and individual health status. Below are the key treatments, including those highlighted in the guidelines.
Immediate exposure removal
The first and most critical step in managing lead poisoning is identifying and stopping further lead exposure. This alone can significantly reduce BLLs over time and improve clinical outcomes. Strategies include:
- Removing lead-based paint, contaminated soil, or lead pipes.
- Ensuring safe drinking water.
- Discontinuing lead-containing products (e.g., traditional medicines or cosmetics).
This foundational step is universally recommended across treatment guidelines.
Gastrointestinal decontamination
Gastrointestinal decontamination prevents the absorption of ingested lead materials, particularly in cases of acute exposure. Treatments include:
- Esophagogastroduodenoscopy (EGD) or surgery: Recommended for removing solid lead objects (e.g., bullets, fishing weights) from the stomach, which dissolve in stomach acid, increasing toxicity risks.
- Whole bowel irrigation (WBI): Used for lead-containing objects or dispersed materials (e.g., paint chips, ceramic glaze) in the intestines. It is effective for clearing the GI tract, mainly when other methods are unavailable.
These interventions are crucial for mitigating acute toxicity but depend on the material type and location.
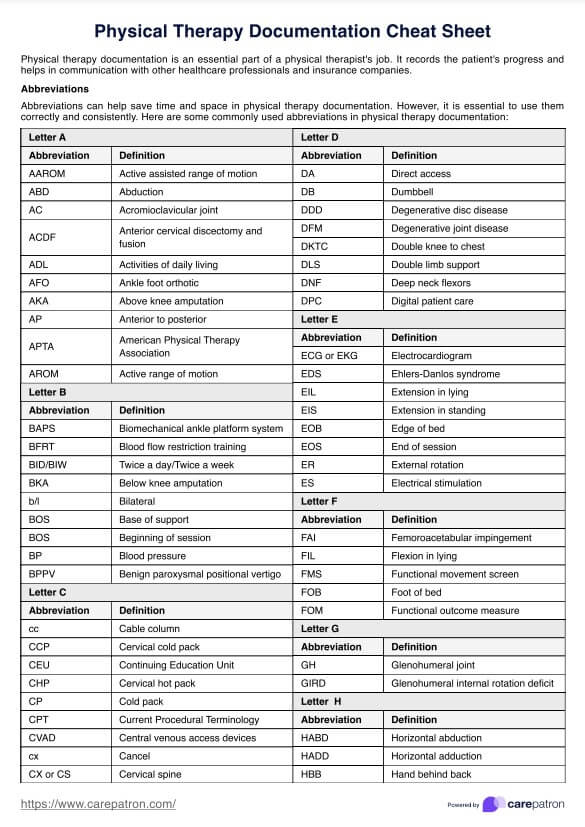
Chelation therapy
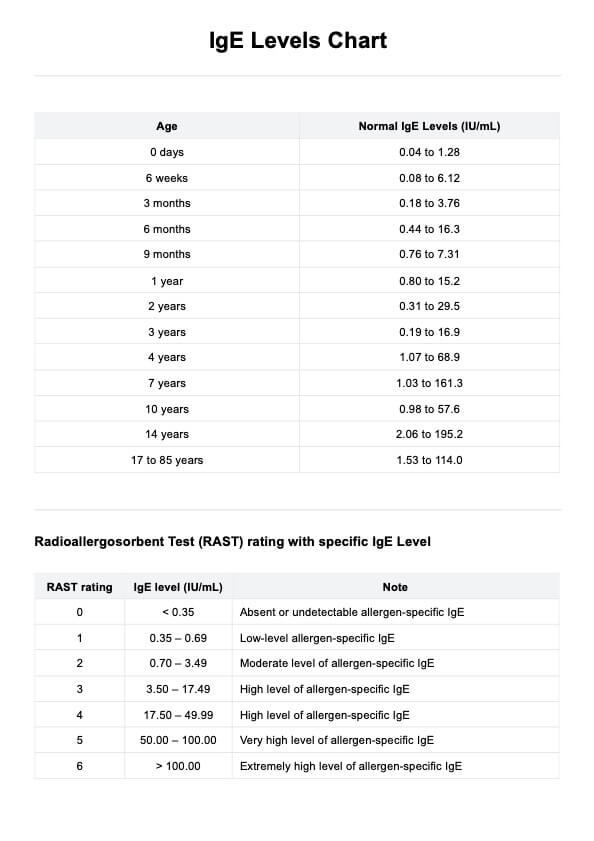
Chelation therapy involves pharmaceuticals that bind lead, facilitating its excretion. It is indicated for individuals with significantly elevated BLLs or symptoms of toxicity. Common agents include:
- Succimer (DMSA): An oral chelator for children with BLLs ≥45 µg/dL. It is often the first-line treatment due to its safety profile.
- Calcium disodium EDTA (CaNa2-EDTA): Administered intravenously, used in severe cases or when oral chelation is ineffective.
- Dimercaprol (BAL): Combined with CaNa2-EDTA for life-threatening lead encephalopathy.
Chelation therapy reduces the body’s lead burden but requires careful monitoring for potential side effects like renal dysfunction.
Surgical removal
Surgical intervention is warranted in cases where lead-containing objects, such as those lodged in the appendix, are causing appendicitis or increasing blood lead concentrations. For asymptomatic individuals, periodic monitoring may suffice, but surgery is recommended if toxicity signs develop.
Nutritional interventions
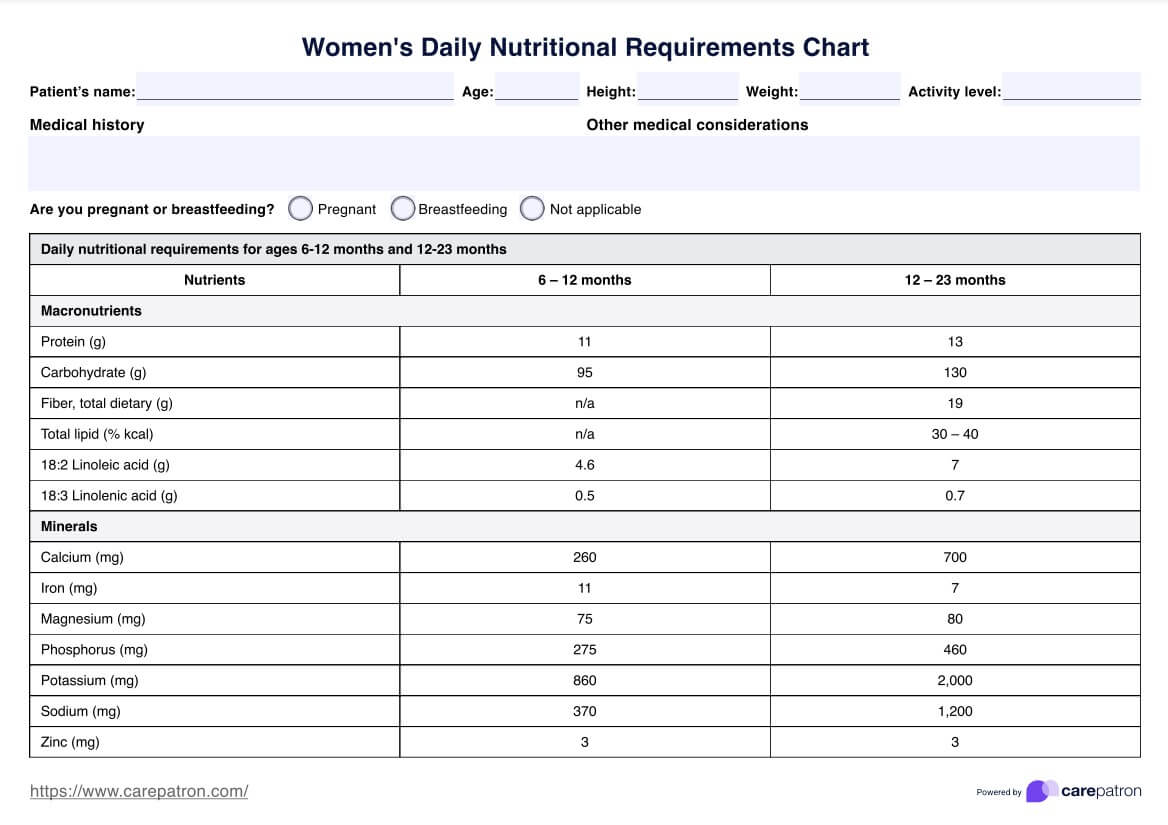
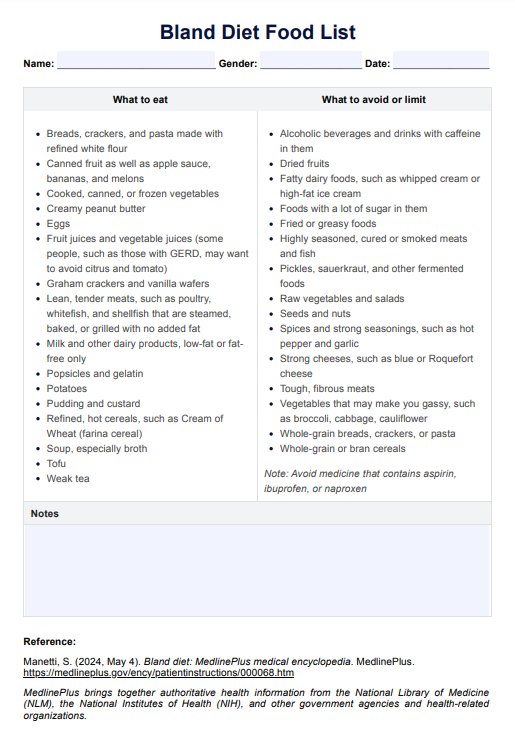
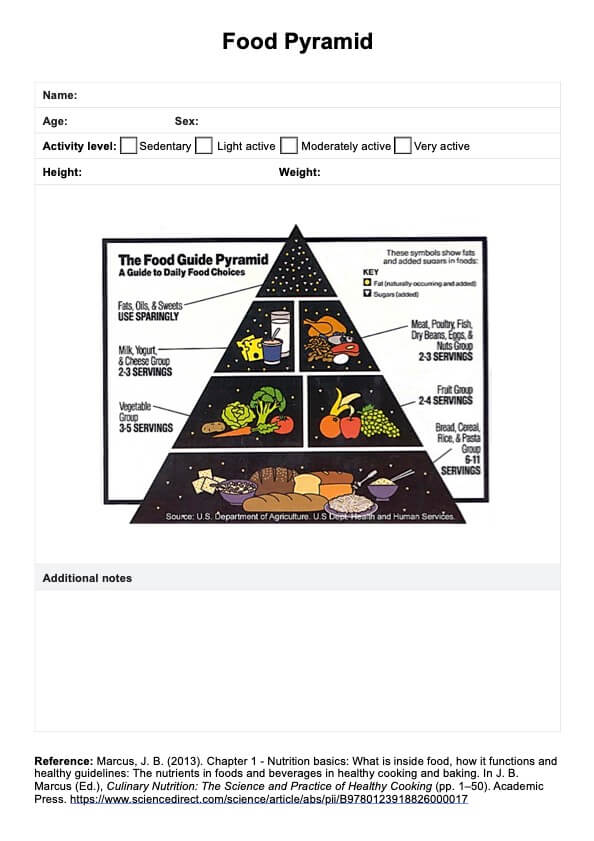
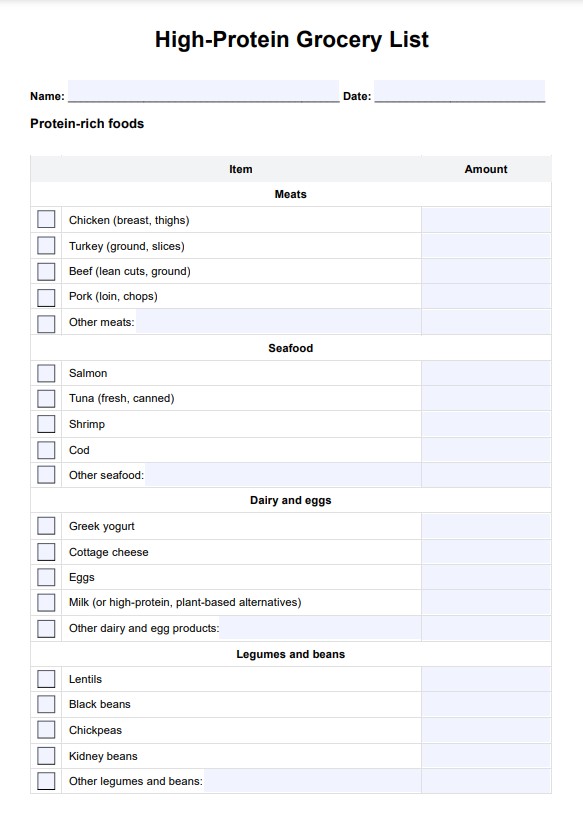
Enhancing nutritional status can help reduce lead absorption and toxicity, particularly in children. Adequate intake of:
- Calcium: Competes with lead for absorption in bones.
- Iron: Reduces lead absorption in the gastrointestinal tract.
- Vitamin C: Enhances lead excretion.
Nutritional interventions are adjunctive and beneficial in populations at high risk of malnutrition.
How to use our Lead Poisoning Treatment Guidelines Handout
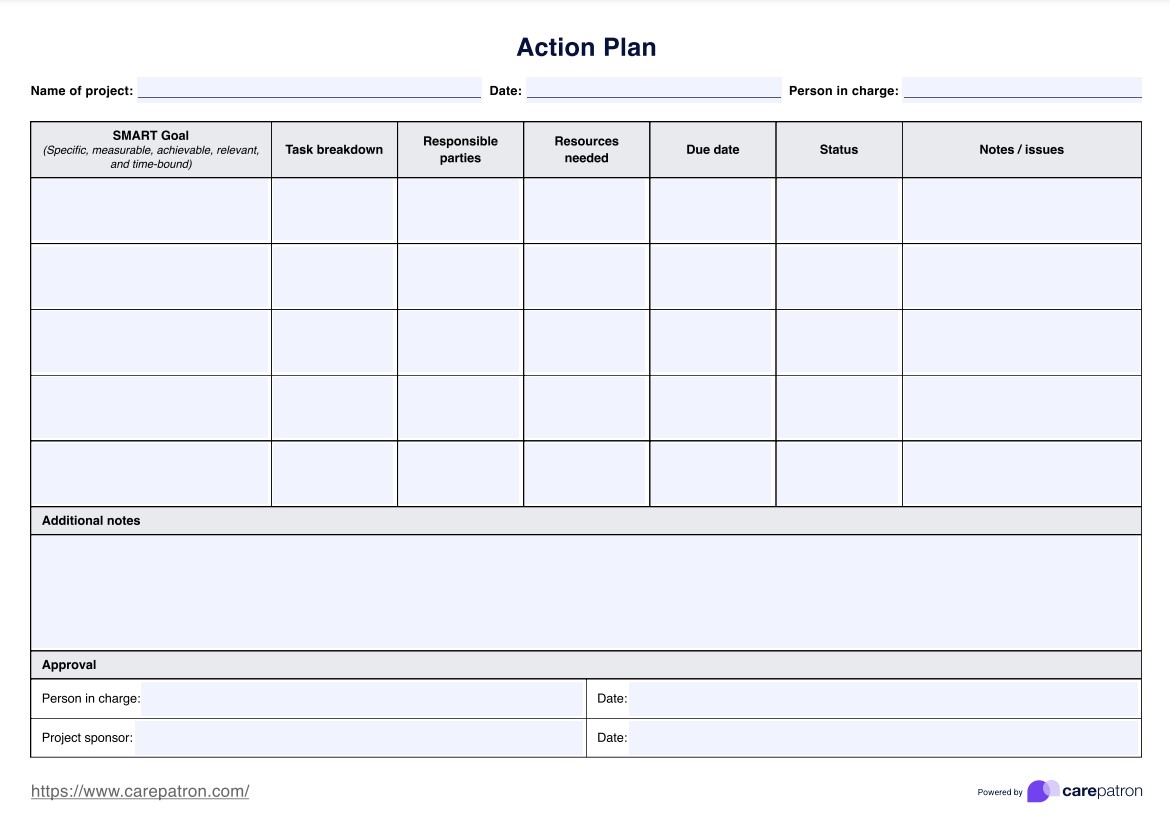
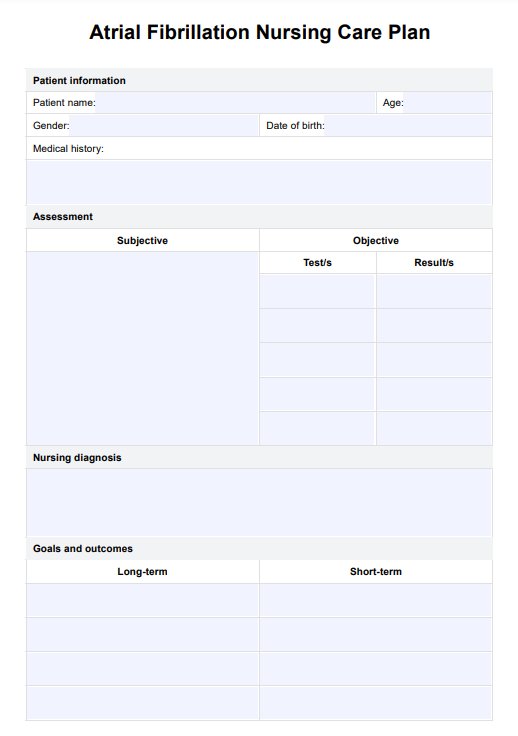
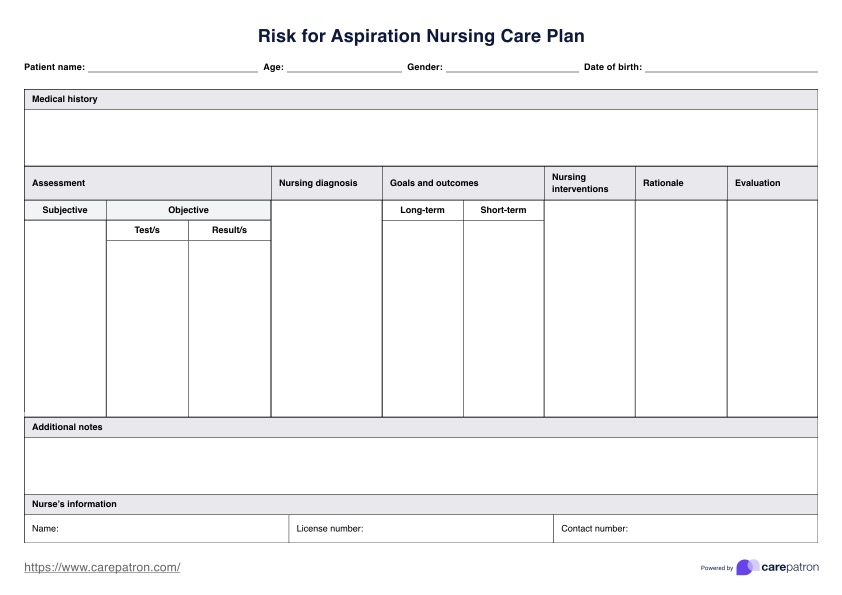
Here's how to use our free handout template:
Step 1: Access the handout
Access the Lead Poisoning Treatment Guidelines Handout via the Carepatron resource library. Use the "Use Template" option to edit directly in the app or download a PDF for easy reference during consultations.
Step 2: Familiarize yourself with the content
Review the handout to revise the key recommendations for managing lead poisoning. Focus on the principles of treatment, including the importance of immediate exposure removal, gastrointestinal decontamination methods such as whole bowel irrigation or surgical removal, and indications for chelation therapy based on blood lead levels (BLLs).
Step 3: Use the handout during consultations
During consultations, use the handout as a visual aid to explain lead poisoning and its treatments. Highlight the importance of stopping exposure and provide personalized advice to fit the patient’s needs.
Step 4: Provide the handout to patients
Give the patient or caregiver a copy of the handout to use as a reference for managing lead poisoning and preventing future exposure. Encourage them to bring it to follow-up appointments for clarification or review.
Benefits of Using the Lead Poisoning Treatment Handout template
Using our free template handout provides you with the following benefits:
- Simplifies communication: Condenses complex WHO guidelines into clear, actionable steps for managing lead exposure, making it easier to convey essential information.
- Supports evidence-based decisions: Provides reliable recommendations for treatment, including exposure removal, gastrointestinal decontamination, and chelation therapy, aligned with the latest WHO guidelines.
- Tailored for diverse scenarios: Includes specific guidance for different patient groups, such as children, pregnant women, and adults, ensuring relevance across clinical contexts.
- Useful for follow-up care: Serves as a reference to reinforce key messages and address questions during subsequent visits, ensuring continuity of care.
よく寄せられる質問
Lead poisoning occurs when lead accumulates in the body, often over months or years. It can cause a range of health issues, from developmental delays in children to memory loss and joint pain in adults. Acute lead poisoning, caused by high levels of exposure in a short time, can lead to severe symptoms like abdominal pain and seizures. Reducing blood lead levels through treatment and stopping exposure is essential for health recovery.
Lead exposure commonly comes from lead-based paint, contaminated soil, drinking water from lead pipes, and specific workplace materials. In children, lead paint in older homes is a frequent cause of lead toxicity, leading to elevated blood lead levels. Identifying and addressing these sources is critical for disease control and prevention.
Treating lead poisoning begins with identifying and removing the source of exposure. For individuals with elevated blood lead levels, therapies such as chelation may be used to help reduce them. Both childhood lead poisoning and adult lead exposure require monitoring and sometimes medical intervention to prevent long-term health effects.
Childhood lead poisoning prevention focuses on primary prevention by removing or reducing lead hazards before exposure occurs. This includes maintaining homes to prevent deterioration of lead-based paint, testing drinking water for lead contamination, and following Environmental Protection Agency (EPA) guidelines for safe lead removal. Local public health officials and environmental health agencies can provide resources and assistance.