Headache Physical Exam
Know more about how to do a physical examination for a headache with this guide, and grab a copy of a helpful template you can use during the assessment.


What is a headache physical examination?
A headache physical examination is a comprehensive assessment conducted by a healthcare professional to identify and understand the underlying causes of an individual's headache. This process is crucial for accurate headache diagnosis and subsequent treatment.
The examination consists of various steps designed to gather specific information about the patient's health and symptoms. Here's a list of the aforementioned steps:
- Gather information: General health, medical history, and family history of headaches or migraines
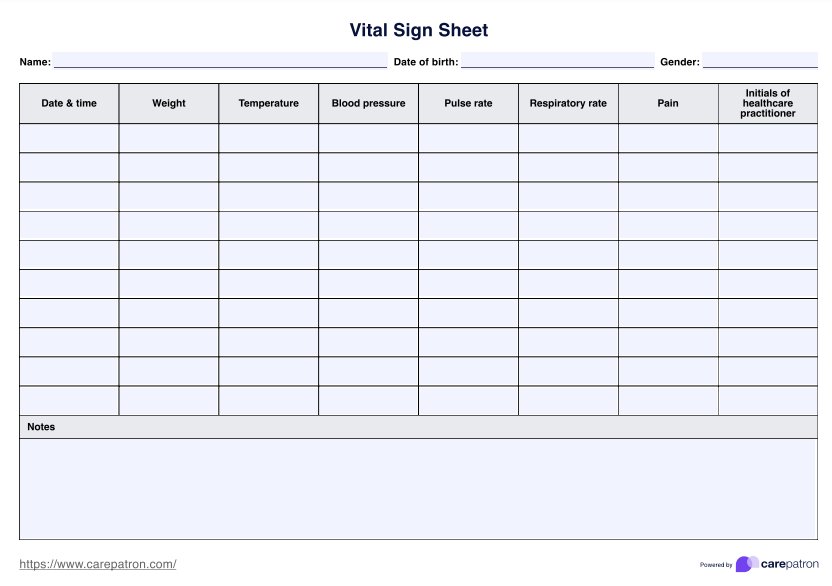
- Checking vital signs: Blood pressure, reflexes, and temperature
- Assessing demeanor: Signs of restlessness or calmness
- Identifying any neurologic issues: Visual changes, weakness, tingling, and balance issues
- Checking for head symptoms: Signs of swelling in the scalp, temporal artery, jaw-to-skull joints, and throat behind the mouth
- Checking for eye symptoms: Changes in visual field, responsiveness to light, and pupil size
- Checking for neck symptoms: Identify stiffness or discomfort
- Checking for cervical spine symptoms: Scrutinized for tenderness
This thorough examination aims to rule out underlying conditions such as sinus infections, toothaches, and head injuries that might be associated with the headaches. Furthermore, it aids in recognizing patterns that could indicate migraine, tension headaches, or cluster headaches, enabling the healthcare professional to determine the most suitable course of treatment.
Headache Physical Exam Template
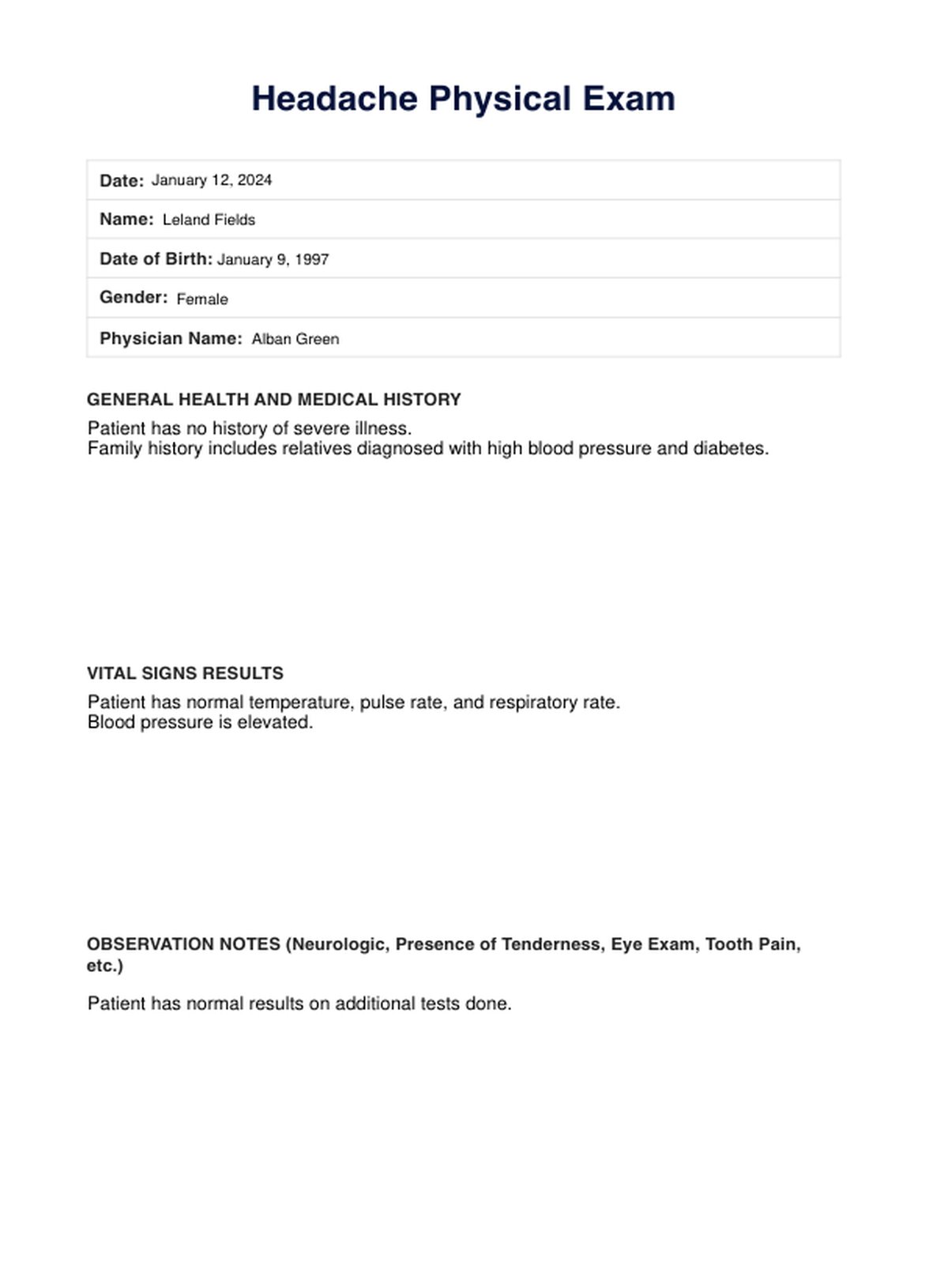
Headache Physical Exam Example
Signs and symptoms your patient needs a headache exam
A patient with a headache may require a headache examination if they manifest specific signs and symptoms indicative of underlying health issues. Signs and symptoms may be any of the following:
- Distinctive headache characteristics: Intense, sharp/stabbing pain, unilateral headaches lasting up to three hours, or persistent dull headache that doesn't throb
- Systemic symptoms: Runny nose, nasal congestion, sweating, warm skin, restlessness, droopy eyelid, tears, eye redness, stiff neck, shoulder pain, sensation of tightness around the head
- Neurological symptoms: Gradual progression or sudden onset of explosive headaches
- Meningeal symptoms: Neck stiffness or photophobia
- Focal neurologic deficits: Weakness, double vision, sensory issues, gait problems
- Others: Nausea and vomiting
Special consideration should be given to elderly patients with new-onset headaches, as temporal arteritis may be a potential concern.
If headaches are frequent, debilitating, and significantly impact daily activities, the patient must seek medical help. It is essential to recognize that these symptoms are diverse and may point to various underlying conditions; therefore, only a healthcare professional can provide accurate diagnosis and appropriate management.
Headache disorders
Before you finalize your headache diagnosis, you should know the different headache disorders your patient may have.
Primary headache disorders
Migraine headache
Among the primary headache disorders, a migraine headache stands out as a complex tapestry of pain that often emerges during puberty and predominantly affects individuals between the ages of 35 and 45. A migraine headache is notorious for its debilitating nature, with symptoms encompassing throbbing head pain, heightened sensitivity to light and sound, and, in some cases, nausea and vomiting.
Tension-type headache
Tension-type headache emerges as a commonplace primary headache disorder, affecting a considerable portion of the population. Characterized by a dull, persistent pain often described by most patients as a 'tightening' sensation, these headaches can be chronic or episodic, contributing to a significant burden on individuals and society.
Trigeminal Autonomic Cephalalgias (TAC)
Trigeminal autonomic cephalalgias (TAC) present a cluster of conditions marked by neurologic symptoms and intense, severe pain episodes. This category includes notorious entities like cluster headache and paroxysmal hemicrania, which, while relatively rare, induce excruciating pain and are often accompanied by autonomic symptoms like tearing nasal congestion, or drooping eyelids.
Other primary headache disorders
Beyond the more prevalent categories, the realm of primary headache disorders encompasses a diverse spectrum of conditions under the 'Other' classification. This includes headaches triggered by coughing, physical activity or exertion, or even during sleep (hypnic headaches).
Secondary headache disorders
Unlike primary headaches, which are standalone disorders, secondary headaches are symptoms signifying an associated disease or condition.
Headache attributable to trauma
Secondary headaches stemming from trauma illuminate the interconnected relationship between physical injuries and resultant head pain. Whether caused by accidents or other forms of head trauma alone, these headaches serve as poignant indicators of underlying damage and necessitate thorough evaluation.
Vascular disorders
Vascular disorders encapsulate a category of secondary headaches intricately linked to issues within the circulatory system. From conditions affecting blood vessels to more severe manifestations like arterial dissections, this class underscores the importance of understanding the intricate interplay between vascular health and headaches.
Nonvascular intracranial disorders
Beyond vascular realms, nonvascular intracranial disorders shed light on conditions within the cranial space that can contribute to headaches. This category encompasses a spectrum of conditions, from benign intracranial hypertension to more complex intracranial pathologies.
Substance use or withdrawal
A secondary headache associated with substance use or withdrawal emphasizes the intricate relationship between chemical dependencies and their impact on neurological well-being. Headache onset that arose from medication overuse or withdrawal symptoms underscores the need for a comprehensive understanding of a patient's substance-related history.
Infection
Infections, ranging from common ailments to more severe conditions, can manifest as secondary headaches. This category highlights how pathogens can impact neurological function and contribute to head pain.
Disorders of hemostasis
Disorders affecting the body's coagulation dynamics are implicated in secondary headaches. Understanding the intricacies of hemostasis becomes crucial in deciphering the underlying causes of these headaches.
Disorders affecting the structures of the head or neck
Structural anomalies within the head or neck can give rise to an acute headache and a secondary headache. From abnormalities in cranial structures to issues within the cervical spine, this category emphasizes the importance of considering anatomical influences.
How does this physical examination template work?
Step 1. Access the template
Begin by accessing the headache physical examination template. This may be a digital form within an electronic health record (EHR) system or a paper-based document. For your ease, you can find such a template in Carepatron's template library or within this guide. Click the "Use Template" or "Download Template" button to obtain a copy. Feel free to customize the template to ensure that it aligns with the specific requirements of the patient encounter.
In addition, to help you out, you may use supplemental resources like a headache chart or headache location chart to aid you with diagnosis.
Step 2. Review patient information
Before initiating the physical examination, review the patient's medical history and any existing health records. This preliminary understanding aids in customizing the examination based on the patient's unique health status, family history, and concerns.
Step 3. Conduct assessments
Start with a comprehensive assessment of vital signs, including blood pressure, heart rate, respiratory rate, and temperature. Then, systematically observe and document general aspects of the patient's appearance. Note signs of distress, abnormalities, or relevant information such as skin color, posture, and overall demeanor.
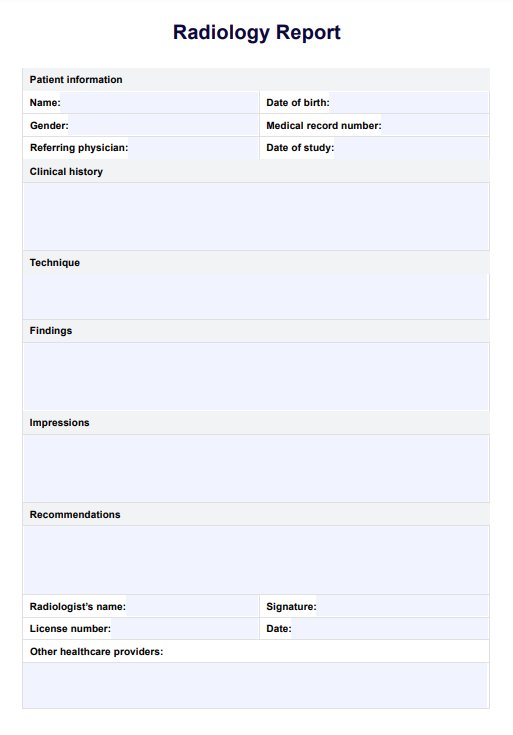
Afterward, you may proceed to the body systems (e.g., cardiovascular, respiratory, neurological). Follow the structured order outlined in the template to ensure a thorough examination. For each system, follow the specific examination components outlined in the template. If applicable, perform a neurological examination, including cranial nerves, reflexes, and sensory/motor function assessments.
Feel free to conduct specialized assessments based on the patient's condition or complaints.
Step 4: Document findings
As examinations are conducted, meticulously document findings in the designated spaces on the template. Use clear and concise language to accurately convey observations, measurements, and any abnormalities detected during the examination.
Step 5: Summary and assessment
Conclude the physical examination template with a summary of findings and an initial assessment. This section may include provisional diagnoses, recommended further investigations, or specialist referrals.
Step 6: Communicate with the patient
Share relevant findings with the patient clearly and compassionately by telling them or showing them the filled-out template. Address any concerns or questions they may have, fostering open communication and ensuring a collaborative approach to healthcare.
Step 7: Record keeping
Ensure the completed physical examination template is appropriately saved or filed in the patient's health record. This documentation is a vital reference for future assessments, care planning, and continuity of care.
Step 8: Follow-Up actions
Based on the findings and assessments, outline any necessary follow-up actions, whether additional diagnostic tests, consultations, or a scheduled follow-up appointment.
Headache diagnosis and treatment
Effectively diagnosing and treating headaches involves a strategic approach encompassing a thorough examination and personalized interventions. Here's a comprehensive guide to help you understand the critical steps in this process.
Diagnosis
- Medical history assessment: Begin with a detailed exploration of your patient's symptoms, medical history, and familial headache patterns. This foundational step helps identify potential triggers and underlying causes.
- Physical and neurological examinations: Conducting a comprehensive physical and neurological examination is crucial. This step aims to uncover any physical illnesses or neurological issues contributing to the headaches.
- Headache diary: Require and check your patient's headache diary to track occurrences, symptoms, and potential triggers such as dietary factors, stress, or sleep patterns.
Treatment
- Self-care measures: Initial self-care steps can be beneficial in less severe cases. These may include resting in a dark room and using over-the-counter medications like ibuprofen, acetaminophen, or aspirin.
- Hydration: Addressing dehydration, a common headache trigger, is vital. Ensure your patient is adequately hydrated; water intake can significantly impact headache frequency and intensity.
- Caffeine intervention: Pairing a caffeinated beverage with over-the-counter pain medication can sometimes expedite headache relief.
- Temperature therapy: Employ cold or hot compresses on your head or eyes to alleviate built-up pressure and ease pain.
- Lifestyle modifications: Having your patient establish a consistent sleep schedule and incorporate daily exercise into their routine can serve as preventive measures, reducing the likelihood of recurrent headaches.
- Magnesium supplementation: Consider magnesium supplementation, a safe and effective remedy to mitigate headache symptoms.
When to seek professional help
If headaches persist, disrupt daily activities, or are accompanied by alarming symptoms such as confusion, weakness, slurred speech, loss of consciousness, blurry vision, nausea, vomiting, or high fever, encourage your patient to seek immediate medical attention. Professional evaluation is imperative for accurate diagnosis and tailored treatment plans.
Commonly asked questions
You can assess headache pain by checking its location, duration, severity, onset, and quality. Afterward, you may use a headache physical examination template to obtain more detailed information.
The physical exam done for a migraine headache is the same as the one used for headaches in general.
Aside from physical examinations, the referring physician may request additional examinations to diagnose the type of headache the patient may have, such as blood and imaging tests.














-template.jpg)