Cerebellar Exam
Discover the comprehensive guide to conducting a Cerebellar Exam. Enhance patient care via effective neurological assessments. Learn more today with Carepatron.


What is cerebellar dysfunction?
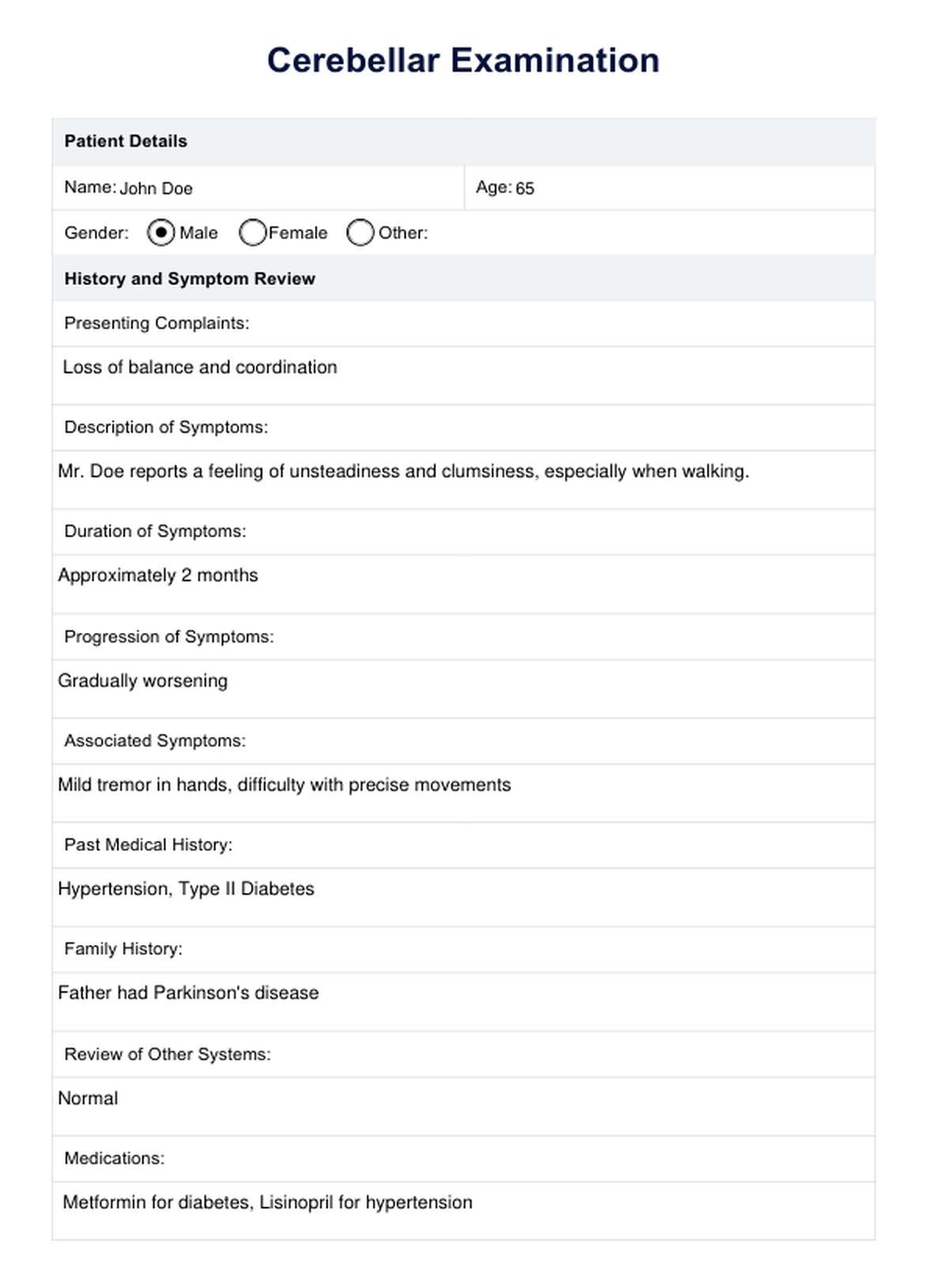
Cerebellar dysfunction is characterized by impairment of the cerebellum, a crucial part of the brain that plays a significant role in coordinating voluntary movements, maintaining balance and posture, and integrating motor functions. This dysfunction disrupts some cognitive functions and the cerebellum's ability to regulate these activities effectively, leading to difficulties with coordination and precision in physical movements.
Numerous conditions can lead to cerebellar dysfunction, ranging from vascular issues like stroke and multiple sclerosis to genetic conditions like Friedreich's Ataxia. The condition manifests through various clinical signs and motor symptoms, including unsteady movements, lack of coordination, and an inability to maintain normal posture, directly affecting an individual's ability to perform everyday tasks smoothly and efficiently.
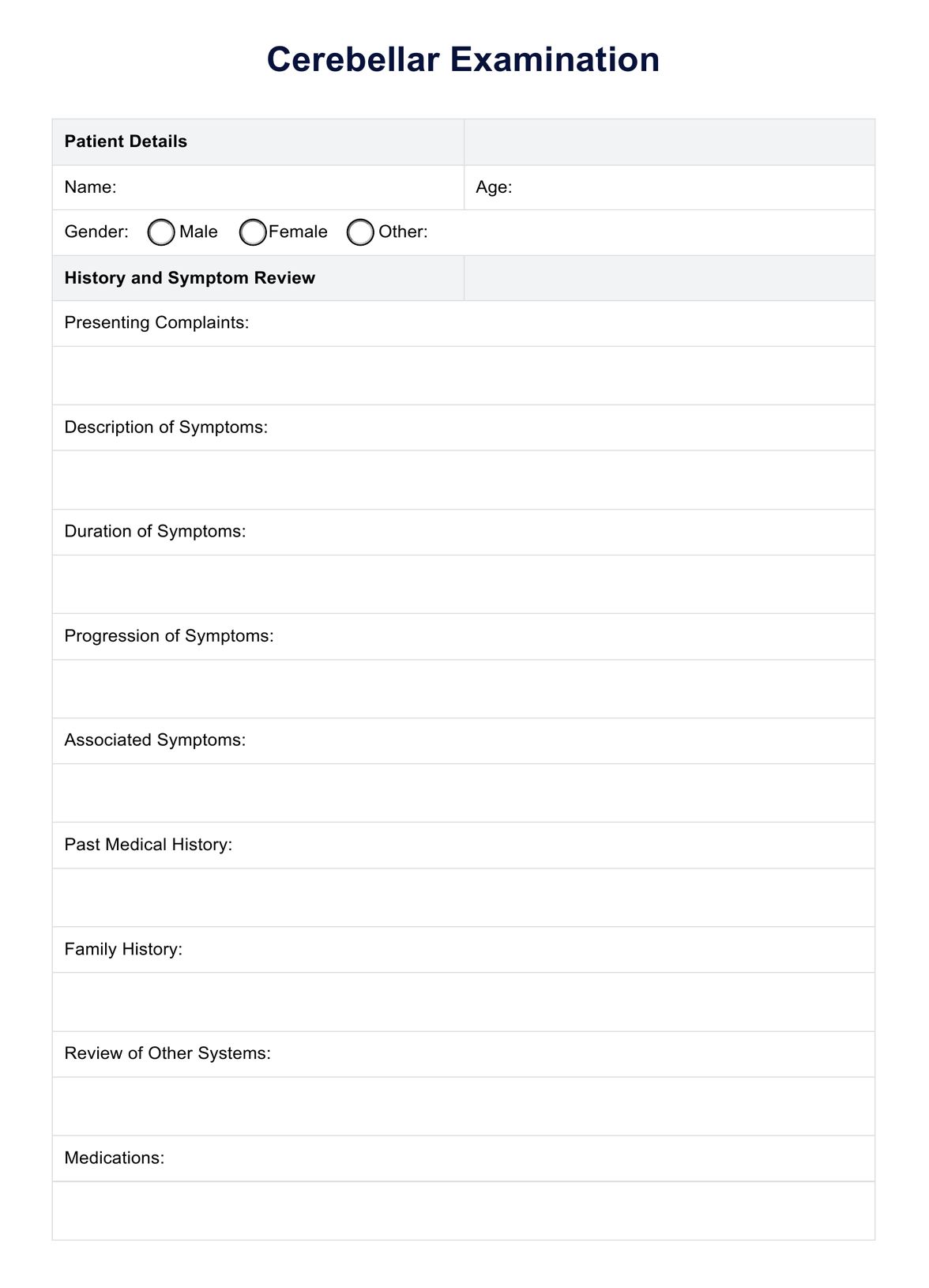
Cerebellar Exam Template
Cerebellar Exam Example
What is a Cerebellar Exam?
A Cerebellar Exam is a comprehensive and specialized physical examination targeted specifically at the cerebellum — an integral brain region located at the posterior end.
Patients presenting cerebellar signs or symptoms of pathology, such as dizziness, loss of balance, or poor coordination, often undergo a cerebellar examination. Healthcare professionals use this examination to diagnose such conditions, encompassing the analysis of gait, balance, and coordination.
Interested in learning more about conducting a thorough Cerebellar Exam? Check out Carepatron, which health professionals sample to ensure they perform the most effective and thorough procedures.
You can also gain deeper insights through Carepatron's explainer video below.
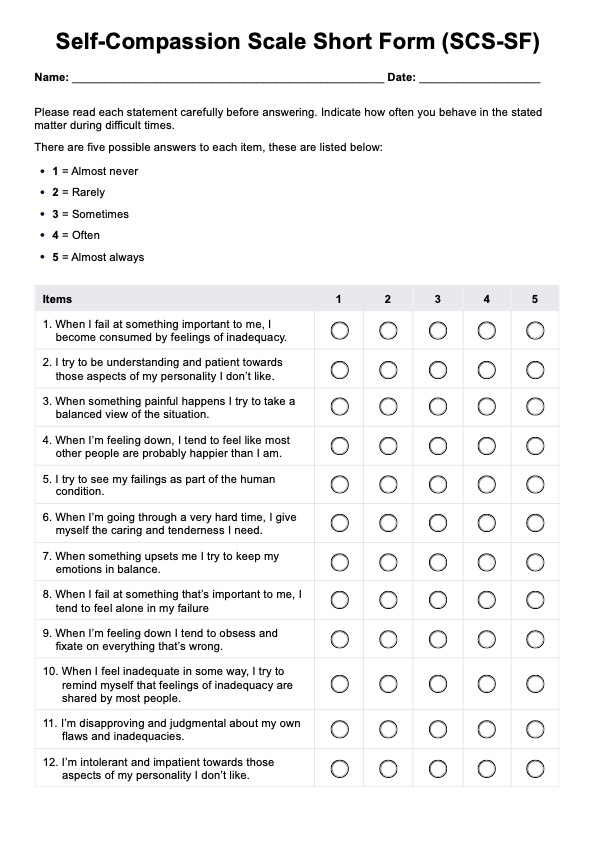
How does this Cerebellar Exam template work?
The Cerebellar Exam or cerebellar function test involves a series of precise tests, each formulated to assess a distinct cerebellum function, and is done through a well-defined, step-by-step process:
Step 1: Patient preparation
Proper preparation of the patient is essential before conducting the neurological examination. This stage involves thoroughly explaining the nature and purpose of the procedure to the patient and obtaining their informed consent, respecting their autonomy and right to participate actively in their care.
Step 2: Execution of tests
This step involves administering a series of cerebellar tests specially designed to assess the integrity and function of the cerebellar system. Each test targets a unique aspect of cerebellar functioning, ensuring a comprehensive evaluation of the patient’s neurological status. Here's a list of said tests and instructions on how to conduct them:
- Finger-to-nose test: Ask the patient to touch their nose with their fingertip and then reach out to touch the examiner’s index finger, which is moved to different positions. This test assesses coordination and the ability to perform controlled movements.
- Heel-to-shin test: Ask the patient to slide the heel of one foot up and down the shin of the opposite leg. This test evaluates the coordination of lower limb movements.
- Rapid alternating movements: Ask the patient to perform rapid, alternating hand movements, such as pronation and supination of the hands. This assesses the ability to coordinate rapid, repetitive movements.
- Gait analysis: Observe the patient’s walking pattern to assess balance and coordination. Patients with cerebellar dysfunction may exhibit an ataxic gait characterized by a wide support base and irregular steps.
- Impaired smooth pursuit: Ask the patient to follow a moving object with their eyes, such as a finger, and note any jerky or saccadic movements. This test assesses oculomotor disturbances commonly associated with cerebellar dysfunction.
You may also conduct additional tests to check the knee jerk reflex and evaluate muscle tone with the patient lying on the examination on an examination couch or bed.
Step 3: Interpretation
Once the tests are complete, healthcare professionals interpret the results. This critical stage involves analyzing the findings to identify signs of potential cerebellar dysfunction. The interpretative insights inform the direction of subsequent patient care.
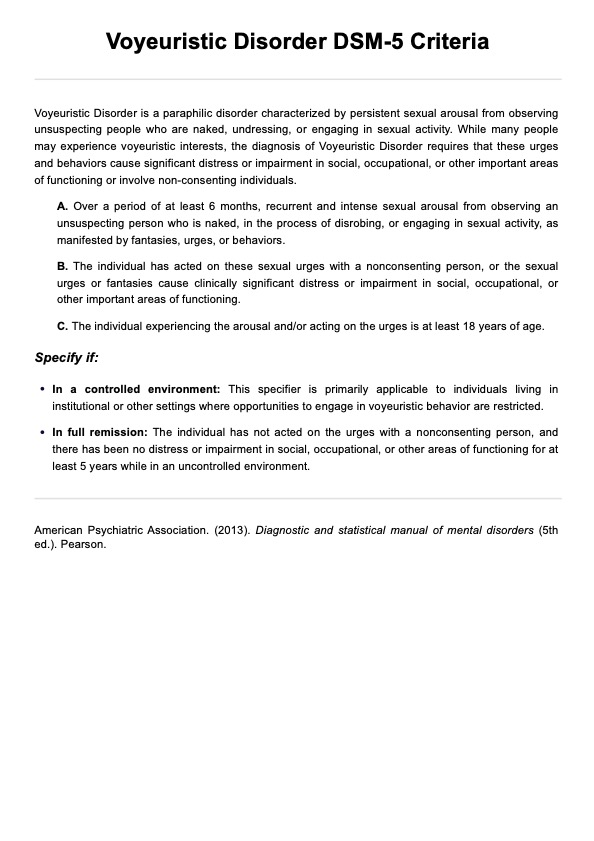
Interpretation of results
Interpreting the results of the examination of the cerebellum is a nuanced process that requires a thorough understanding of cerebellar anatomy and its associated functions. Here are the possible interpretations of some results you will obtain:
- Poor performance in coordination tasks: Difficulty or inaccuracy in performing tasks for tests such as the finger-nose test, heel-to-shin test, and rapid alternating movements can indicate cerebellar ataxia, a common sign of cerebellar dysfunction.
- Observed ataxic gait: The patient’s walking pattern is closely observed. An ataxic gait or lack of coordination in the right and left leg, characterized by unsteady and wide-based walking, often suggests cerebellar involvement.
- Presence of intention tremor: This type worsens with targeted movement and is a key indicator of cerebellar issues. It is typically assessed through tasks that require precise targeting, like the finger-to-nose test.
- Presence of dysdiadochokinesia: This term refers to the inability to perform rapid alternating movements, such as quickly flipping the hands back and forth. Difficulty with these movements can point to cerebellar lesions.
- Difficulty with balance and posture: Difficulties with tests that challenge balance and posture, such as standing with feet together or walking in a straight line, indicate the presence of cerebellar lesions.
- Presence of dysarthria: The presence of dysarthria is often associated with cerebellar damage.
- Presence of hypotonia: If one shows signs of hypotonia, especially during an assessment for unilateral cerebellar disease, one may have an ipsilateral cerebellar lesion.
Next steps
After conducting the test, gathering observations, and interpreting results, the next steps must be done as soon as possible. Examples of the next steps healthcare professionals may take are the following:
Interpret the severity and impact
Healthcare professionals must assess the degree of difficulty or inability to perform specific tasks to gain insight into the severity of the cerebellar dysfunction.
Localize the dysfunction
Localize the affected area within the cerebellum, as different regions control different aspects of motor function.
Comprehensive interpretation
Understand the nuances by comprehensively analyzing the test results in conjunction with the patient’s medical history, symptoms, and other diagnostic tests.
Commonly asked questions
The Cerebellar Exam typically takes 10–15 minutes, although this may vary based on the patient's condition.
Interpreting the Cerebellar Exam involves comparing the findings to normal, expected results. Any deviation may indicate potential cerebellar dysfunction.
The Cerebellar Exam is used when there's suspicion of cerebellar dysfunction, often evidenced by symptoms like unsteady gait, lack of coordination, or problems with delicate motor tasks.
Healthcare professionals, particularly those specializing in neurology, can use the Cerebellar Exam. It can also be helpful for general practitioners and physiotherapists.

.jpg)









-template.jpg)