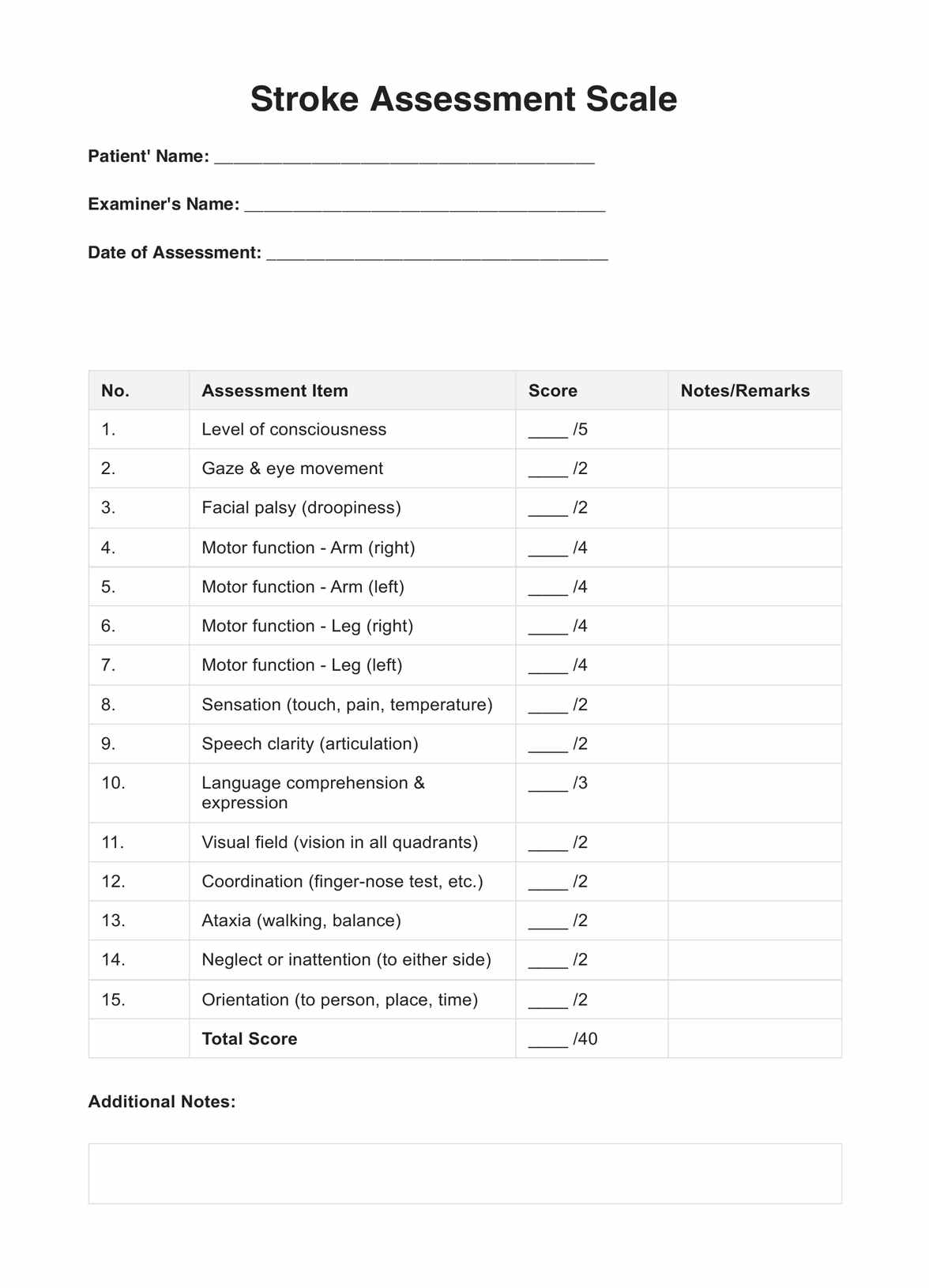
Stroke Assessment Scales
Discover the benefits and intricacies of the Stroke Assessment Scale with Carepatron—essential for timely and accurate evaluations in stroke patient care.


What is a Stroke Assessment Scale?
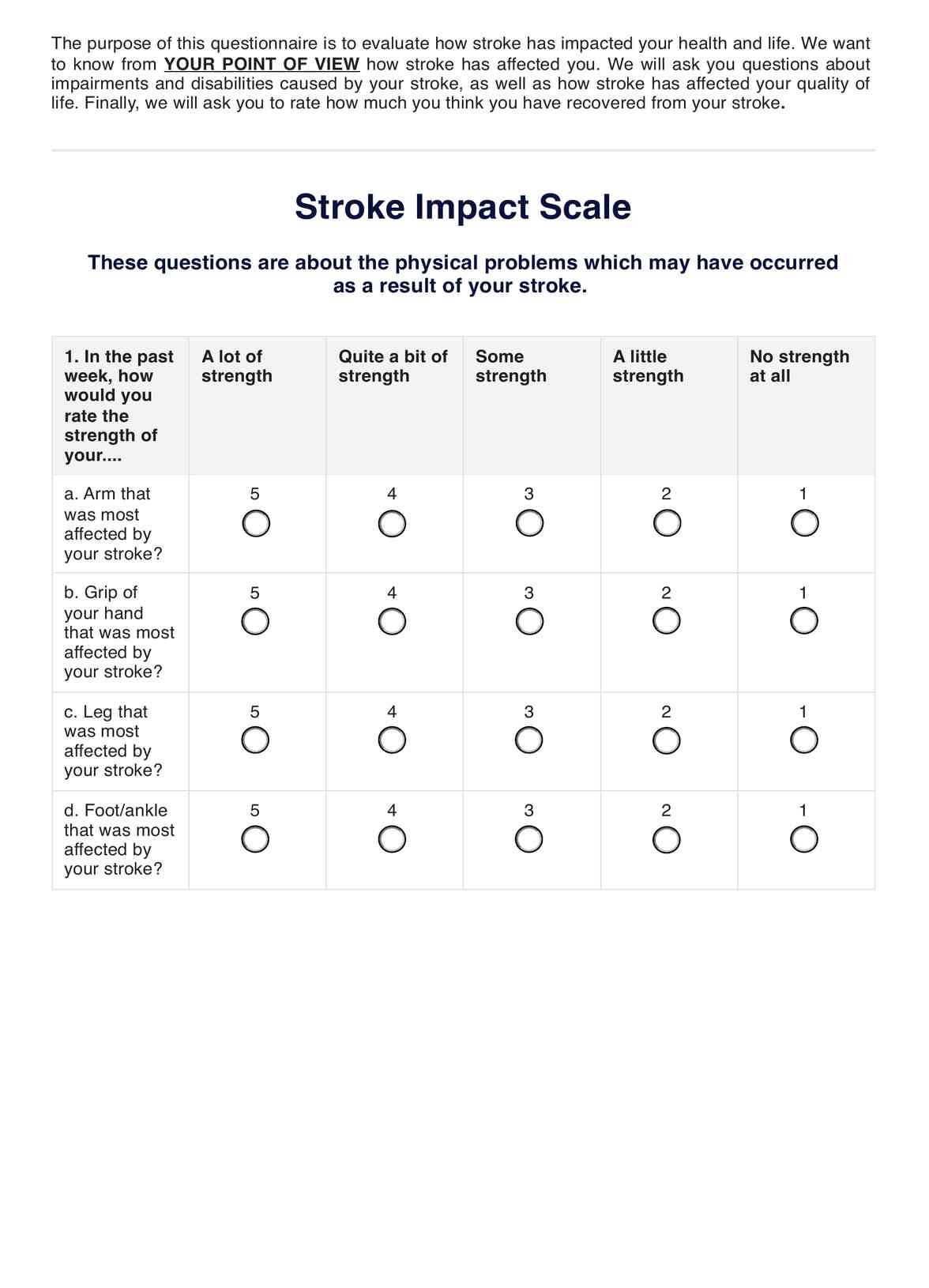
A Stroke Assessment Scale is an instrumental tool in the medical community. Specifically designed for healthcare professionals, it offers a systematic approach to gauge and categorize the severity of strokes that a patient has experienced. A Stroke Assessment Scale provides an invaluable benchmark that shapes critical clinical decisions, projects patient outcomes, and crafts precise treatment strategies.
Beyond its primary function, the scale plays a more prominent role in the grand scheme of medical advancement. It's not only about immediate patient care but also about long-term contributions to medical research. Its ability to offer uniform and reliable data across different patient cohorts makes it an irreplaceable asset for extracting actionable insights and pushing the envelope in stroke care research.
The evolution of the Stroke Assessment Scales traces back to years of dedicated research combined with real-world clinical observations. As these scales have been refined over time, they've become more adept at addressing the nuances associated with stroke severity. When healthcare practitioners integrate these scales into their assessment protocols, they're equipped with a powerful resource. This ensures that they're not just following a general protocol but are creating a bespoke care plan tailored to each patient's unique needs, championing the cause of delivering optimal patient care.
Stroke Assessment Scales Template
Stroke Assessment Scales Example
How does it work?
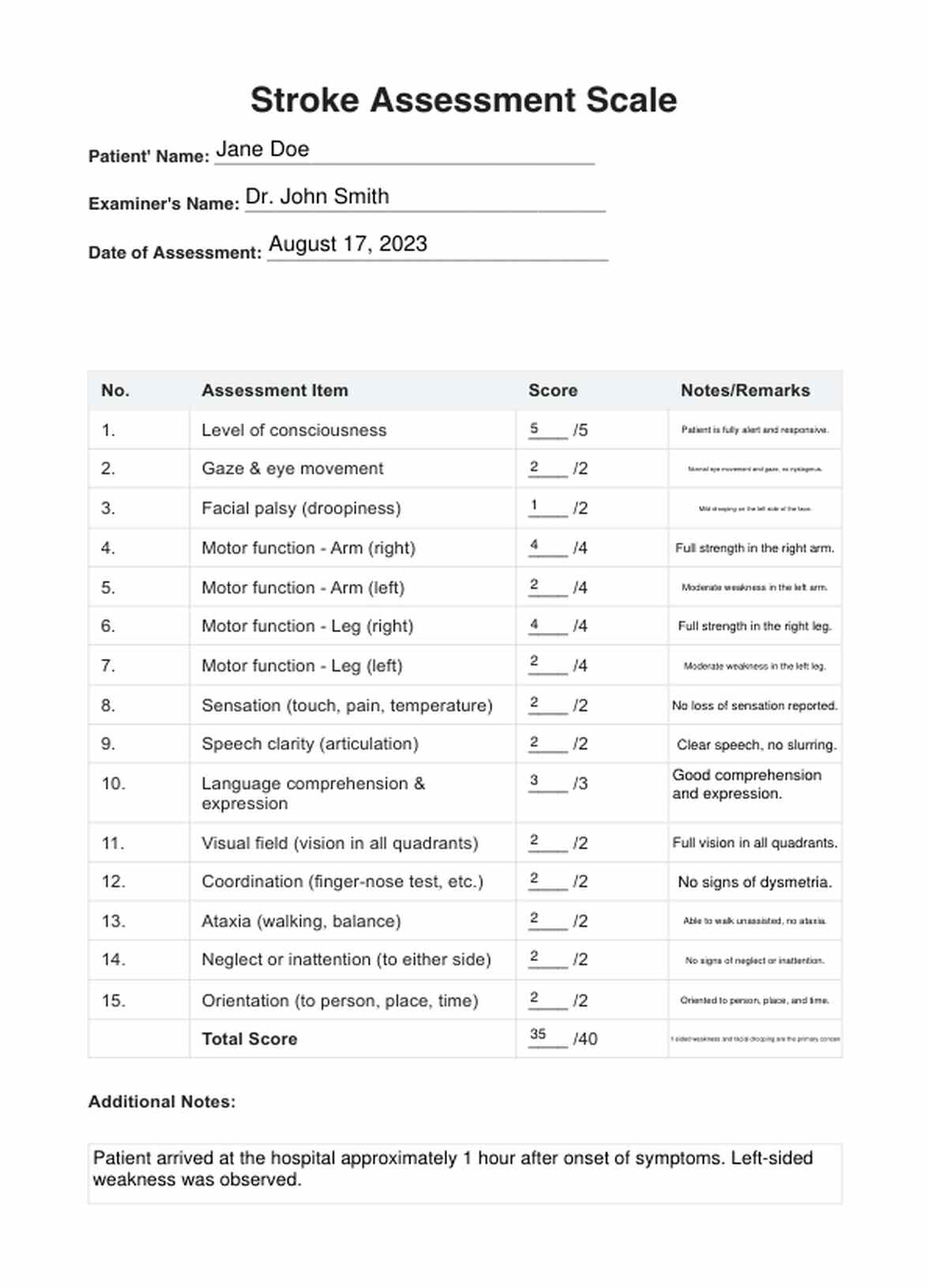
The Stroke Assessment Scale is a meticulously crafted instrument built on years of medical research and clinical observations. Its primary aim is to classify and evaluate the severity of strokes, ensuring that patients receive care tailored to their specific needs. Here's a step-by-step breakdown of how this process unfolds:
Step 1: Comprehensive patient evaluation
Before diving into scoring, it's essential to evaluate the patient holistically. This isn't just a cursory glance but an in-depth observation of their current state. Medical professionals observe and record initial symptoms, ranging from noticeable physical limitations like difficulty moving limbs to speech impediments to the patient's consciousness level.
They will check for vital signs and risk factors like deep vein thrombosis, obstructed blood flow, and more. Understanding these symptoms is crucial, as they are the foundation for subsequent steps, especially when determining what stroke patients are dealing with (e.g., acute ischemic stroke, transient ischemic attack, hemorrhagic stroke, etc.).
This assessment involves checking the levels of consciousness of a stroke patient, including other aspects like if their face is drooping, if there's neglect or inattention to either side of the body, if they have slurred speech, and more.
Step 2: Systematic score assignment
Once initial observations are documented, it's time to assign scores based on the specific criteria set out in the scale. Each symptom is evaluated against this criterion and assigned a corresponding score. While each symptom might have varying degrees of severity, their collective scores will paint a picture that determines just how severe the stroke is.
Step 3: Informed treatment determination
With a cumulative score, medical professionals aren't left in the dark. This score acts as a guiding beacon, illuminating the path forward. Depending on the score's magnitude, healthcare practitioners can initiate appropriate treatments and interventions, ensuring patients receive care that aligns with their unique situation.
Here at Carepatron, we have a printable Stroke Assessment Scales for download.
Step 4: Imaging tests
Imaging tests should be conducted after using this scale (and other similar tools). Here are some examples of such imaging tests: CT angiography (CTA), CT perfusion (CTP), CT venography (CTV), MRI, MR angiography (MRA), and MR perfusion (MRP). This is to get a good look at the brain tissue and determine what stroke phase the patient is at (acute phase, subacute, chronic) and what treatment they should undergo (acute stroke treatment, chronic).
Other assessments to use for (ischemic) stroke patients and survivors
The National Institutes of Health Stroke Scale (NIH Stroke Scale)
The NIH Stroke Scale (NIHSS) is one of the most universally accepted and implemented tools in stroke care and the medical field, endorsed by the American Stroke Association. The NIHSS dives deep into a patient's neurological function. It meticulously evaluates various critical areas, ranging from the patient's level of consciousness and gaze patterns to more intricate aspects like visual fields and the presence of facial palsy.
Stroke Assessment for Nurses
This assessment is normally done on stroke survivors and confined patients. As the name indicates, nurses also conduct it. For this assessment, nurses will check the patient's airway, breathing, and circulation. They will also use the Glasgow Coma Scale to assess the patient's consciousness, pupillary response, and motor and sensory functions. They will also check for facial droops, arm drifts, and slurred speech. Nurses will pass the results to the next nurse taking a shift, and so on.
Medical professionals can utilize such assessments to understand a stroke's impact, allowing them to tailor care and interventions to the patient's unique needs. The NIHSS, with its detailed criteria, ensures that no stone is left unturned when assessing a patient following a stroke.
Implementing this nursing diagnosis template and NIH stroke scale template can boost your practice and client success. It helps clients outline actionable strategies for improvement.
When would you use this Stroke Assessment Scale template?
Standardized tools ensure patients receive consistent, high-quality treatment in the complex medical care arena. Stroke Assessment Scales, particularly the NIHSS, are indispensable among these tools for various reasons and scenarios.
- Immediate post-stroke assessment: The initial hours following a stroke are the most critical period. The Stroke Assessment Scales provide a structured method for healthcare professionals to quickly and systematically evaluate the damage and plan subsequent interventions.
- Determining stroke severity: It's not just about identifying a stroke but also gauging its severity. The nuances between a minor and major stroke can dictate drastically different treatment pathways. Using the NIHSS, clinicians can differentiate between the severities and make informed decisions about immediate care requirements.
- Guiding treatment decisions: Based on the cumulative score from the Stroke Assessment Scale, practitioners can decide on the most appropriate treatments, ranging from medications to potential surgical interventions.
- Predicting patient outcomes: One of the paramount concerns in post-stroke care is predicting how the patient will fare. Stroke Assessment Scales allow for more accurate prognostication, helping families and medical teams set realistic expectations and goals.
- Evaluating treatment efficacy: Post-treatment, these scales serve another vital role. By conducting periodic evaluations using the scale, healthcare providers can monitor a patient's progress and determine the effectiveness of the interventions.
- Research and continuous improvement: On a broader scale, the data garnered from these assessments feeds into medical research. Consistent usage of Stroke Assessment Scales across patient populations ensures that research data remains standardized, paving the way for breakthroughs and refined best practices.
The Stroke Assessment Scales guide many facets of stroke care, from immediate interventions to long-term management and research initiatives.
Benefits
Efficient patient care
Utilizing our Free Stroke Assessment Scales ensures swift and streamlined patient care, which is especially vital in emergencies where every second counts.
Evidence-based clinical decisions
Our Stroke Assessment Scales yield quantifiable scores, granting clinicians a comprehensive picture of a patient's condition. This clarity empowers them to make well-informed, evidence-based treatment choices.
Optimized patient outcomes
Individualized assessments from the Stroke Assessment Scales let you provide tailored treatments and management plans for modifiable risk factors. These insights significantly enhances patient recovery and long-term outcomes.
Uniformity in data collection
The standardized nature of these scales ensures a consistent data collection method. This is invaluable in medical research, allowing for easier data comparison and analysis across multiple studies and settings.
Facilitating continual medical advancements
By providing reliable, uniform data, Stroke Assessment Scales indirectly support the advancement of stroke treatment methodologies, promoting continual improvement in patient care.
Commonly asked questions
Medical professionals, especially neurologists and emergency room staff, use these scales to quickly assess and categorize stroke severity.
Primarily in the immediate aftermath of a suspected stroke, to guide treatment and predict outcomes.
You can use the scale through observing specific symptoms and assigning scores based on set criteria.. The summed scores then guide further action.

.jpg)


















-template.jpg)