No. The Parkinson’s Rigidity Test only checks if the patient has rigidity in their upper and lower extremities, which is a symptom of Parkinson’s Disease. It’s not enough to give you the full picture of the patient.
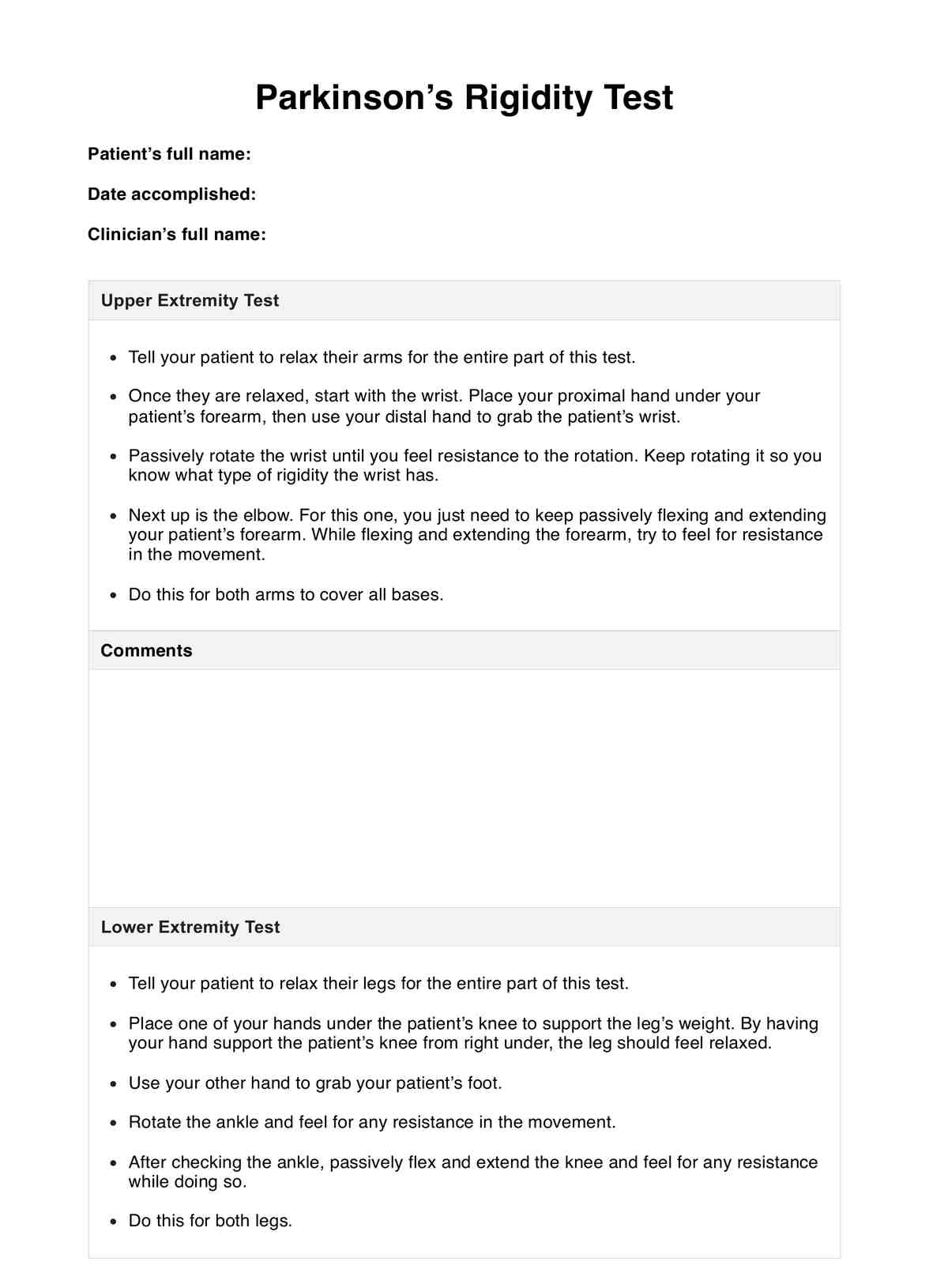
Parkinson’s Rigidity Test
If your patient is suspected of having Parkinson’s Disease, one of the things you need to do is check for specific rigidity symptoms. Conduct the Parkinson’s Rigidity Test to effectively gauge the rigidity of your patient’s limbs.
Parkinson’s Rigidity Test Template
Commonly asked questions
You should conduct tests that check for Bradykinesia, tremors, gait, and balance. It’s best to do these before conducting scans and neurological tests.
There are different ways to look at this. 1) They are not symptomatic of Parkinson’s Disease; 2) You’re conducting this for a routine check-up and their medicine is working; 3) The rigidity might be there, but rotation, flexing, and extending the limb won’t do the trick, so, the activation method we mentioned earlier might do the trick.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











