Modified Rankin Scale (mRS)
If you are dealing with a patient who had a stroke or some other neurological injury, you can use the Modified Rankin Scale (mRS) to assess their functional status! Learn more about the scale through this guide.


What is the Modified Rankin Scale (mRS)?
When a person, unfortunately, suffers from a stroke or another type of neurological problem, their functional status is impacted to varying degrees. Some are only mildly affected, and some are so horribly impacted they can't do what they usually do. To help assess the functional status of such people, the was developed.
The Modified Rankin Scale (mRS) specifically assesses the severity of their disability by checking if they can perform their daily living activities (ADLs) and other activities they usually do. Can they still do their daily activities and other things independently? Can they still do them, but they need assistance from others? Or can they no longer do them and require someone to do things for them?
The answers to these questions will help determine the patient's specific score on the Modified Rankin Scale, which will be discussed later in this guide.
The score will determine the contents of a person's care plan, and the scale can be used to monitor the patient periodically.
This is a valuable tool for neurologists, therapists (physical and occupational), and nurses handling stroke patients or others requiring constant nursing care.
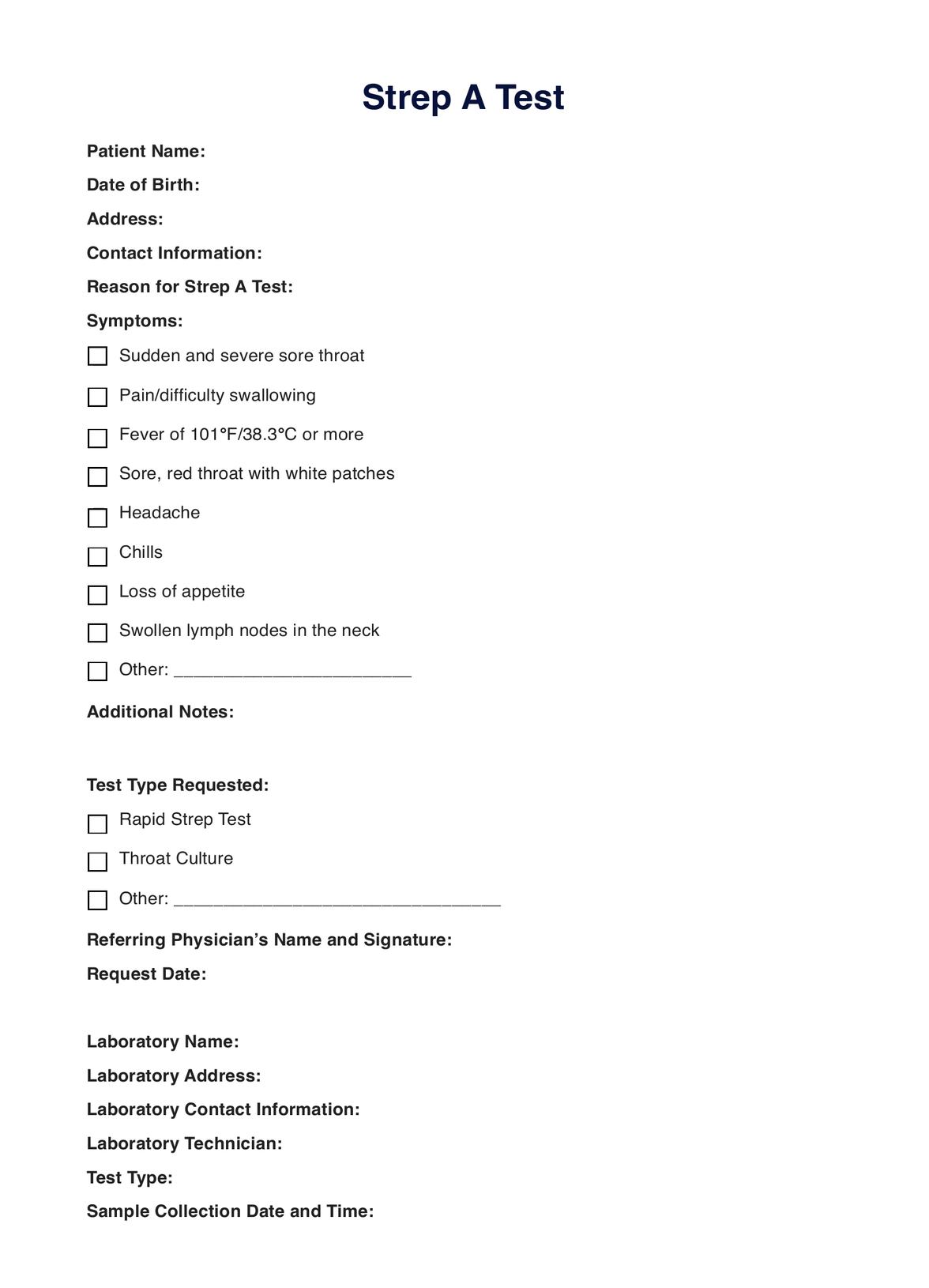
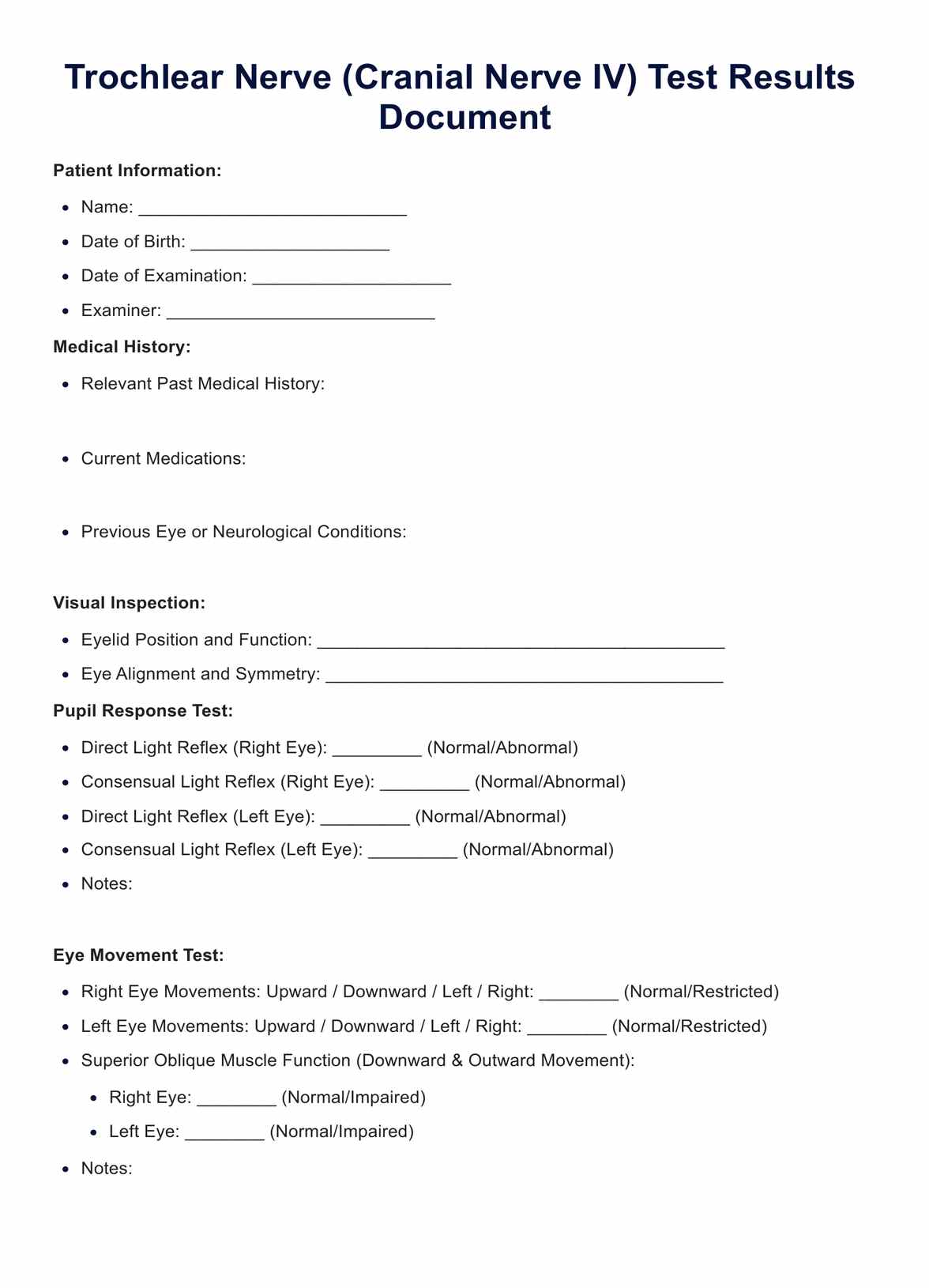
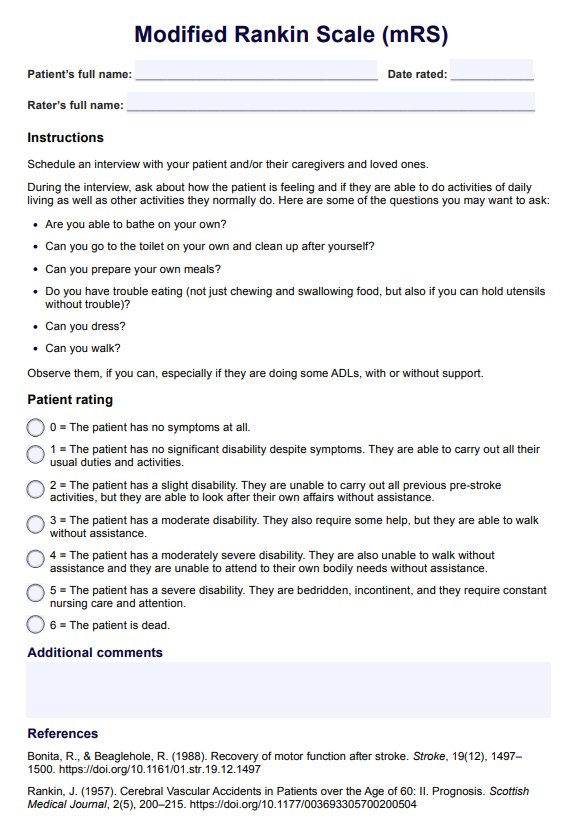
Modified Rankin Scale (mRS) Template
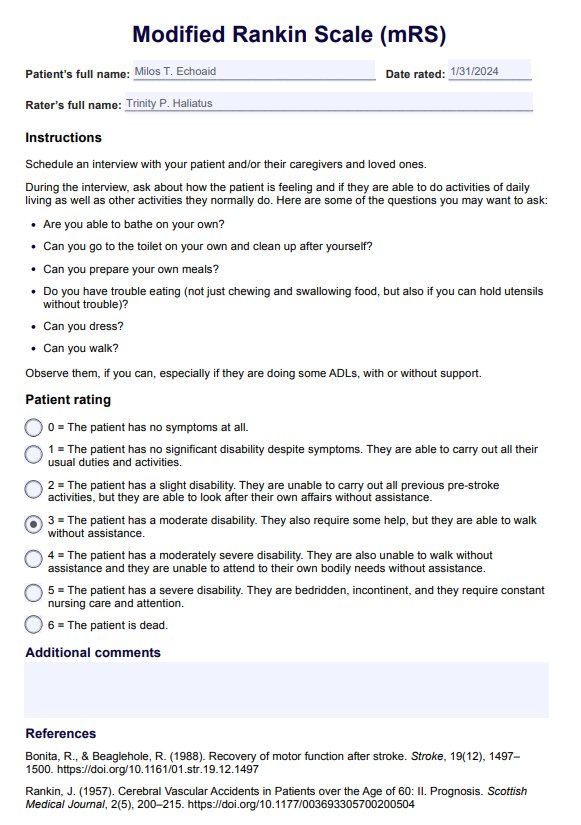
Modified Rankin Scale (mRS) Example
How to use the Modified Rankin Scale (mRS)
The Modified Rankin Scale (mRS) is an easy-to-use outcome measure. It requires little from the professional; the only thing that needs to be done when engaging with the sheet is to select a number rating.
Before selecting a rating, the professional must schedule an interview with the patient who suffered a stroke or a neurological problem. During the interview, the professional will ask the patient a series of questions related to how they are feeling and whether they can perform activities of daily living. You should also observe some of them, too, if you can.
Here are some questions that you can ask them:
- Are you able to bathe on your own?
- Can you go to the toilet on your own and clean up after yourself?
- Can you prepare your own meals?
- Do you have trouble eating (not just chewing and swallowing food, but also if you can hold utensils without trouble)?
- Can you dress?
- Can you walk?
You can tweak the questions to ascertain if they can do these things but require the aid of something or someone or if they can't do certain things at all.
Ask them about other activities they do that are not necessarily activities of daily living, such as their hobbies and recreational activities. If they have difficulty communicating, you may have a caregiver or companion who supports them daily to help them answer for you.
Once you get all the necessary information, you can rate their functional outcome using the scale.
How to score the Modified Rankin Scale (mRS)
The Modified Rankin Scale (mRS) is easy to score because you don't need to calculate anything. The score options are already set, and you only have to pick one out of seven possible scores. The scores also have set descriptions, so you will know where your patient falls based on your interview with them.
Here are the modified Rankin score options:
- 0 = The patient has no symptoms at all.
- 1 = The patient has no significant disability despite symptoms. They can carry out all their usual duties and activities.
- 2 = The patient has a slight disability. They are unable to carry out all previous pre-stroke activities, but they can look after their own affairs without assistance.
- 3 = The patient has a moderate disability. They also require some help, but they are able to walk without assistance.
- 4 = The patient has a moderately severe disability. They are also unable to walk without assistance and attend to their own bodily needs without assistance.
- 5 = The patient has a severe disability. They are bedridden and incontinent, and they require constant nursing care and attention.
- 6 = The patient is dead.
The mRS score you assign should help you and your team determine what goes into the patient's care plan.
What are the benefits of the Modified Rankin Scale (mRS)?
Saves time
If you and your team are part of a busy hospital and you have a lot of patients to look after, then you will love this tool because you aren't really required to do much when you engage with it—you just pick a single number as your patient's functional status score. While it may take a few minutes to an hour to interview your patient and observe them, it should only take you between one to five minutes to accomplish the scale, with no unnecessary calculations.
Helps educate a patient's family and friends.
The scale primarily focuses on the patient's disabilities and whether they can carry out their activities of daily living as well as other things that they normally do. This is also the key concern of the patient, their loved ones, and their friends. By using this scale, the rating you give will help all of them understand the patient's functional status and what kind of support they need.
The Additional comments box is here to help with that because it can serve as your opportunity to elaborate on things that the patient, their loved ones, and friends need to know.
Guides treatment planning, implementation, and monitoring
The Modified Rankin Scale (mRS), specifically the rating you selected for the patient, will help guide the treatment plan. Through the rating and the additional comments box, you can communicate the relevant information with your team, the patient, and the patient's loved ones.
Other members of your team can conduct the tests that they feel are important regarding the aspects of the person that their neurological condition has impacted. Then, based on the results, they can determine what should go into the patient's care plan.
Physical therapists on your team can conduct routine physical therapy tests to help rehab whichever extremities have been affected. If they have slurred speech, speech therapists can play a role in the care plan to get them back to a state where they can speak again. These are just some kinds of treatment that can be included in a care plan!
Eventually, you can use this as a monitoring tool to assess the patient's recovery progress and how effective your team's care plan is.
Commonly asked questions
Yes, but it can be used to assess a patient with a different neurological disability, such as traumatic brain injury, cerebral palsy, multiple sclerosis, or problems caused by cerebral vascular accidents.
It depends on how you look at it. It can only take a second because you're simply picking a number. However, it can take you up to ten minutes if you take the time to weigh the information you got from interviewing your patient or the patient's companion and from observing the patient.
Considering the interview and the observation parts, the amount of time you will spend on both will vary from patient to patient. Just don't be surprised if it takes you an hour. You are dealing with a patient impacted by a neurological problem, after all.
That depends on your team's care plan. You can go with monthly, quarterly, every half-year, or annually. Weekly might not be the best way to go about it because you can expect that progress might take a while to show.





















-template.jpg)