The trochlear nerve test assesses the function of cranial nerve IV (CN IV), which innervates the superior oblique muscle of the eye. This test is crucial because the trochlear nerve, the only cranial nerve that emerges from the dorsal aspect of the brainstem (near the inferior colliculus), has the longest intracranial course. It plays a crucial role in controlling the eye's movement, particularly its ability to move downward and outward. The test helps diagnose conditions like trochlear nerve palsy and can provide insights into the health of other cranial nerves and the superior orbital fissure region.
The Trochlear Nerve Test
Explore the essentials of the Trochlear Nerve Test, the key for diagnosing eye movement disorders related to Cranial Nerve IV, and its role in ocular health.
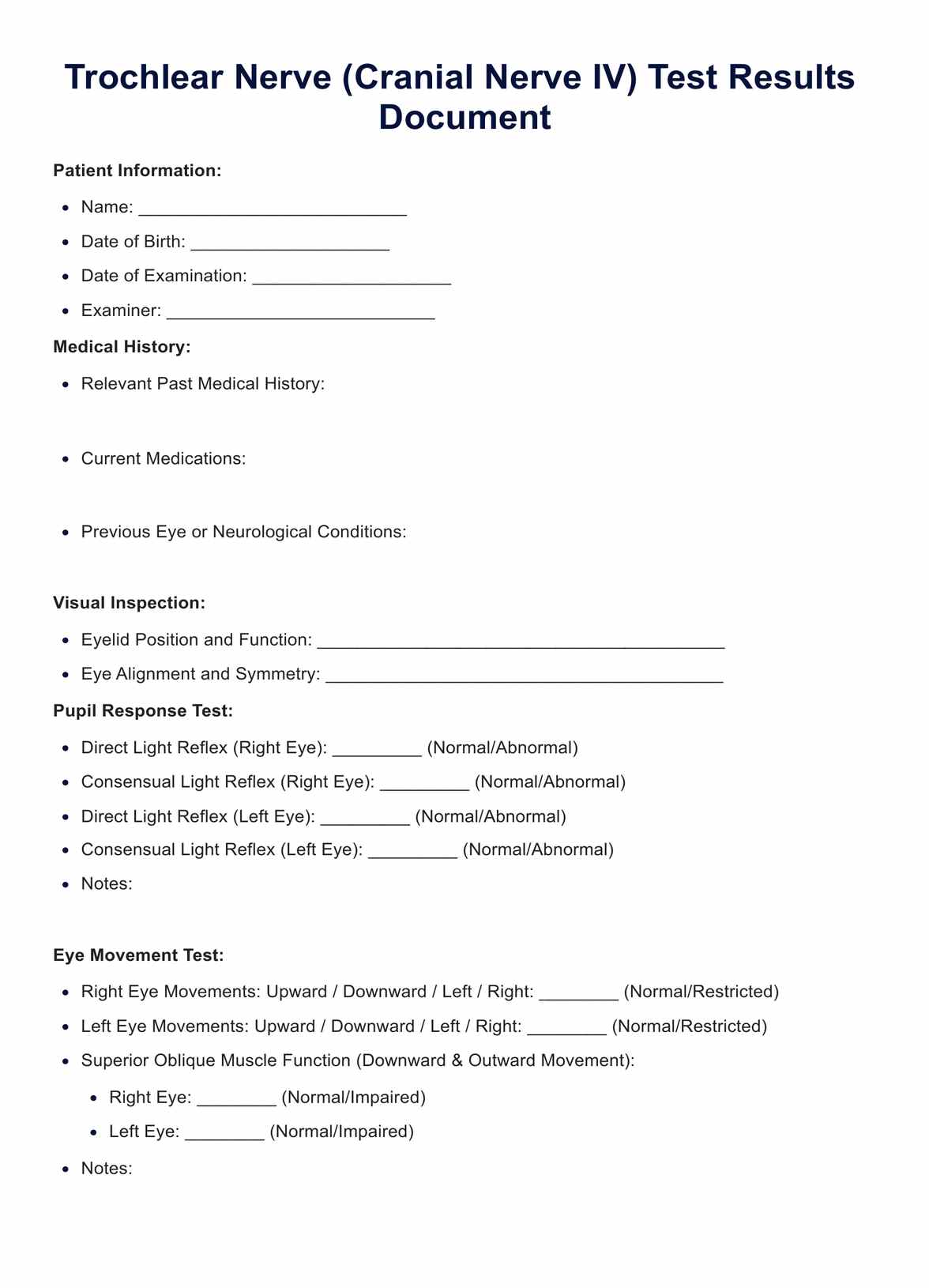
The Trochlear Nerve Test Template
Commonly asked questions
The trochlear nerve test is part of a broader examination of cranial nerves, especially those involved in eye movement, like the oculomotor (CN III) and abducens (CN VI) nerves. These nerves collectively control all extraocular muscles, ensuring coordinated eye movement. Abnormalities in the trochlear nerve test could indicate problems that might also affect the function of these other nerves and structures, like the cavernous sinus and superior orbital fissure.
Symptoms that might necessitate a trochlear nerve test include double vision (mainly vertical diplopia), difficulty moving the eye downward and outward, and a head tilt. These symptoms can arise from issues in the trochlear nucleus, the nerve's pathway, or its target muscle, the superior oblique. Conditions like acute vestibular syndrome, trauma affecting the middle cranial fossa, or issues in the lateral wall of the cavernous sinus can also prompt this test.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











