DSM 5 Criteria for Borderline Personality Disorder
Explore the DSM 5 Criteria for Borderline Personality Disorder. Understand BPD diagnosis and its impact on mental health professionals and patients.


What is borderline personality disorder (BPD)?
Borderline personality disorder (BPD) is a complex mental health condition characterized by a pervasive pattern of instability in moods, self-image, behavior, and relationships. Individuals with BPD may experience intense emotions, impulsive actions, and chronic feelings of emptiness, leading to difficulties in maintaining stable relationships and functioning in daily life, particularly in early adulthood.
What is the cause of borderline personality disorder?
The cause of BPD is not fully understood, but it is believed to be a combination of genetic, environmental, and neurobiological factors. Adverse childhood experiences, such as trauma, abuse, neglect, or post-traumatic stress disorder, are also associated with an increased risk of developing BPD.
What are the consequences of BPD?
The consequences and negative effects of BPD can be significant, impacting various aspects of an individual's life. People with BPD may struggle with emotional regulation, leading to intense and rapidly changing moods. They may also engage in self-destructive behaviors, such as substance abuse, self-harm, or suicidal ideation, as a way to cope with their emotional pain. Additionally, BPD can affect interpersonal relationships, causing instability and conflicts due to fears of abandonment and difficulties in trusting others.
Women with BPD often have co-occurring disorders like major depression, anxiety, substance abuse, or eating disorders. At the same time, men with BPD are more likely to have substance abuse or antisocial personality disorder. Understanding BPD is crucial for providing appropriate support and treatment to individuals affected by this disorder. Through this borderline personality disorder DSM 5 diagnostic criteria template, you can help diagnose patients and help them as they go through this condition.
DSM 5 Criteria for Borderline Personality Disorder Template
DSM 5 Criteria for Borderline Personality Disorder Example
How is BPD different from other personality disorders?
Borderline personality disorder (BPD) is one of several personality disorders, each with its unique set of characteristics. While there are similarities among personality disorders such as bipolar disorder and antisocial personality disorder, BPD has distinct features that set it apart:
- Emotional instability
- Fear of abandonment
- Unstable relationships
- Impulsivity
- Self-image issues
- Chronic feelings of emptiness
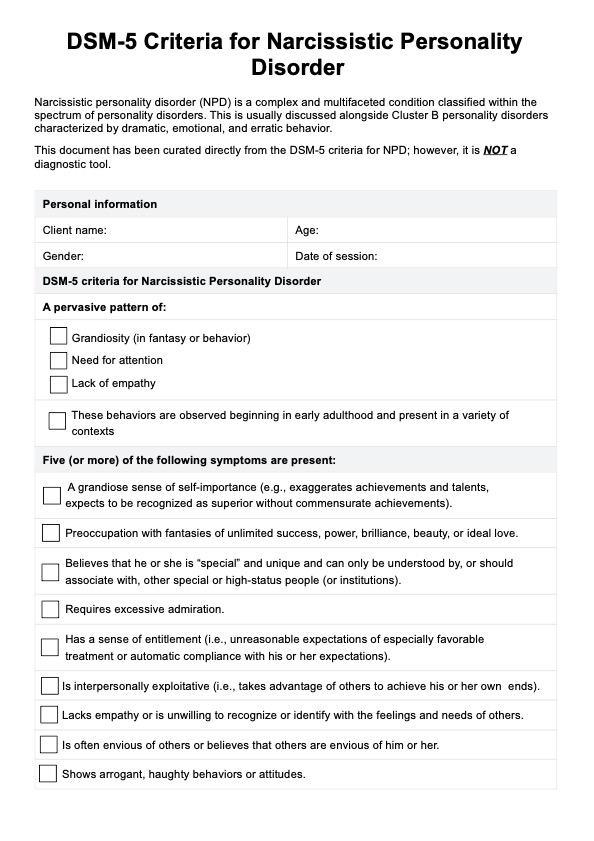
While other personality disorders, such as narcissistic personality disorder (NPD) or avoidant personality disorder (APD), may share some overlapping symptoms, the combination and intensity of symptoms in BPD are unique. For example, NPD is characterized by an inflated sense of self-importance and a lack of empathy, while APD involves a pervasive pattern of social inhibition and feelings of inadequacy. BPD, on the other hand, is primarily marked by emotional dysregulation and instability in interpersonal relationships.
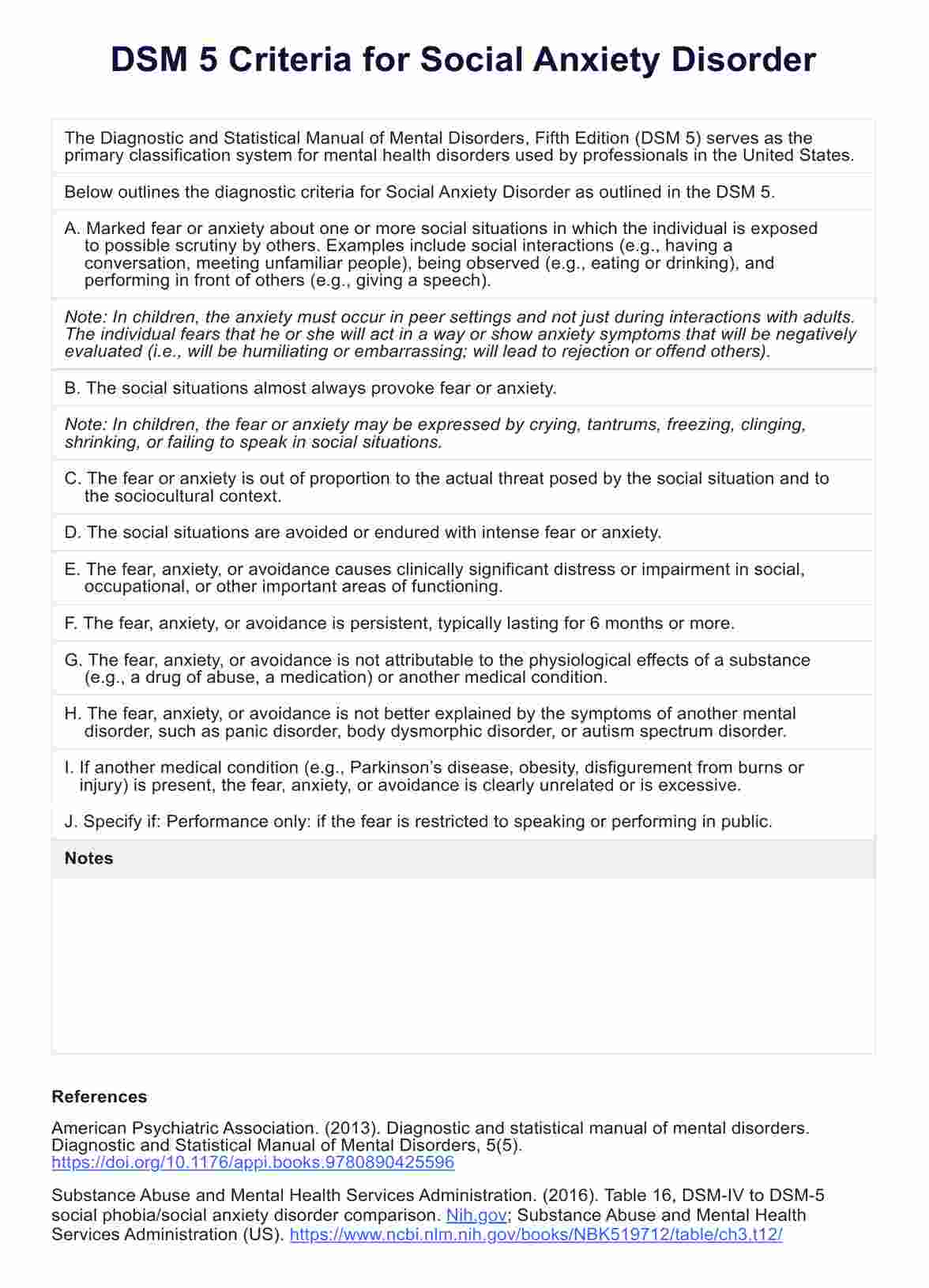
It is also important to differentiate BPD from other conditions, such as post-traumatic stress disorder and mood disorders, to ensure accurate diagnosis and effective treatment. Understanding the distinctions between BPD and other psychiatric disorders is crucial for accurate diagnosis and effective treatment. Each disorder requires a tailored approach to address the specific challenges and needs of the individual.
How is BPD diagnosed?
The diagnosis of BPD is a multi-step process that involves a comprehensive evaluation by a mental health professional.
What assessments are conducted?
First off, some assessments need to be done before BPD is diagnosed. Here's what you should expect:
- Clinical interview: A thorough clinical interview is the cornerstone of BPD diagnosis. The mental health professional will ask about symptoms, personal and family medical history, and the individual's functioning in various areas of life.
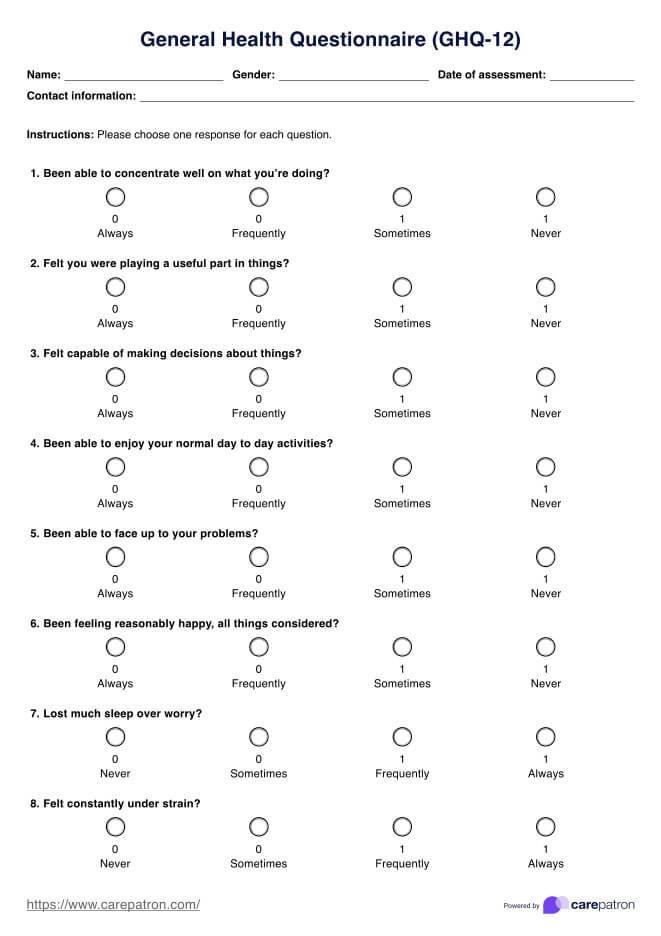
- Psychological assessment: Standardized psychological tests and questionnaires may be used to assess BPD symptoms and rule out other mental health conditions.
- Observation: The clinician may observe the individual's behavior and interaction patterns during the assessment process.
- Medical evaluation: Although there are no laboratory tests to diagnose BPD, a medical evaluation may be conducted to rule out other conditions contributing to the symptoms.
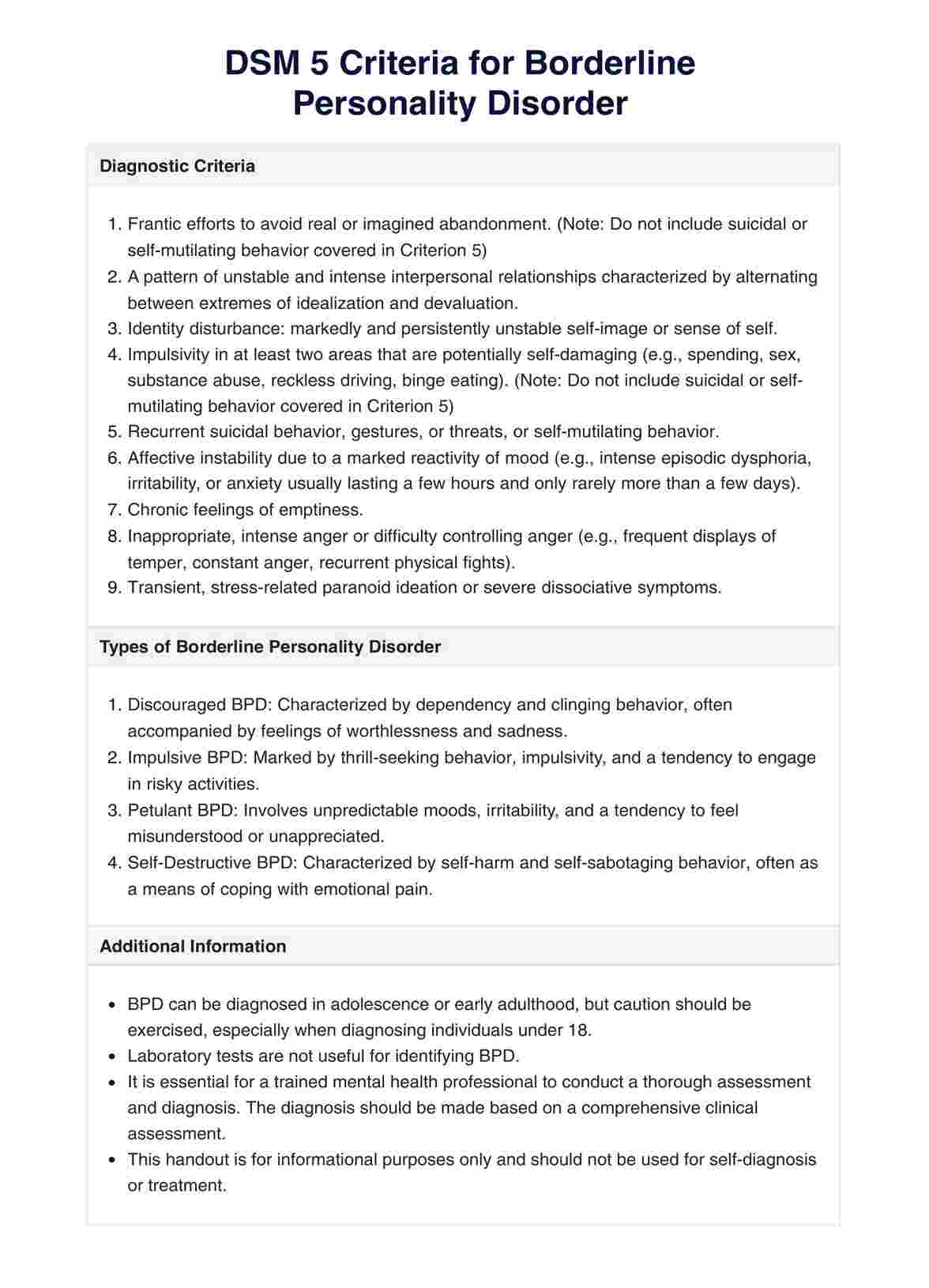
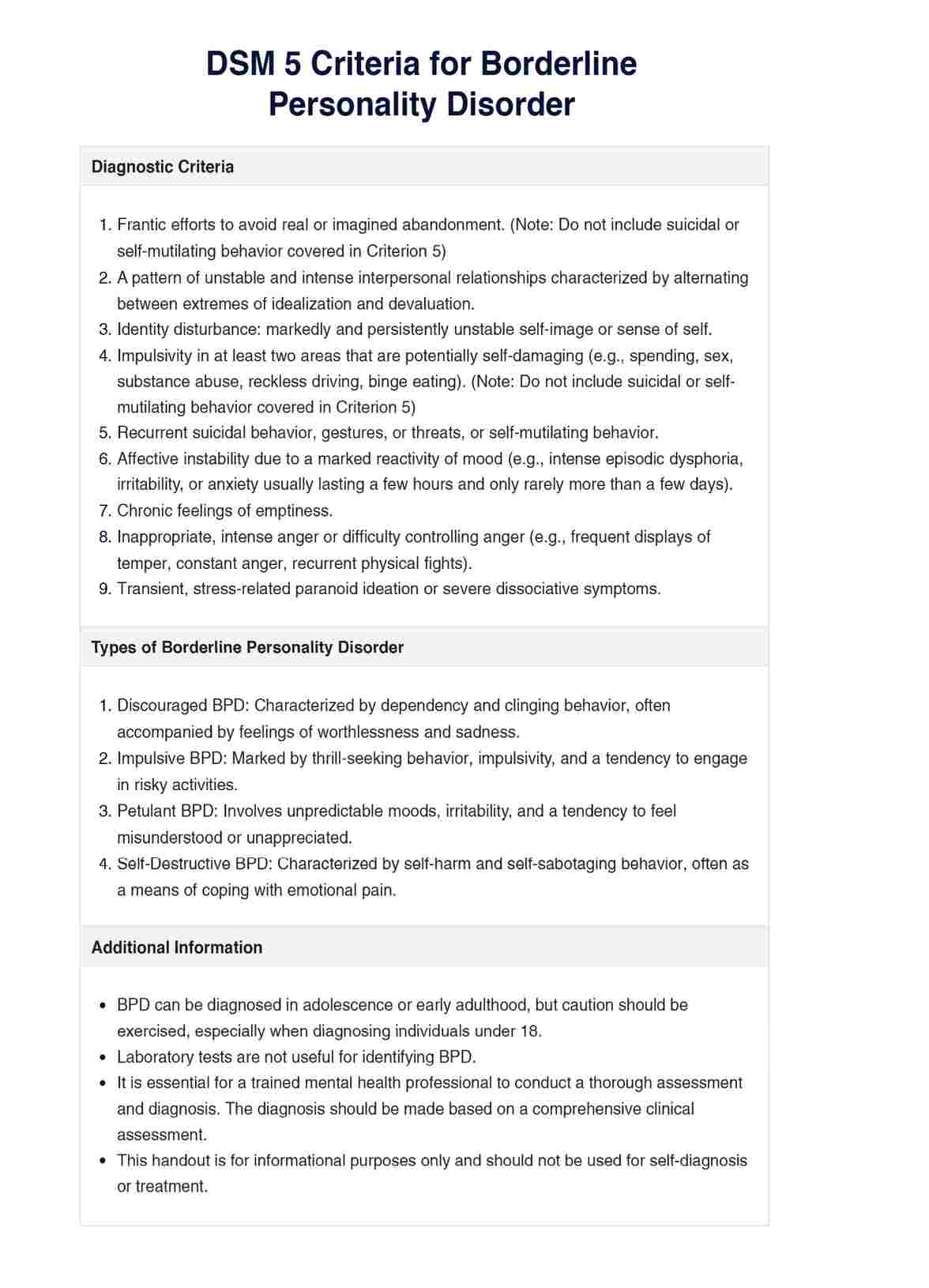
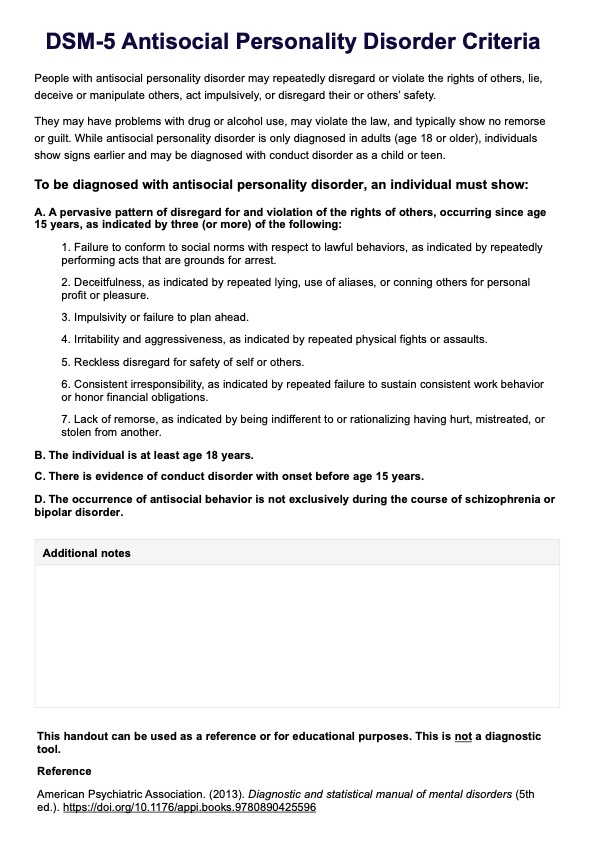
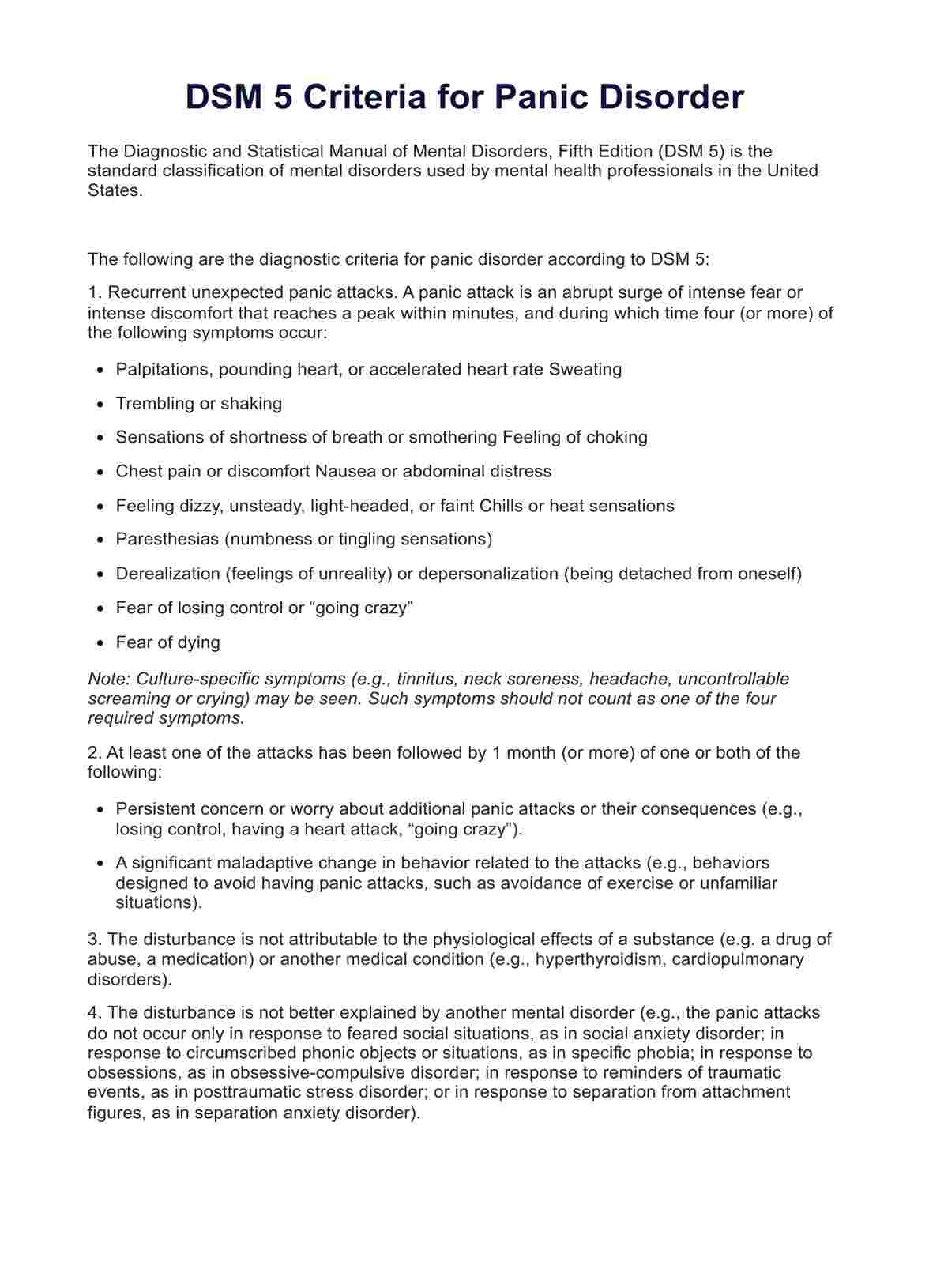
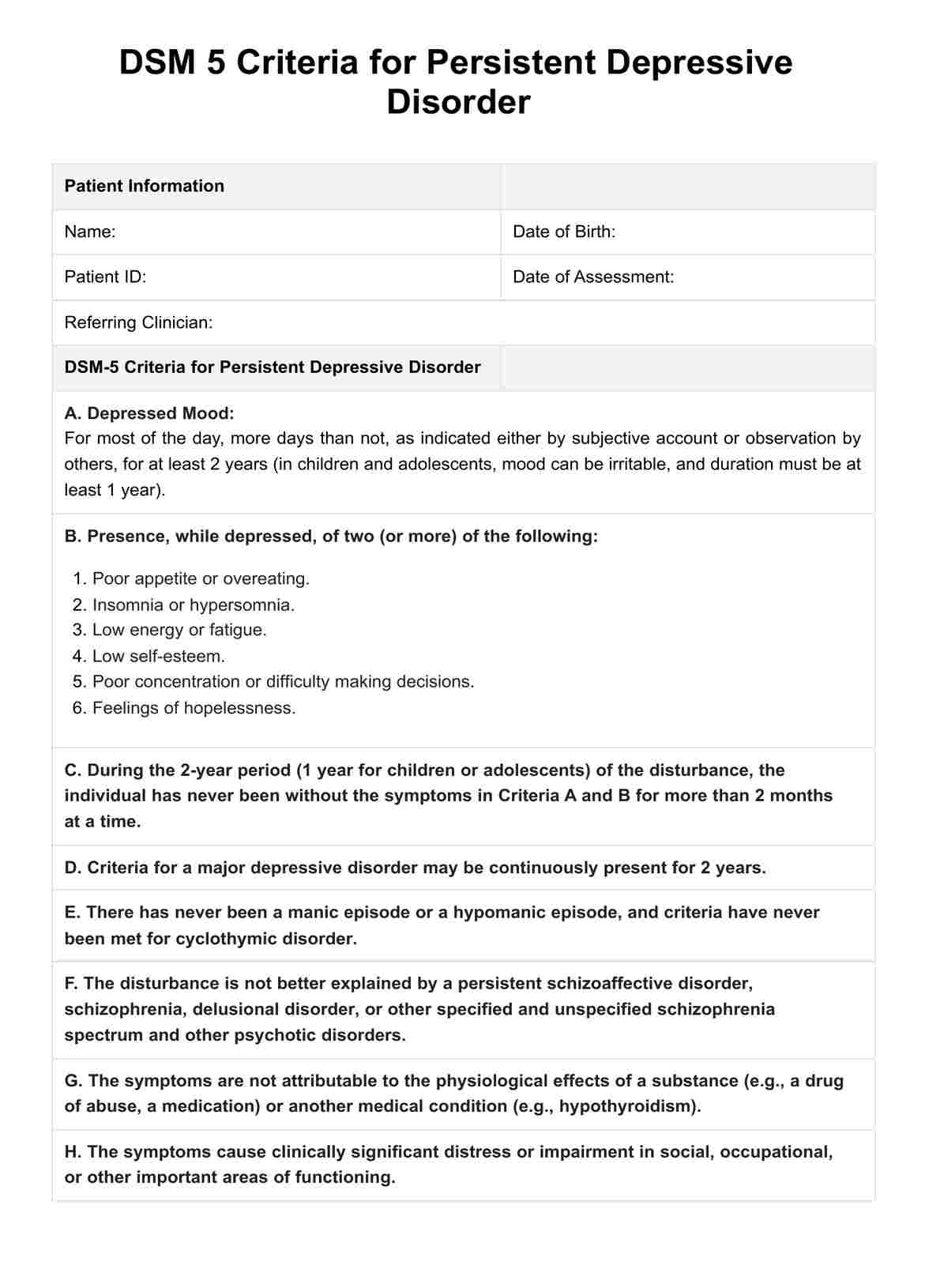
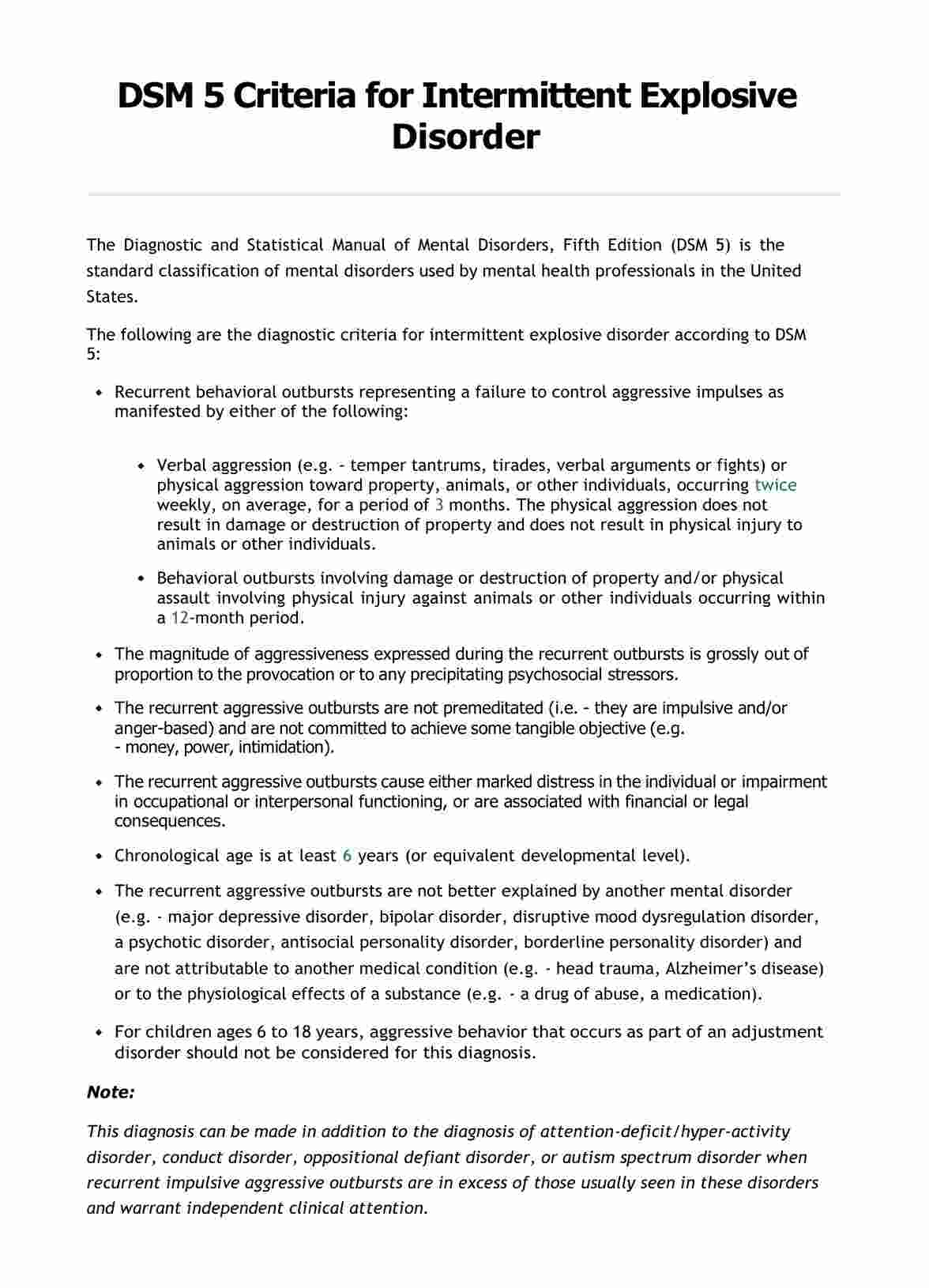
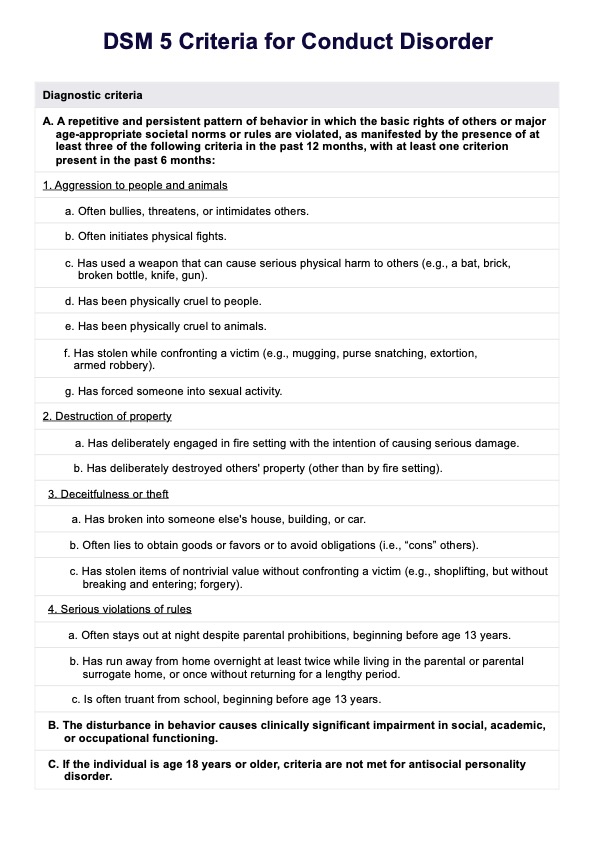
DSM 5 Criteria for Borderline Personality Disorder
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a comprehensive classification system for mental disorders. It is published by the American Psychiatric Association (APA) in 2013 and is widely used by mental health professionals in the United States and around the world. The DSM-5 serves as a guide for diagnosing mental disorders and provides standardized criteria to ensure consistency and accuracy in diagnosis.
The DSM-5 outlines the following criteria for diagnosing BPD:
- Frantic efforts to avoid real or imagined abandonment.
- A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization and devaluation.
- Identity disturbance: markedly and persistently unstable self-image or sense of self.
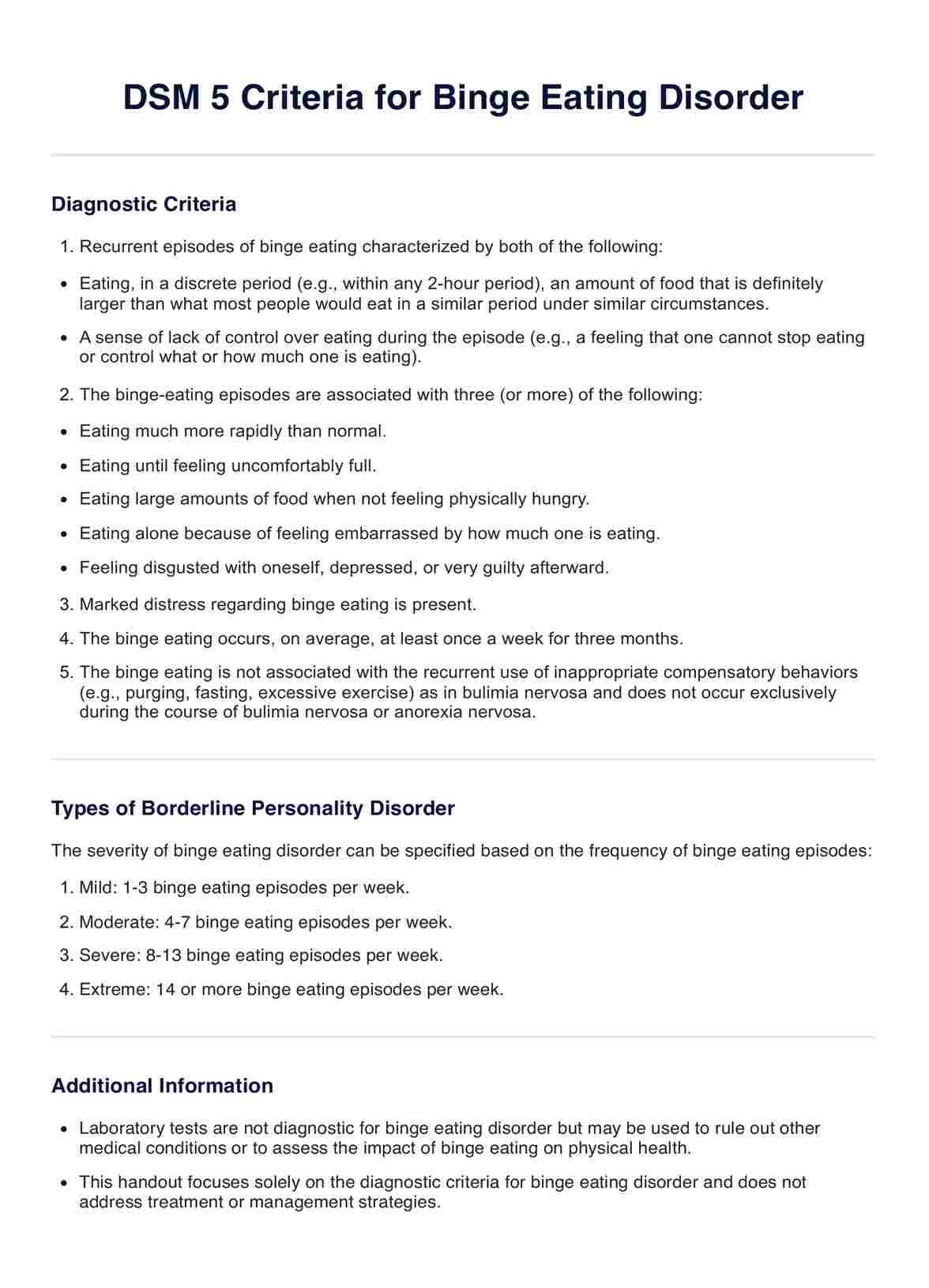
- Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating).
- Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior.
- Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days).
- Chronic feelings of emptiness.
- Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
- Transient, stress-related paranoid ideation or severe dissociative symptoms.
To be diagnosed with BPD, an individual must exhibit at least five of these criteria.
Are there differences between the DSM 4 and DSM 5 criteria for this?
The DSM has a long history, with the first edition published in 1952. Since then, it has undergone several revisions to reflect advances in our understanding of mental health. The most recent edition, DSM-5, was released in 2013 and introduced several significant changes, including reclassifying some disorders and adding new ones.
The criteria for BPD in the DSM-5 are largely consistent with those in the DSM-4. However, the DSM-5 provides more detailed descriptions and examples to clarify the criteria and improve diagnostic accuracy.
Treatments for BPD
Addressing Borderline Personality Disorder (BPD) requires a comprehensive approach that combines various therapeutic methods. Here are some key treatments for BPD:
Psychotherapy
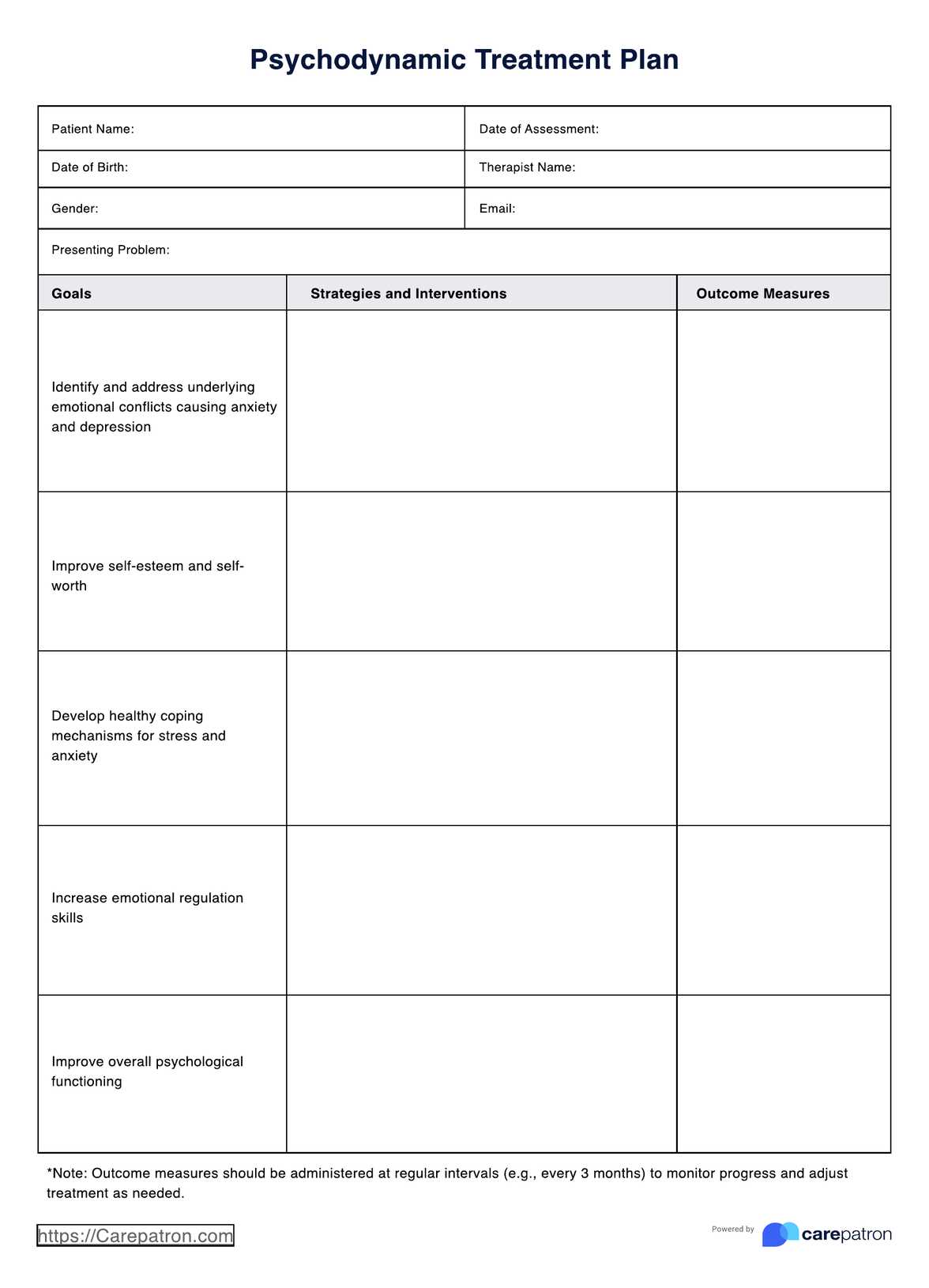
Psychotherapy is the cornerstone of BPD treatment, with several types being particularly effective:
- Dialectical behavior therapy (DBT): Developed specifically for BPD, DBT focuses on teaching skills to manage emotions, tolerate distress, and improve relationships.
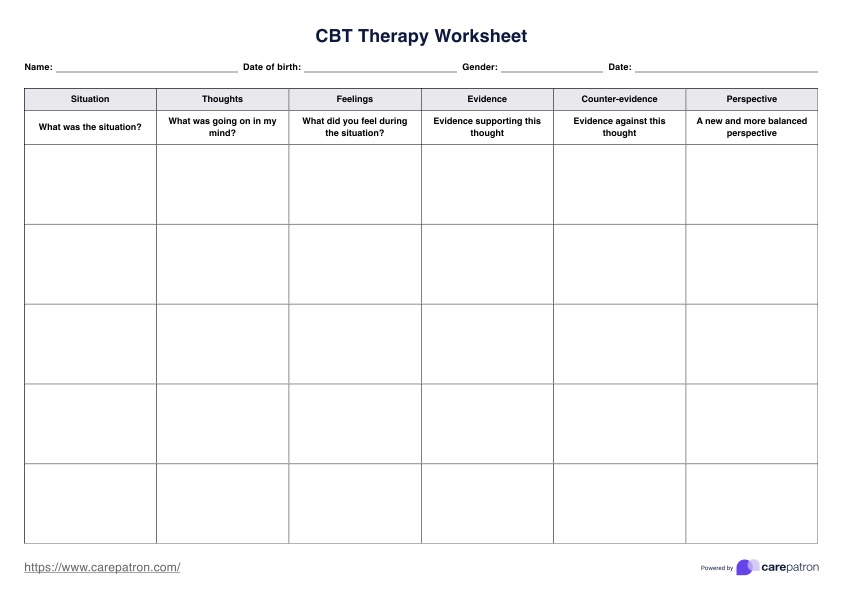
- Cognitive behavioral therapy (CBT): This therapy helps patients identify and change problematic thought patterns and behaviors.
- Schema therapy: This integrates elements of CBT, DBT, and other therapies to help patients understand and change long-standing life patterns.
- Mentalization-based therapy (MBT): MBT aims to improve the patient's ability to understand their own and others' mental states, which can be challenging for those with BPD.
Medication
While there are no medications specifically approved for BPD, certain medications can help manage symptoms or co-occurring disorders:
- Antidepressants: May help with mood swings, depression, or anxiety.
- Mood stabilizers: Can reduce impulsivity and mood instability.
- Antipsychotics: May be used to help with symptoms such as anger, paranoia, or transient psychotic episodes.
Group therapy
Group therapy provides a supportive environment where individuals can learn from others with similar experiences, practice social skills, and receive feedback.
Hospitalization
In severe cases, particularly when there's a risk of self-harm or suicide, short-term hospitalization may be necessary to ensure safety and stabilize the individual.
It's important for patients with borderline personality disorder to work closely with their healthcare providers to develop a personalized treatment plan that addresses their unique needs and symptoms.
Research on borderline personality disorder
Borderline personality disorder has been extensively documented in psychiatric literature, leading to the creation of standardized diagnostic manuals like the DSM. However, recent groundbreaking research continues to shed light on the complex nature of this disorder. Here are some highlights from recent studies:
Rejection distress in BPD
A study led by Eric Fertuck from The City College of New York, Columbia University, and the New York State Psychiatric Institute identified a unique brain response to social rejection in individuals with BPD. The research found that the rostro-medial prefrontal cortex, a region typically active during rejection, remains inactive in those with BPD.
This may explain the heightened sensitivity and distress to rejection experienced by individuals with this disorder. The findings have significant implications for improving diagnosis and developing more effective therapies for BPD (Fertuck et al., 2022).
Stress reactivity, generation, and chronic feelings of emptiness in BPD
Research by Allen et al. (2020) explored the relationship between stress and BPD by examining the roles of negative affect, antagonism, and disinhibition. The study discovered that antagonism and disinhibition, in particular, are key features that drive the generation of stressors resulting from individual choices or behaviors in people with BPD. This insight into the distinct features of BPD can help tailor interventions to reduce the stress-related burden in affected individuals.
These studies represent just a fraction of the ongoing research efforts to understand and treat borderline personality disorder. By continually exploring the biological, psychological, and social facets of BPD, researchers hope to improve the lives of those affected by this challenging condition.
References
Allen, T. A., Dombrovski, A. Y., Soloff, P. H., & Hallquist, M. N. (2020). Borderline personality disorder: Stress reactivity or stress generation? A prospective dimensional study. Psychological Medicine, 1–8. https://doi.org/10.1017/s003329172000255x
American Psychiatric Association. (2013a). Diagnostic and statistical manual of mental disorders (5th ed.). Pearson.
Fertuck, E. A., Stanley, B., Kleshchova, O., Mann, J. J., Hirsch, J., Ochsner, K., Pilkonis, P., Erbe, J., & Grinband, J. (2022). Rejection distress suppresses medial prefrontal cortex in borderline personality disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging8(6), 651–659. PubMed. https://doi.org/10.1016/j.bpsc.2022.11.006
Commonly asked questions
The 9 symptoms of BPD include fear of abandonment, unstable relationships, unclear or shifting self-image, impulsive and self-destructive behaviors, self-harm, extreme emotional swings, chronic feelings of emptiness, explosive anger, and feeling suspicious or out of touch with reality.
The 4 types of BPD are discouraged BPD, impulsive BPD, petulant BPD, and self-destructive BPD. Individuals can experience more than one type simultaneously or at different stages in their lives.
BPD can have a significant impact on an individual's life, leading to unstable relationships, emotional instability, impulsive behavior, and difficulties with self-image. It can also result in challenges in employment, social interactions, and overall quality of life.



















-template.jpg)